Maternity – Birth Control – Infertility
Sample ACA/Obamcare/Covered CA INDIVIDUAL
Silver 70 PPO EOC – Evidence of Coverage – Full Policy
How to read a policy our webpage
Scroll down for Small Employer Group Plans
How is Maternity Covered under
ACA/Health Care Reform/Obamacare
-
- Benefits are available for maternity care services.
- Benefits include:
- Prenatal care;
- Postnatal care; Scroll down for more information.
- Involuntary complications of pregnancy;
- Inpatient Hospital services including labor, delivery, and postpartum care;
- Elective newborn circumcision within 18 months of birth; and
- Pregnancy termination services. G-d Forbid
- See the Diagnostic X-ray, imaging, pathology, and laboratory services and Preventive Health Services sections for information about coverage of genetic testing and diagnostic procedures related to pregnancy and maternity care.
- The Newborns’ and Mothers’ Health Protection Act requires health plans to:
- provide a minimum Hospital stay for the mother and newborn child of 48 hours after a normal, vaginal delivery and
- 96 hours after a C-section.
- The attending Physician, in consultation with the mother, may determine that a shorter length of stay is adequate.
- If your Hospital stay is shorter than the minimum stay, you can receive a follow-up visit with a Health Care Provider whose scope of practice includes postpartum and newborn care. This follow-up visit may occur at home or as an outpatient, as necessary. This visit will include parent education, assistance and training in breast or bottle feeding, and any necessary physical assessments for the mother and child. Prior authorization is not required for this follow-up visit. Page 67 Specimen Policy – Be sure to check YOUR EOC Evidence of Coverage .
- DOL FAQ’s on Newborn and Mothers Health Protection
- Why??? Encouragement to have more babies – Otherwise civilization will end… NPR 4/25/2025 *
- Benefits include:
- References & Links
- Health costs associated with pregnancy, childbirth, and postpartum care
- The high costs of having a baby: New analysis shows childbirth sticker shocks in the U.S
- The staggering financial burden of giving birth — even with insurance
- Women who Give Birth Incur Nearly $19,000 in Additional Health Costs, Including $2,854 More that They Pay Out of Pocket
- My body has changed forever, stretched in ways I’d never imagined since my two pregnancies. My hips have widened, my stomach is softer. There will always be a gap between my abdominal muscles. I have stretch marks, my first and only tattoos. My back aches and feels weaker than before. My boobs are smaller and softer.
- California gives new moms extra Medi-Cal benefits. It can’t say who’s using them
- nbcdfw.com/middle-class-insured-childbirth-crippling-debt
- the mother baby center.org/ labor-induction/
- Blue Shield Mavin
- Blue Shield of California and Maven are here to support fertility and pregnancy journeys every step of the way. With Maven, you and your partner can get access to virtual support for fertility, pregnancy and postpartum. You’ll enjoy 24/7 access to Care Advocates, specialists, mental health support, and content tailored to your experience.
- Confirmation from Blue Shield 12/8/2025 Maven is included within our IFP plans at no additional cost However, please note that infertility treatments (IVF) are not covered under any individual plans.
- Changes under Trump – less testing, screening… Time *
- Health Net Ambetter Maternity & Family Planning
- What is a Midwife – California Health Care Foundation *
- Advantages to Employer if there is less parental stress Kaiser.org *
- Benefits are available for maternity care services.
All our Health plans are Guaranteed Issue with No Pre X Clause
Instant Quote & Subsidy #Calculation
There is No charge for our complementary services, we are paid by the Insurance Company.
- Our Quote Engine Takes all the complexity out of using pencil and paper to figure out the premiums per the Obamacare/ACA rules under CFR §1.36B-3 *
- We are authorized Brokers for Dental, Vision & Covered CA get instant quotes direct and in Covered CA with subsidy calculation for:
- Watch our 10 minute VIDEO that explains everything about getting a quote
Contact Us - Ask Questions - Get More Information - Schedule a Zoom Meeting
[email protected]
By submitting the information below , you are agreeing to be contacted by Steve Shorr a Licensed Sales Agent by email, texting or Zoom to discuss Medicare or other Insurance Plans as relevant to your inquiry. This is a solicitation for Insurance
Instant Term Life Insurance Quote #naaipquote
- Schedule Zoom consultation
- Tools - Calculator to help you figure out how much you should get
- How much life insurance you really need?
Life Insurance Buyers Guide
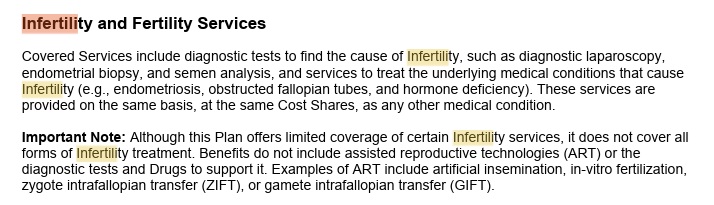
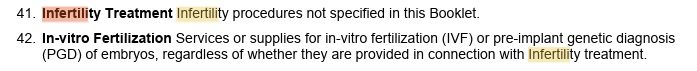
Infertility Coverage
Employer Group Plans
Infertility on California
Group Employer Plans
- IVF covered in CA new law
- SB 729 Treatment for infertility & fertility services requires large health insurance companies to cover in vitro fertilization
- The bill also expands healthcare benefits to LGBTQ+ families seeking to have children, changing the definition of infertility for insurance purposes to include “a person’s inability to reproduce either as an individual or with their partner without medical intervention.” Read more >>> Los Angeles Times
-
- large and small group health plans issued or renewed after July 1, 2025, must provide coverage for the diagnosis and treatment of infertility and fertility services. It will remove the exclusion of in vitro fertilization from coverage.
- Kaiser Summary
- SB 62 Update CA Benchmark Plan Essential Benefits legislature.ca.gov
- KFF News
- Blue Shield FAQ’s
- Visit our webpage on how to read your EOC Evidence of Coverage – Actual Policy
- time.com//trump-ivf-fertility-insurance
- politico.com//2025/10/25/free-ivf-fizzled-
- white house.gov/2025/10/fact-sheet-ivf-and-high-quality-fertility-care/
- SB 729 Treatment for infertility & fertility services requires large health insurance companies to cover in vitro fertilization
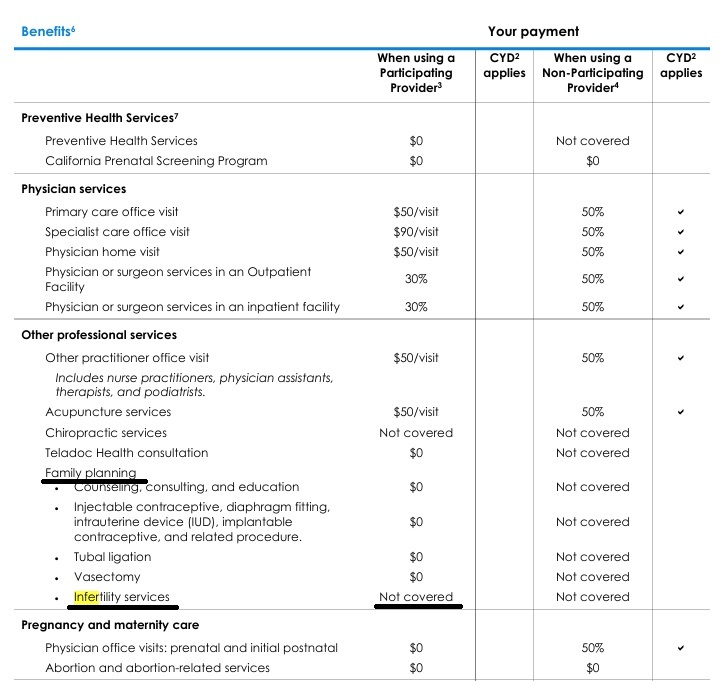
Excerpt from Health Net Plan Guide
- infertility – CA Law? and newborn care.
- §146.130 Standards relating to benefits for mothers and newborns.
- Maternity: Inpatient hospital and ambulatory
- Prescription drug coverage for contraceptives
- Maternity hospital stay
- Sterilization operations and procedures View the Affordable health ca.com page Assembly Bill 1453 (Monning) and Senate Bill 951 (Hernandez). View the California Health and Safety Code, section 1367.005
- ivf specialists.com
- If You’re Poor, Fertility Treatment Can Be Out of Reach
- Federal?
-
IVF – Fertility Treatments
- Even When IVF Is Covered by Insurance, High Bills and Hassles Abound
- Should health insurers cover the cost of fertility treatment?
- Overturning Roe V. Wade: Here’s How It Could Impact Fertility Treatments And IVF
- Aetna Clinical Bulletin Infertility
- Infertility Definition
- May be either of the following:
- A demonstrated condition recognized by a licensed Physician or surgeon as a cause for Infertility; or
- The inability to conceive a pregnancy or to carry a pregnancy to a live birth after a year of regular sexual relations without contraception.
- May be either of the following:
- Fertility preservation services
- Fertility preservation services are covered for Members undergoing treatment or receiving Covered Services that may directly or indirectly cause iatrogenic Infertility. Under these circumstances, standard fertility preservation services
- are a Covered Service.
- Exclusion
- Any services related to assisted reproductive technology (including associated services such as radiology, laboratory, medications, and procedures) including but not limited to
- the harvesting or stimulation of the human ovum,
- in vitro fertilization,
- Gamete Intrafallopian Transfer (GIFT) procedure,
- Zygote Intrafallopian Transfer (ZIFT),
- Intracytoplasmic sperm injection (ICSI),
- preimplantation genetic screening,
- donor services or procurement and storage of donor embryos,
- oocytes, ovarian tissue, or sperm,
- any type of artificial insemination, services or medications to treat low sperm count, or services incident to reversal of surgical sterilization,
- except for Medically Necessary treatment of medical complications of the reversal procedure. Specimen Policy use Ctrl F to find
- Any services related to assisted reproductive technology (including associated services such as radiology, laboratory, medications, and procedures) including but not limited to
- Alabama Republicans want to give IVF doctors immunity after court rules frozen embryos are kids
- Senate Democrats Plan Speedy Action In Defense Of IVF Treatments
- Federal Law
Birth Control
Birth Control – Contraception
-
- Birth control benefits
- Plans in the Health Insurance Marketplace® must cover contraceptive methods and counseling for all women, as prescribed by a health care provider.
- Plans must cover these services without charging a copayment or coinsurance when provided by an in-network provider — even if you haven’t met your deductible.
- Covered contraceptive methods
- FDA-approved contraceptive methods prescribed by a woman’s doctor are covered, including:
- Barrier methods, like diaphragms and sponges
- Hormonal methods, like birth control pills and vaginal rings
- Implanted devices, like intrauterine devices (IUDs)
- Emergency contraception, like Plan B® and ella®
- Sterilization procedures
- Patient education and counseling
- FDA-approved contraceptive methods prescribed by a woman’s doctor are covered, including:
- Plans aren’t required to cover drugs to induce abortions and services for male reproductive capacity, like vasectomies.
TIP To be sure if a specific method is covered by your plan, check your plan’s materials or ask your employer or benefits administrator. - Birth control benefits rules for employer-provided coverage
- If you work for a religious employer
- Health plans sponsored by certain exempt religious employers, like churches and other houses of worship, don’t have to cover contraceptive methods and counseling.
- If you work for an exempt religious employer and use contraceptive services, you may have to pay for them out-of-pocket. Contact your employer or benefits administrator for more information.
- If you work for a non-profit religious organization
- Some non-profit religious organizations — like non-profit religious hospitals and institutions of higher education that certify they have religious objections to contraceptive coverage — don’t have to contract, arrange, pay, or refer for contraceptive coverage.
If your health plan is sponsored or arranged by this type of organization, an insurer or third party administrator will make separate payments for contraceptive services that you use.
- You’ll have access to contraceptive services without a copayment, coinsurance, or deductible when they are provided by an in-network provider.
- Contact your employer or health plan to learn more. health care.gov/ /birth-control-benefits
- Insurers must provide contraceptive coverage at no cost or face potential enforcement action, according to new federal guidance meant to counter reports of coverage denials.
- xyz got caught and has been ordered to reimburse the member — and all others in her situation — for the out-of-pocket costs they incurred. LA Times June 2024
- Why It’s So Hard to the Get Birth Control You Want Covered by Insurance Time Magazine
- HHS, Labor and Treasury put insurers on notice about ACA contraception coverage
- Contraception’s Complains
- Top Biden officials press insurers on contraceptive coverage Advocates for broad coverage say insurers are skirting the rules and denying coverage in some cases
- Birth control benefits
- HHS Warns Insurers Of Penalties If Birth Control Is Not Covered
- California Wants to Snip Costs for Vasectomies
- Our webpage on Preventative Care
- Search Ctrl F * Specimen Policy * for contraception
Abortion
Abortion G-d Forbid
- California governor signs law making abortions cheaper
- Aetna Clinical Policy Bulletins
- Mifepristone (Mifeprex; also known as RU 486)
- CA Department of Insurance Abortion G-d forbid
- kff health news.org/abortion-care-denial-life-threatening-exception-wisconsin/
- kff health news.org/ after-abortion-was-wiped-from-cdc-website-users-now-get-adoption-info