
Authorized Agent - Broker
Get Instant Quotes
UHC United Health Employer Small Business Group Health Plans
UHC administer your benefits
United Health Care Employer eServices
Manage group benefits in Employer eServices®
- Employer eServices provides a suite of tools to simplify health plan management for employers.
- Receive eligibility updates
- Pay invoices
- Check out wellness tips and more
- uhc.com/employer/california get forms & brochures
- Improved employee experience – digital
- Uhceservices.com Reference Guide for Employers
- Plan documents and forms have now been consolidated on uhceservices.com
- look for the Resources menu in the top navigation to view and download up-to-date forms, product grids, benefit summaries/SBCs and other documents. Existing users of uhceservices.com can use their same One Healthcare ID to sign in.
New users can create a new account using the instructions available on the uhceservices.com homepage. - Sign in to Employer eServices
- This resource center provides enhanced support for medical benefits administration.
- Look up plan benefit information
- Manage eligibility
- Get health plan ID cards for members

- Sign In to UHCServices.com
-
Who to #Contact
-
- Employer Contact Sheet 12.2019
- Client Services Operations 1.800.591.9911 (Urgent Matters)
- client service [email protected]
- [email protected]
- Employer Contact Sheet 12.2019
Customer Support 1-800-651-5465 ♦ 1-866-336-9369
Website Demo
Tutorial
- View the tutorial →
- Guided Tour
- If you can’t get the demo’s to run, here’s UHC’s response:
- Please make sure for eServices site that ad or pop up blockers are disabled. If the issue persists please contact 1-800-651-5465 for eServices technical support.
- Uhceservices.com Reference Guide for Employers
- If you can’t get the demo’s to run, here’s UHC’s response:
-
- This resource center provides enhanced support for medical benefits administration.
Jump to section on:
- Wellness
- Contact Info
- Participation Audit
- For NEW business, see our main UHP page.
- UHC Websites
- Forms & brochures
- How to enroll new employees
#Enrollment Options UHP
Three (Four) different ways to enroll new employees
4th way - just email us the application * [email protected]
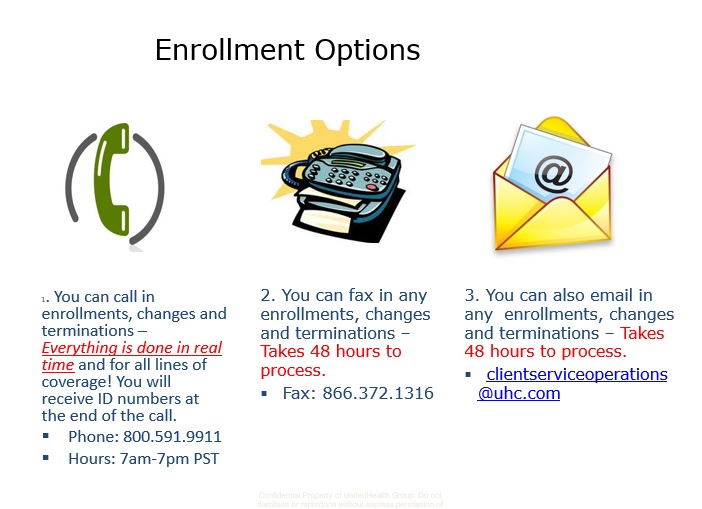
Try this number too (800) 624-8822
- Question How do we terminate an employee? What COBRA or Cal COBRA forms do we have to give the former employee? Our group is under 20 lives.
- Answer See the links above, navigate to and download the Employer Group Reporting (Termination) Form
- You can always email us and we will send it to you, for example, if the form gets updated and you have trouble finding it.
- Here's our webpage on Cal COBRA. The employee has the right to continue on the group plan for 3 years, but pays a 10% premium for doing so.
- He can also get guaranteed issue ACA/Obamacare. He can get quotes and enroll here. Note also that in general, all companies automatically send a Cal COBRA package to the terminated employee. Thus the termination form is the ONLY one needed.
- Form to notify UHC of a COBRA event.
- See pages 5 & 6 of the employer administration manual for more detail. I'm double checking to see if there is a more recent version.
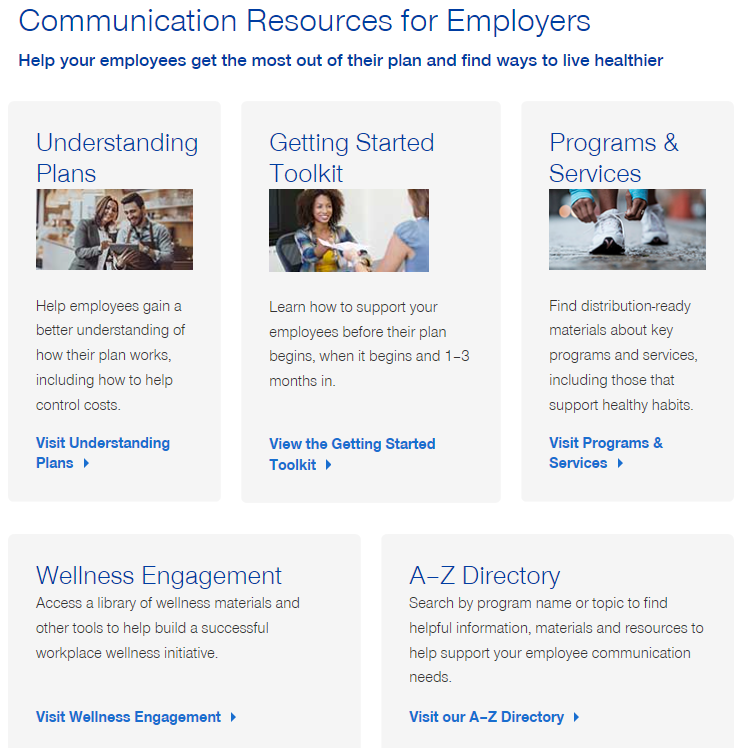
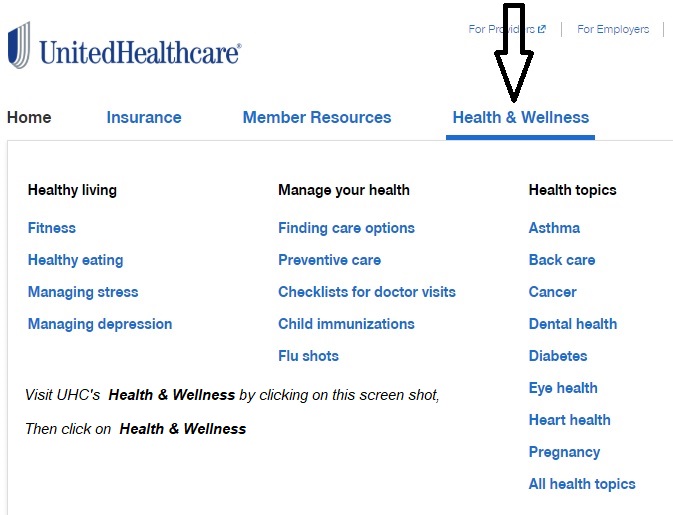
UHC #Wellness Engagement
health topics and articles
Employer Group
- Individuals
UHC Wellness Employer & Member Materials
- COVID-19 – UnitedHealthcare:
- Employer FAQs
- Broker FAQs
- Our main webpage on COVID
Cafe Well Video
Wellness Programs
Get rewarded for going to the Gym
Weight Loss
Health Coverage #Guide
Art Gallagher
Health Care Reform FAQ's
Understanding Health Reform
***********************************
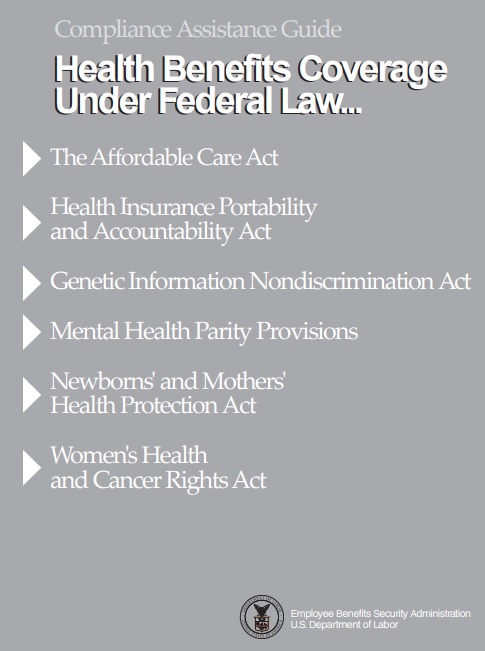
Compliance #Assistance Guide from DOL.Gov Health Benefits under Federal Law
- Health Care Reform Explained Kaiser Foundation Cartoon VIDEO
- Choosing a Health Plan for Your Small Business VIDEO DOL.gov
- ACA Quick Reference Guide California Small Group Employers Revision 2020 Word & Brown
- kff.org/health-policy-101/
Health Insurance unfortunately is very complicated
President Trump February 27, 2017
- Thus, if we haven't simplified and explained in PLAIN ENGLISH what you are looking for:
UHC United Health Care
#Participation Audit
Do you have a high enough percentage of employees covered?
Are you a bonified business?
- Our UHC – United Health Care Administrative Page
- UHC's Web Page on Eligibility Verification
- Our Webpage on Common Ownership -
- UHC Common Ownership Certification Form
- Employer Information Form UCH
- Our Webpage on Common Ownership -
- UHC's Web Page on Eligibility Verification
Questions about your Eligibility Audit?
Broker ONLY Portal
- uhc eservices
- employer e services.com
- Uhceservices.com Reference Guide for Brokers
- UnitedHealthcare agents and brokers
- Warner Pacific Carrier 411
- uhc e services.com/marketing-materials
- uhc e services.com emp eng planner/view all topics
- Product Grids and Network Documents
- Benefit Summaries & SBCs
- Broker ONLYE Services training Video
- Uhceservices.com Reference Guide for Brokers
- uhc.com/agents-brokers/news-strategies



https://www.uhc.com/find-a-doctor
https://www.uhc.com/agents-brokers/employer-sponsored-plans/news-strategies/cost-and-utilization-reporting-update-july-2025
I cant find where to terminate my policy, both with UHC and my bank ACH
I was given what to include to cancel, but I can’t find it anywhere where I was told to go to after ‘ [email protected].’
That email address is the place to go. It shows in the UHC Contact Sheet.
Here’s instructions from CFPB Consumer Financial Protection Bureau
If you cancel your coverage, with UHC rather than just stop paying, you may be able to get back premiums.
UHC keeping sending me late notices when I’m not late, even the same day they send a bill. They cite AB 2470. What’s up with that?
Well I see that I had looked AB 2470 up some time earlier and it says in part, there must be 30 day notice for cancellation.
So, if one gets a bill for October 1 and doesn’t pay it, they will be cancelled October 31st. So to comply, the Insurance Company must send the bill 30 days ahead of the cancellation day, which is practically the day they send the October bill!
Here’s Blue Cross’s explanation
Ca state law requires we send reminder notice to anyone who has not paid by the due date. We run a report around 25th of the month and mail out the letters by the 27th to anyone who has not paid for the invoice that generated on the 1st of the month (example June invoice generates on 5/1 so on 5/25 if you have not paid June yet we will send this letter on the 27th).
This is just a reminder notice and its required by law so that is why we have to use certain language. I know some find it threatening but it’s just a reminder and not a threat to cancel you actually have until 6/30 to make the payment. I hope that helps explain.
See the UHC Administrative Manual and Premium Direct Debit Program above on how to do that.