Administer your benefits

Authorized Agent - Broker UnitedHealthcare
Get Instant Quotes
UnitedHealthcare Employer Small Business Group Health Plans
UnitedHealthcare Employer eServices
Manage group benefits in Employer eServices®
- Employer eServices provides a suite of tools to simplify health plan management for employers.
- Receive eligibility updates
- Pay invoices
- Check out wellness tips and more
- uhc.com/employer/california get forms & brochures
- Improved employee experience – digital
- Uhceservices.com Reference Guide for Employers
- Plan documents and forms have now been consolidated on uhceservices.com
- look for the Resources menu in the top navigation to view and download up-to-date forms, product grids, benefit summaries/SBCs and other documents. Existing users of uhceservices.com can use their same One Healthcare ID to sign in.
New users can create a new account using the instructions available on the uhceservices.com homepage. -
Important documents
On this page you’ll find samples of the following important medical plan documents. Please use the information here as a general reference.Sample Certificates of Coverage
Prior Authorization Guides Why UHC.com *
- look for the Resources menu in the top navigation to view and download up-to-date forms, product grids, benefit summaries/SBCs and other documents. Existing users of uhceservices.com can use their same One Healthcare ID to sign in.
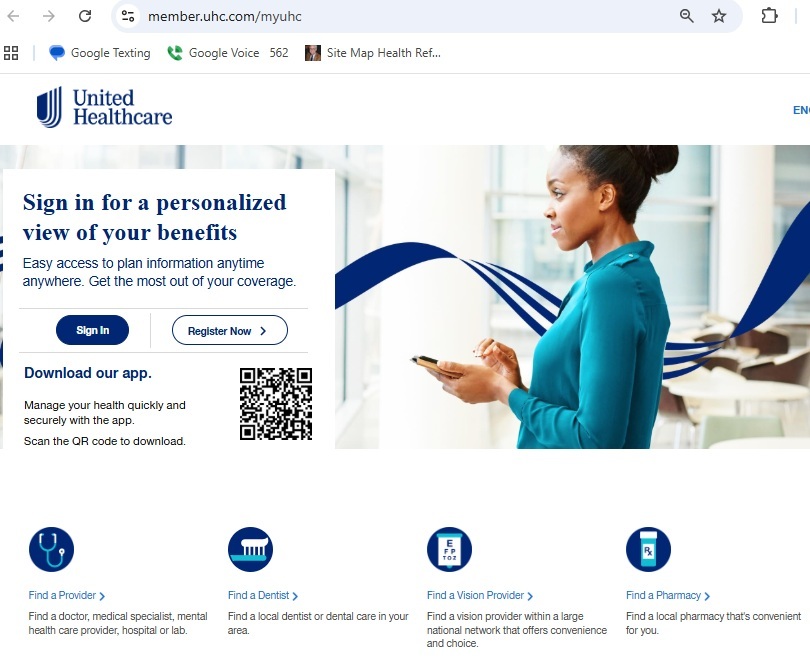
- Sign in to Employer eServices
- This resource center provides enhanced support for medical benefits administration.
- Look up plan benefit information
- Manage eligibility
- Get health plan ID cards for members

- Sign In to UHCServices.com
-
Who to #Contact
-
- Employer Contact Sheet 8/2022 UHC Flyer
- Client Services Operations 1.800.591.9911 (Urgent Matters)
- client service [email protected]
- [email protected]
- Employer Contact Sheet 8/2022 UHC Flyer
Customer Support 1-800-651-5465 ♦ 1-866-336-9369
Website Demo
Tutorial
- View the tutorial →
- Guided Tour
- If you can’t get the demo’s to run, here’s UHC’s response:
- Please make sure for eServices site that ad or pop up blockers are disabled. If the issue persists please contact 1-800-651-5465 for eServices technical support.
- Uhceservices.com Reference Guide for Employers
- If you can’t get the demo’s to run, here’s UHC’s response:
-
- This resource center provides enhanced support for medical benefits administration.
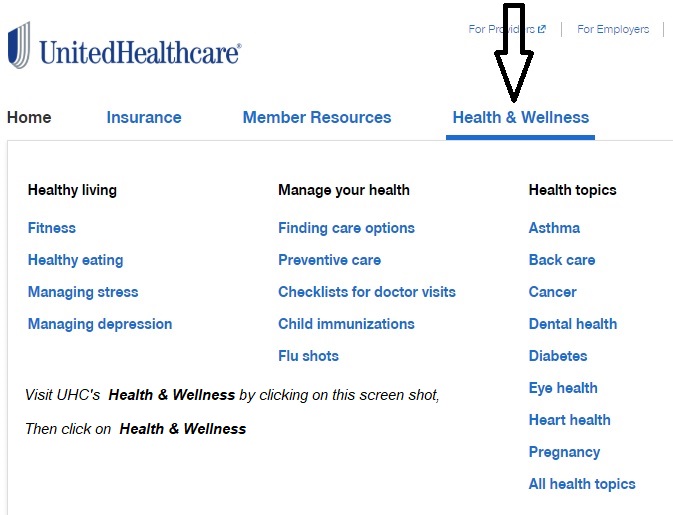
My UHC.com
- My UHC.com
- Welcome to what care can do These health and wellness benefits are available as part of your health plan — at no additional cost to you. UHC Flyer
- 24/7 Virtual Care No Co Pay Zero dollars UHC Flyer
- A freestanding facility1 is an outpatient, diagnostic or ambulatory center or independent laboratory which performs services and submits claims as a freestanding entity and not as a hospital. You will have a lower co-payment or no co-payment2 when you use a freestanding network facility instead of a hospital for outpatient services. Outpatient services are health services or treatments that do not require an overnight hospital stay. Flyer
- Digital tools to keep you connected Smart Phone Apps UHC Flyer * UHC Flyer
- Important things to know about selecting your PCP A primary care provider (PCP) is your health guide — someone who can help coordinate your care and supports you in achieving your best health. UHC Flyer
- Choosing a network physician just got simpler. Finding a doctor, specialist or facility couldn’t be easier. Just follow the steps below. UHC Flyer
- A focus on primary care and the patient-doctor relationship for better access to quality, efficient care. flyer
- UnitedHealthcare Rewards is a program where employees and their spouses can earn up to $1,000 for reaching program goals and completing one-time activities. Participants can personalize their experience by selecting activities that are right for them — and same goes for ways to spend earnings. Flyer
- Preventative Care flyer
- Nurse Line flyer
Jump to section on:
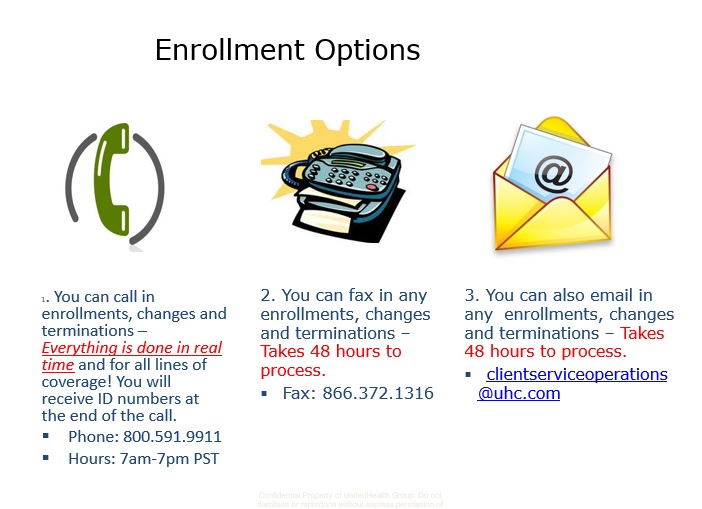
#Enrollment Options UHP
Three (Four) different ways to enroll new employees
4th way - just email us the application * [email protected]
Find a provider - PCP Primary Care Physician
Try this number too (800) 624-8822
- Question How do we terminate an employee? What COBRA or Cal COBRA forms do we have to give the former employee? Our group is under 20 lives.
- Answer See the links above, navigate to and download the Employer Group Reporting (Termination) Form
- You can always email us and we will send it to you, for example, if the form gets updated and you have trouble finding it.
- Here's our webpage on Cal COBRA. The employee has the right to continue on the group plan for 3 years, but pays a 10% premium for doing so.
- He can also get guaranteed issue ACA/Obamacare. He can get quotes and enroll here. Note also that in general, all companies automatically send a Cal COBRA package to the terminated employee. Thus the termination form is the ONLY one needed.
- Form to notify UnitedHealthcare of a COBRA event.
- See pages 5 & 6 of the employer administration manual for more detail. I'm double checking to see if there is a more recent version.
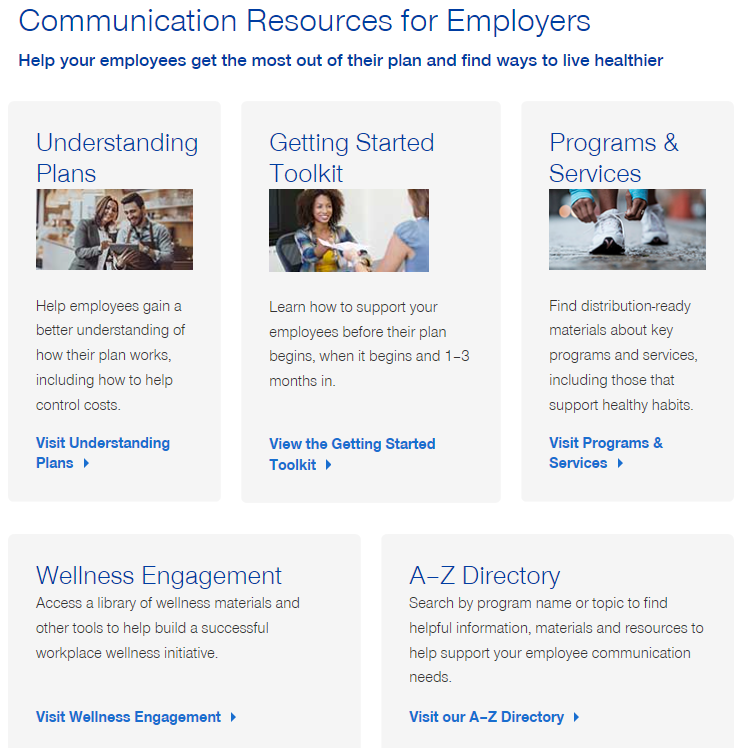
UnitedHealthcare #Wellness Engagement
health topics and articles
Employer Group
- Health Topics
- Nutrition
- Fitness
- Wellness Programs from UHC Flyer
- Rewards Tool Kit brochure
- Individuals
Wellness Employer & Member Materials
- COVID-19 – UnitedHealthcare:
- Employer FAQs
- Broker FAQs
- Our main webpage on COVID
Cafe Well Video
Health Coverage #Guide
Art Gallagher
Health Care Reform FAQ's
Understanding Health Reform
***********************************
Compliance #Assistance Guide from DOL.Gov Health Benefits under Federal Law
- Health Care Reform Explained Kaiser Foundation Cartoon VIDEO
- Choosing a Health Plan for Your Small Business VIDEO DOL.gov
- ACA Quick Reference Guide California Small Group Employers Revision 2020 Word & Brown
- kff.org/health-policy-101/
- Health Savings Accounts
Health Insurance unfortunately is very complicated
President Trump February 27, 2017
- Thus, if we haven't simplified and explained in PLAIN ENGLISH what you are looking for:
FAQ’s
- Question: We keep getting late notices when I’m not late, even the same day they send a bill. They cite AB 2470. What’s up with that?
- Answer: Well I see that I had looked AB 2470 up some time earlier and it says in part, there must be 30 day notice for cancellation.
- So, if one gets a bill for October 1 and doesn’t pay it, they will be cancelled October 31st. So to comply, the Insurance Company must send the bill 30 days ahead of the cancellation day, which is practically the day they send the October bill!
- Here’s Blue Cross’s explanation just as an example
- Ca state law requires we send reminder notice to anyone who has not paid by the due date. We run a report around 25th of the month and mail out the letters by the 27th to anyone who has not paid for the invoice that generated on the 1st of the month (example June invoice generates on 5/1 so on 5/25 if you have not paid June yet we will send this letter on the 27th).
- This is just a reminder notice and its required by law so that is why we have to use certain language. I know some find it threatening but it’s just a reminder and not a threat to cancel you actually have until 6/30 to make the payment. I hope that helps explain.
- See the Administrative Manual and Premium Direct Debit Program above on how to do that.
UnitedHealthcare
#Participation Audit
Do you have a high enough percentage of employees covered?
Are you a bonified business?
- Our UnitedHealthcare Administrative Page
- UnitedHealthcare’s Web Page on Eligibility Verification
Questions about your Eligibility Audit?
Broker ONLY Portal
- Uhceservices.com Reference Guide for Brokers UHC Pdf
- United eServices Small Business Renewal Job Aid bookelet
- eservices
- Broker & Agency Training Catalog
- employer e services.com
- eservices.com Reference Guide for Brokers
- UnitedHealthcare agents and brokers
- Warner Pacific Carrier 411
- e services.com/marketing-materials
- e services.com emp eng planner/view all topics
- Product Grids and Network Documents
- Benefit Summaries & SBCs
- Broker ONLYE Services training Video
- Uhceservices.com Reference Guide for Brokers
- uhc.com/agents-brokers/news-strategies
- Use Key Resources and Level Funding to Get Ahead