HRA’s – Health Reimbursement Accounts Section 105 Plans
MERP
ICHRA Individual HRA
What is HRA’s – Health Reimbursement Accounts
- HRA’s – Health Reimbursement Accounts allow an employer to pay or Self Fund say by using a Ben E Lect Program and possibly save thousands of $$$, for his and the employees uninsured medical care for the diagnosis, cure, mitigation, treatment, or prevention of disease, or for the purpose of affecting any structure or function of the body. and deduct them. TASC * (§IRC §213 (d), IRS Publication 502 Allowable Medical Expenses Internal Revenue Code (IRC) §105 * Publication 969)
- There are also NEW provisions to allow reimbursement for Individual Policies purchased by employees.
What is Section 105 MRP Medical Expense Reimbursement
- Under ACA/Obamacare only reimbursement of medical insurance premiums and qualified “preventative care” are allowed. This puts a huge kibosh on the otherwise huge tax savings for small business entrepreneurs. … The co-pays, deductibles, and other non-covered medical is still allowed by the section 105 MRP plan. The bottom line is the math, and for some, the HSA’s Health Savings Accounts (HSA) may be a better route going forward. Legal Wiz.com
“#Individual Coverage ICHRA”
and the EBHRA “Excepted Benefit HRA ” (can’t pay premiums)
Advantages of the Individual Coverage HRA ICHRA include, but are not limited to:
- Funds can be used to reimburse the employee’s premiums for an individual health insurance policy. Get a quote.
- Employer Contribution will affect tax credits – Learn more here
- Reimbursements made to employees do not count towards the employee’s taxable wages.
- The employer can choose to roll-over unused amounts into the following year.
- Coverage can be offered to different classes of employees (e.g.; full-time, part-time, seasonal, salaried, hourly)
- Contrast to Management Carve Outs §2716 Salary Discrimination
- An offer of the Individual Coverage HRA represents an “offer of coverage” under the employer mandate, however, contributions must meet affordability guidelines. (affordability Health Care.gov) The IRS will release further guidelines regarding this later.
- ICHRA will allow businesses the alternative to offer employees a monthly allowance of tax-free money. It allows them to buy individual health coverage tailored to fit their unique needs, control costs, and address ACA compliance for applicable large employers. ICHRA.com *
The ICHRA Individual Coverage HRA also comes with restrictions and regulations including but not limited to:
- An offer of an Individual Coverage HRA cannot be made to any employee that is offered a traditional group health plan.
- If an offer of coverage is made to a class of employees, there is a minimum class size that is required. Size is typically 10% of that specific class of employees. For example, if an employer has 200 employees, a minimum of 20 employees would have to be in a specified class.
- Contributions can be in any amount that the employer chooses, but contributions must be consistent for all employees in a specified class.
- The employer must provide notice of the Individual Coverage HRA to employees.
- The employer must be able to substantiate that the employee is enrolled in an individual plan or Medicare (model notices are available).
- The employer must notify employees on an annual basis that the individual health insurance is NOT subject to ERISA.
- The final rule also created the “Excepted Benefit HRA“ which, starting in January of 2020, will permit employers to finance additional medical care. Employees can use the HRA without having to be enrolled in the group’s traditional health plan.
- The requirements associated with the “Excepted Benefit HRA” include, but are not limited to:
-
-
- The annual contribution is capped at $1,800.
- It must be offered in conjunction with a group health plan, but there is no requirement for the employee to enroll in that plan.
- The “Excepted Benefit HRA” cannot be used to fund group health or Medicare premiums.
- It can fund premiums for dental, vision, or short-term limited duration insurance.
-
- Employers who want to offer the “Individual Coverage HRA” can do so but employees will need to enroll in an individual plan during the open enrollment period. benefitmall.com * TASO FAQ’s * Take Command Heatlh FAQ’s * Health Care.gov * SHRM.org *FAQ’s
FAQ’s, Links & Resources
- Complete ICHRA Guide
- Section 105 Non Discrimination requirements
- CMS.Gov FAQ’s
- SHRM’s New Final Rule Lets Employees Use HRAs to Buy Health Insurance
- people keep.com//what-to-expect-from-the-individual-coverage-hra-ichra-in-2020
- Commission Opinion Letter: Individual Coverage Health Reimbursement Arrangements (ICHRA) under the ADEA EEOC.gov *
Jump to section on:
Just Enter your census or securely send us an excel spreadsheet or a list of employees and get instant proposals
for all these companies that we are Authorized Agents for in California
The 21st Century Cures Act
President Barack Obama on Dec. 13 signed into law the 21st Century Cures Act, which will let small businesses use health reimbursement arrangements (HRAs) to fund employees who purchase individual health plans on the open market.
Learn More===>SHRM.org
The Cures act incorporates key elements of the proposed Small Business Healthcare Relief Act, creates a new type of HRA—the qualified small employer health reimbursement arrangement (QSEHRA). The legislation specifies that:
- The maximum reimbursement for health expenses that small employers can provide through employee QSEHRAs is $4,950 for single coverage and $10,000 for family coverage, to be adjusted annually for inflation.
- Small employers that choose to provide QSEHRAs must offer them to all full-time employees except those who have not yet completed 90 days of service, are under 25 years of age, or who are covered by a collective bargaining agreement for accident and health benefits. Part-time and seasonal workers may also be excluded.
- Generally, an employer must make the same QSEHRA contributions for all eligible employees. However, amounts may vary based on the price of an insurance policy in the relevant individual health insurance market, which in turn can be based on the age of the employee and eligible family members, or the number of family members covered.
- Learn More===SHRM.org
HRA Health Reimbursement Account
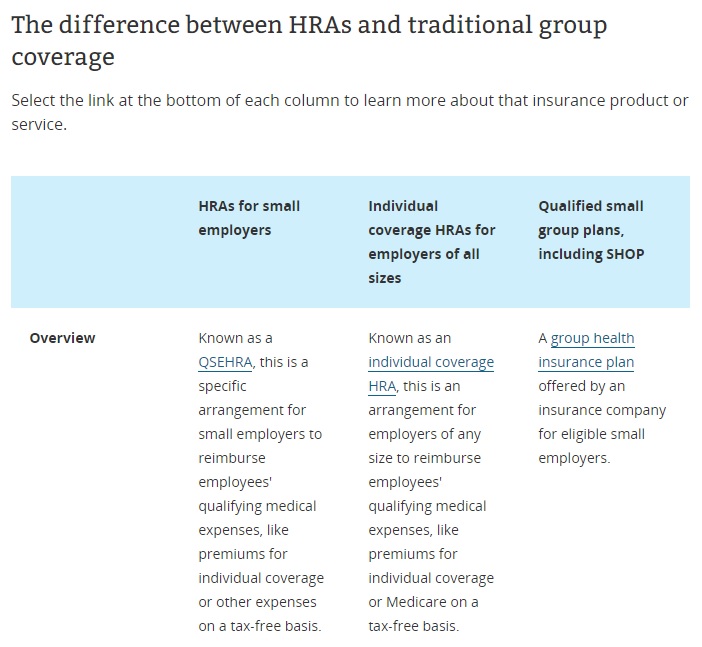
HRAs, ICHRA, QSEHRA and traditional group coverage
- Individual Coverage Health Reimbursement Account ichra.com/ichra-defined on ichra.com
- Health Reimbursement Arrangements CMS.Gov
- Read the full comparison on
- Deciding between group coverage & an HRA? Health Care.gov *
- Individual coverage Health Reimbursement Arrangements (HRAs) Health Care.gov *
- Get Employer Quotes
- House passes GOP bill increasing options for employer health insurance coverage
Section 105 MERP Medical Expense Reimbursement Account
MERP’s – Medical Expense Reimbursement Plans – Section 105
- HOW SECTION 105 MEDICAL REIMBURSEMENT PLANS SAVE ON TAXES Difference Card.com
- Some companies allow and some don’t IRS Section §105 MERPs Wikipedia
- Blue Cross requires a signed statement that you won’t do it). Qualified claims must be described in the HRA plan document at inception, i.e., before reimbursing employees for those medical expenses.
- The employee does not have to report income as long as the plan complies with §106, 105 (b) and Rev Ruling 2-41 The funding for medical expenses can be pay as you go.
- Companies that allow HRA’s & HSA’s (Health Savings Accounts).
- Aetna,
- Kaiser
- UHC and
- Health Net
- Please email [email protected] or call us 310.519.1335 to discuss further.
- Instant Quotes
Consumer Links & Resources
- Aetna FAQ’s & Explanation non discrimination executive medical
- IRS More Info on Health Care Arrangements to not have a group plan but pay for employee individual plans Make sure your plan is ACA compliant or face HUGE penalties Wikipedia Other Insurance Clause – Dual Coverage?
- Can the 105 plan pay lower benefits depending on the amount the employee receives from other insurance, like Medicare?
- Section 105- Amounts Received Under Accident and Health Plans (Also Section 106-Contributions by Employers to Accident and Health Plans) Rev. Rul. 2005-24
Administrators – Plan Documents
- Core Documents.com
- TASC for HRA’s
- Purchase Plan Documents – It is not necessary for tax purposes that the plan be in writing or that the employee’s rights to benefits under the plan be enforceable. For example, an employer’s custom or policy of continuing wages during disability, known to the employees generally, has been held to constitute a plan. Niekamp v. U.S. , 240 F. Supp. 195 (E.D. Mo. 1965); Pickle, TC Memo 1971-304
- Employer Driven Insurance Services, Inc.
Instant Term Life Insurance Quote #naaipquote
- Schedule Zoom consultation
- Tools - Calculator to help you figure out how much you should get
- How much life insurance you really need?
Life Insurance Buyers Guide
Level Funding
Self Funded, Level Funding & #MEC plans
opti med health.com
- Key Resources & Level Funding to get ahead – Trustmark February 2023

Resources & Links
- CA Law restricting stop loss HR Daily Advisor
- lbl group.com/sb-161-effect-stop-loss-california-self-funded-health-insurance
- S.B. 161 prohibits stop-loss insurers in California from issuing policies with specific deductibles below $35,000 for self-funded employer plans. After Jan. 1, 2016, the law increases the minimum specific attachment point to $40,000.
- Also under the law, starting Jan. 1, aggregate attachment points cannot be less than $5,000 times the total number of group members, 120 percent of expected claims, or $35,000 ($40,000 after Jan. 1, 2016). HR Daily *
- leginfo.legislature.ca.gov/
- leavitt.com/sb-161-limits-stop-loss-for-self-funded-small-employer-health-plans/
- Self-Funding – Life After SB-161: Is Self Funding Still Viable In California?
Tax Guides



https://hub.calbrokermag.com/company/the-difference-card#engagement-video
https://excelhealthplans.com/
https://hub.calbrokermag.com/resource/the-difference-card-how-section-105-medical-reimbursement-plans-save-on-taxes
https://kffhealthnews.org/news/article/ichra-benefit-trend-employers-health-plan-allowance-individual-insurance/