How to find a network provider?
no index
It can sometimes be difficult to find a provider that is accepted by your Insurance Company. Meaning they are a Network Provider whether you are in an HMO, PPO, etc. Even in a PPO, you get paid best when using a Network Provider.
FAQ on how to read list of accepted Insurance on a Provider – Hospital Site
See below on finding a provider in your network and/or
MD & Hospital Finder – Quotit – All Companies
Check our Companies – Carriers page and then get more detail on how to use their provider finder
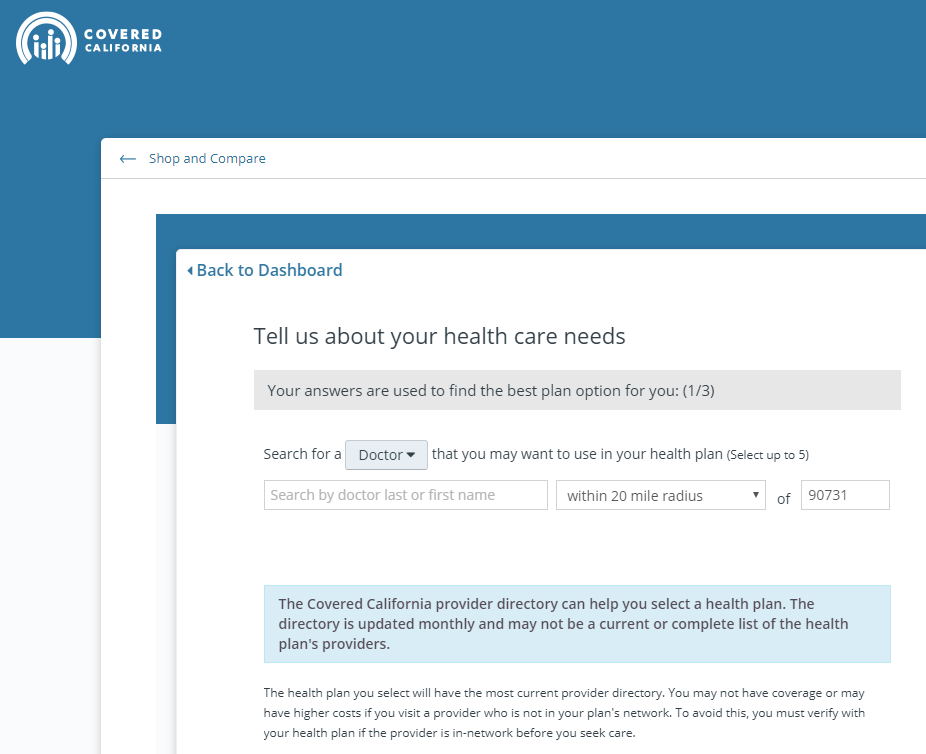
Covered CA Search
1st use their Shop & Compare Tool
Network Definitions throughout our website and all the different Insurance Companies
Mirrored Plans – same network & benefits in and out of Covered CA
- Provider Networks & Search Health Net
- Narrow Networks – 3 month grace period
- Blue Shield PPO Out of State & Country
- Provider Lists – Definitions HMO, Tiered – PPO, PPO, EPO
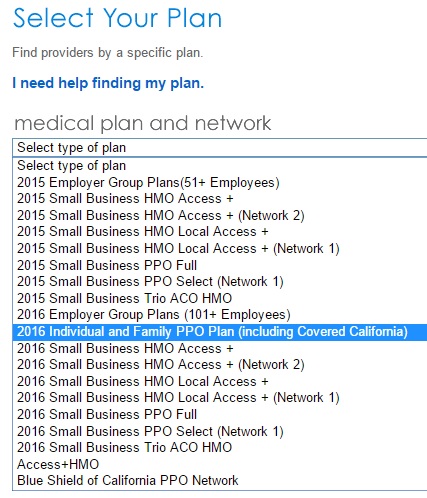
- Provider Finder – Instructions * Exclusive PPO – Trio HMO
- Pharmacy, Doctor & Provider Finder Oscar
Employer Plans
Health Net
United Health Care
Check the definition in your EOC Evidence of Coverage
Links & Resources
Health Grades.com Find an MD and get ratings – we have no control over outside links – evaluate for yourself
California Choice – Web MD Tool – Compare Hospitals Outcomes
CHFC Study on Provider Lists 9.2015
Network, HMO, PPO etc. explanation on Insure Me Kevin.com
Glossary – Definitions
View actual Evidence of Coverage page 14 and check out the definitions and explanations of the role of the PCP Primary Care Physician and IPA Independent Practise Assoc.
NEW Provider Finder tools for our clients and future clients, who get free proposals by clicking here for individuals or here for employer groups.
Just send us your list (Word & Brown Group Form) of MD’s, specialty, city – address to [email protected] and we can search ALL Small Group Plans & Networks, we can now do Individual too per Duncan S… and send you back a report using the proprietary strenuus.com system, Broker Log In.
InsuBuy International Medical Coverage – Instant Quotes & Enrollment
Historical
- Tier 1 & 2 List ♦ Insure Me Kevin.com Blog ♦ Where to get care flyer – ER vs Urgent Care, etc. ♦ Instructions ♦ Network Info ♦ Pathway is the same on and off the exchange. We are required by Covered CA to list it as Pathway X on provider finder. Email dated 11.17.2015 ♦ Live Health ONLINE ♦ More Info
-
- Provider Lists – Definitions HMO, Tiered – PPO, PPO, EPO
Assurant (Aetna PPO) Not writing Business for 2016 Cedar’s Sinai – Alternatives for 2016
- L
os Angeles Times – Covered CA Provider FinderPublished 9.28.2014 – Forget it, hasn’t been updated!
same Narrow Network in or out of Covered CA.
Explanation on Insure Me Kevin.com
We will grant you that some are very difficult to use, even for us, with advanced degrees in Insurance and 30+ years of experience. See this page on instructions and this one on narrow lists under Health Care Reform if you need additional help. SB 137 effective 1.1.2016 hopefully will make things easier.
Child, Related Pages
& Site Map
[child-pages]
#Covered CA Certified Agent
No extra charge for complementary assistance
- Get Instant Health Quotes, Subsidy Calculation & Enroll
- Appoint us as your broker
- Get Instant Health Quotes, Subsidy Calculation & Enroll
- Videos on how great agents are



What does it mean, when the provider list says, doctor not accepting new patients?
They’re saying I’m a new patient because I just signed on with them as my insurance and that my doctor isn’t taking new patients. That’s nonsense. I’ve been with her 12 years.
I don’t like to cite “forum” websites, but this is the best explanation I found so far…
http://www.city-data.com/forum/health-insurance/2302915-not-accepting-new-patients-2.html
One recently published study showed as many as a fourth of the doctors listed in California directories last year for marketplace plans were not accepting new patients.
Gentieu found that only 15 percent of those listed as primary care doctors in one Medical Mutual network were actually primary care physicians taking new patients. Many had not accepted new patients in years.
Physicians often fail to tell insurers when they stop accepting patients for certain plans, Medical Mutual and other carriers said.
https://khn.org/news/insurers-flawed-directories-leave-patients-scrambling-for-in-network-doctors/
Lopez pointed to a new California law that took effect July 1 requiring insurers to update their online directories once a week and their printed ones every quarter.
https://khn.org/news/inaccurate-provider-lists-a-major-barrier-to-care-study-finds/
“We’d have customers call up [a doctor] and they’d say, ‘We take Blue Cross PPO,’” said John Jaggi, an Illinois broker. “But they didn’t take Blue Choice Preferred PPO.” Neither the patient nor the doctor’s office knew the difference, he said.
https://khn.org/news/insurers-flawed-directories-leave-patients-scrambling-for-in-network-doctors/
call the doctors’ offices and ask if they are accepting new patients. Be sure to ask whether they will accept your insurance plan.
Somewhere there is a legal case, that the plain meaning to the average person is the definition to be used
http://www.calhealthreport.org/2017/09/25/despite-new-law-doctor-directories-still-often-inaccurate/
CONTRACT AMBIGUITIES CONSTRUED AGAINST DRAFTER
The Latin term contra proferentem is a contract principle that provides that an ambiguous or uncertain term in a contract will be construed against the party that caused the uncertainty to exist. Civ. Code§ 1654. Ambiguities are contract language that is difficult to comprehend or distinguish. Royal Neckwear Co. v. Century City, Inc., 205 Cal.App.3d 1146, 1153 (1988).
The plain meaning of the contract will be followed where the words used—whether written or oral—have a clear and unambiguous meaning. Words are given their ordinary meaning; technical terms are given their technical meaning; and local, cultural, or Trade Usage of terms are recognized as applicable. The circumstances surrounding the formation of the contract are also admissible to aid in the interpretation.
West’s Encyclopedia of American Law, edition 2. Copyright 2008 The Gale Group, Inc. All rights reserved.
See also some of our other pages that talk about accepting new patients:
https://individuals.healthreformquotes.com/provider-finder/narrow-lists/out-of-network-problems/
https://individuals.healthreformquotes.com/open-enrollment-for-individuals-families/ccr-code-regulations-ca-%C2%A76504-special-enrollment-periods/special-enrollment-triggering-events/md-network/
https://individuals.healthreformquotes.com/open-enrollment-for-individuals-families/ccr-code-regulations-ca-%C2%A76504-special-enrollment-periods/special-enrollment-triggering-events/error-material-violation/
https://individuals.healthreformquotes.com/provider-finder/narrow-lists/class-action-doi-investigation/
Modern healthcare how to create a better after visit summary