Negotiated Fee Rate
What is the regular Price?
Balance – Surprise Billing
Negotiated Fees
The #Negotiated Fee – Rate is the amount of payment that an Insurance Company has negotiated with the Participating Provider as the maximum they can charge both the Insurance Company and YOU! hioscar.com/negotiated-rate * Page 42 Blue Cross EOC & 167 More explanation calhealth.net
So, NO a doctor on the Insurance Companies Participating Provider list, can NOT make you pay the difference! That’s why it’s important to double check with the doctor and the LIST!
Excerpt from Blue Shield Explanation
It’s the secret number the insurance company and the provider have worked into their contract. The industry often calls that number the “adjusted rate” or the “negotiated rate.” NPR.org
View an actual Specimen Policy Explanation EOC Evidence of Coverage – Page 42 Blue Cross EOC & 167 More explanation calhealth.net–
How do I know that the amount I’m being billed
is the correct amount?
Once your insurance carrier pays their portion of the bill, they will send you an explanation of benefits (EOB) to show how the claim was paid. You can compare your EOB to the statement sent by the hospital. How the carrier paid the claim is based on their contract with us and their contract with you. If you feel the insurance company should have paid a higher amount, please contact them directly for resolution. Scripts.org Patient Billing FAQ’s
Todd Friedman, Esq. can help if debt collectors are harassing you when you don’t owe the $$$
Why insurers are paying double for the same procedure in the same hospital
#Out of Network Problems
Updating Online Provider Lists
- Health plans must update their printed directories at least every quarter and their online directories at least every week if providers report changes.
- Provider directories must be posted online and be available to anyone, not just enrollees. Print directories must be available upon request.
- The directories must “prominently” display directions for consumers who want to report inaccuracies. Upon receiving complaints, plans have 30 business days to makes changes, if necessary.
- Providers must inform plans within five business days if they are no longer accepting new patients — or, alternately, if they will start accepting them.
- Health plans can delay payments to providers who fail to respond to attempts to verify information.
- The law also gives consumers recourse. Let’s say you use a provider directory to find a doctor but you’re billed the out-of-network price because the directory was wrong. In that case, health plans must reimburse you the amount beyond what you would have paid to see an in-network doctor. SB 137 Insurance Code §10133.15 Effective 7.1.2016* CA Health Line 8.26.2016
- Insure Me Kevin.com on MD’s using bait and switch to mess with the networks 6.18.2016
- Bay Area – Blue Cross – virtually no providers – Insure Me Kevin.com 8.25.2016
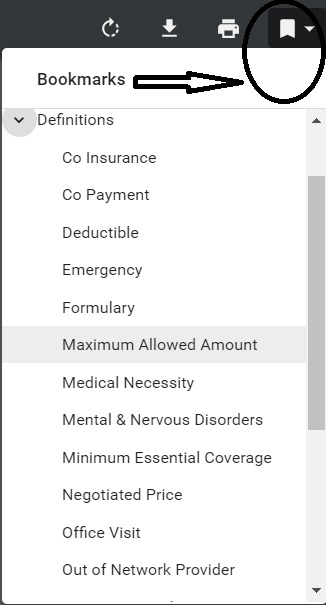
- Out of Network Provider
- The use of health care providers who have not contracted with the health plan to provide services. HMO members are generally not covered for out-of-network services except in emergency situations. Members enrolled in preferred provider organizations (PPO) and point-of-service (POS) coverage’s can go out-of-network, but will pay some additional costs. Learn More ==> Specimen Policy Definition page 168
-
…Then in October, they were told Dignity Health was out of network.
“What we were faced initially when the problem came to our mailbox, even though it had been going on for probably five months prior to us being made aware, we were faced with about $100,000 of medical bills,” Read more *
-
Does the negotiated rate apply to #prescriptions Rx too?
That is, if I have Blue Shield Bronze Plan with no Rx coverage till the $7k OOP Out of Pocket Maximum has been met, do I get the lower negotiated – contracted rates?
- Yes, see excerpts from Blue Shield Bronze PPO EOC below
- Blue Shield Participating Providers include primary care Physicians, specialists, Hospitals, and Alternate Care Services Providers that have a contractual relationship with Blue Shield to provide services to Members of this Plan. Participating Providers are listed in the Participating Provider directory.
- Participating Providers agree to accept Blue Shield’s payment, plus the Member’s payment of any applicable Deductibles, Copayments, and Coinsurance or amounts in excess of specified Benefit maximums as payment-in-full for Covered Services, except… Page 2 of EOC
- Blue Shield negotiates contracted rates with Participating Pharmacies for Drug. If the Member’s Plan has a Calendar Year Pharmacy Deductible, the Member is responsible for paying the contracted rate for Drugs until the Calendar Year Pharmacy Deductible is met.
- The Member must pay the applicable Copayment or Coinsurance for each prescription when the Member obtains it from a Participating Pharmacy. When the Participating Pharmacy’s contracted rate is less than the Member’s Copayment or Coinsurance, the Member only pays the contracted rate. Page 25 of EOC
- Learn More===> EOC explains all about Rx benefits
- Here’s how Medicare under Part D handles it. I grant you, that I don’t understand what CMS is saying here…
- Part D Definitions 42 CFR 423.100
- The Blue Cross Specimen Policy explains Rx coverage starting on page 120.
- SHRM Article
- Insure Me Kevin.com on Bronze Deductible….
- Shop & Compare Tools Part D Rx
- Part D Rx Low Income Subsidy – LIS – Extra Help
- Prescriptions Drugs – Rx – Including under 65 ACA
Miscellaneous
- Yes, see excerpts from Blue Shield Bronze PPO EOC below
What’s on this page?
All our plans are Guaranteed Issue with No Pre X Clause
Quote & Subsidy #Calculation
There is No charge for our complementary services
Watch our 10 minute VIDEO
that explains everything about getting a quote
- Our Quote Engine Takes all the complexity out of using pencil and paper to figure out the premiums per the Obamacare/ACA rules under CFR §1.36B-3 *
- Get more detail on the Individual & Family Carriers available in CA
Hospitals will be required to #post online their standard charges!
- Transparency rules have been around for a while. Cal Broker 8.7.2018 * The Hill * CMS is looking for a contractor to create a price comparison tool. Modern Health Care 8.28.2018 LA Times 6.10.2016
- the top 10 hidden facts about hospital prices that answer questions about why it is so expensive and why the bills are so complicated Read More Med City News.com *
- Health insurance prices for care are now out there, but finding them is an ordeal
- Study finds hospitals are still not posting prices 1/2023
- Health Insurance Price Data: It’s Out There, but It’s Not for the Faint of Heart
- New price transparency regulations for hospitals, insurers empower patients
- More Consumers Find Transparency Tools Accessible, Useful in 2022
- Few hospitals are posting the prices of their common procedures online, despite a federal law that went into effect more than a year ago
- Many hospitals are required to provide an itemized bill upon request
- Pre-service cost estimates: A tale of two patient journeys
- Where consumers look for health care pricing information, charted
- cms.gov/health plan-price-transparency/consumers
Trump Executive Order
Trump Executive order directs federal agencies to issue guidance that would:
- Require hospitals to disclose information about negotiated rates in a format that’s understandable and usable by patients and consumers.
- Require insurance companies to provide patients with information about the cost of their care, including out-of-pocket costs before they receive services.
- Develop a comprehensive roadmap for consistent, limited, and consumer-centric quality metrics.
- Expand the availability and use of HSAs to cover direct primary care arrangements and healthcare sharing ministries. It also seeks to include more preventive services that can be covered in the deductible period.
- Rules issued – Modern Health Care 11.15.2019 * HHS.gov *
- cms.gov/hospital-outpatient-prospective-payment-system-opps-policy-changes-hospital-price
- cms.gov/newsroom/fact-sheets/transparency-coverage-proposed-rule-cms-9915-p
- The final rule (CMS-1717-F2)
- The proposed rule (CMS‑9915‑P)
Healthcare Payments Database,
Some argue that negotiated prices are proprietary — that is, legally protected trade secrets — and that their disclosure could foster collusion between providers. Other observers maintain that disclosure could help policymakers understand what is driving cost increases and how best to target efforts to make care more affordable.
The Secret of Health Care Prices: Why Transparency Is in the Public Interest, analyzes, for the first time, the legal and economic implications of collecting and releasing this data, including a review of trade secret statutes and case law regarding the protection of negotiated prices as trade secrets and data dissemination practices from the 18 states with mandatory APCD collection programs.
Accompanying the report, a blog post examines recent developments in price transparency policy, the arguments for and against the release of proprietary price information, and steps California could take to help ensure its new database is a success
hospitals have asked the courts to through the rule out! Modern Health Care 5.7.2020 * New York Times 12.4.2019 *
Links & Resources
- californiahealthline.org/dont-try-it-at-home/
- LA Times itemized bill should be the norm.
- Health Affairs.org 1.19.2021
- Heath Care Dive.com 12.8.2020
- Denver Channel.com
- latimes.com/white-house-seeks-healthcare-price-disclosure
- California health foundation on why we need Price transparency
- npr.org/trump-teams-bid-to-make-hospital-costs-more-transparent-is-data-heavy
- chcf.org/whats-behind-hospital-prices (looking glass)
- Health plans can do more to improve price transparency for consumers, survey finds
Resources to find out the costs of Medical Services
- Charge Master – Coding – Optum 360 – Hospitals must post this starting 1.1.2019 *
- Leaked SoCal hospital records reveal huge, automated markups for healthcare Los Angeles Times 12.10.2021
- fair health consumer.org/
- health care blue book.com
- transplant.org – costs per transplant
- Kaiser Family Foundation – Tons of Information
- shrm.org/negotiating-drug-prices
- clinic price check.com
- fair health consumer.org
- health care blue book.com
- dhs.lacounty.gov/hospital-price-transparency/
Kaiser & Blue Shield
Treatment Cost #Estimator Tool
requires sign in
The tool is for all Kaiser Members that are enrolled on Deductible or Health Savings Account Plans. The cost estimates are for services that are marked "after deductible" to give members an idea of the cost of those services.
- 2021 Kaiser Sample Fee List
- How do I know what level of service I will get billed for?
- BLUE SHIELD Treatment Cost Estimator – for PPO Members
- Cost Helper.com what people are paying for health services
Mandated Posting of Negotiated Rates
#Transparency-in-coverage regulation
- Here’s the negotiated rate machine readable webpages for the following Insurance Companies:
- Cal Choice
- Anthem Blue Cross
- Blue Shield
- CIGNA
- Centene – Health Net
- Kaiser
- Sharp Health Plan
- Sutter Health
- United Health Care
- Western Health
- FAQ’s from the United States Departments of Labor, Health and Human Services, and Treasury.
- Most health insurers have released their rates. Now, experts detail what they are doing with the data
- mercer.com/2022-aca-cost-sharing
- kff.org/surprise-medical-bills-2022/
- UHC FAQ’s
- Transparency in Coverage Final Rule Fact Sheet (CMS-9915-F)
- cms.gov/health plan-price-transparency
#Balance Billing
Balance Billing is when an insurance plan covers less than what a doctor, hospital, or lab service wants to be paid. The health-care provider demands, bills the balance from the patient. Uncertain and fearing the calls of a debt collector, the patient pays up. Business Week 8.27.2008 is NOT allowed in CA for Emergency Care, even if out of network. See our provider finder
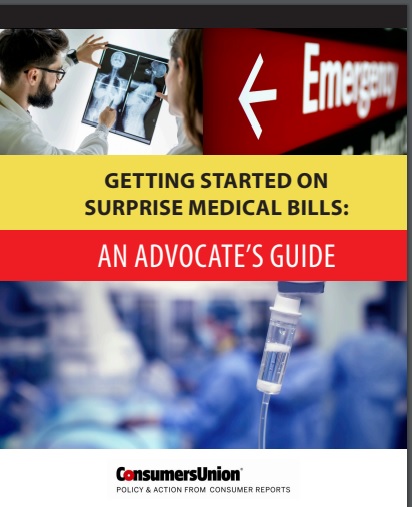
The No #Surprises in Medical Bills Act
The no surprises act holds consumers harmless from the cost of unanticipated out-of-network medical bills. Surprise bills arise in in emergencies – when patients typically have little or no say in where they receive care. They also arise in non-emergencies when patients at in-network hospitals or other facilities receive care from ancillary providers (such as anesthesiologists) who are not in-network and whom the patient did not choose.
No Surprises ACT – CMS bans surprise billing! Modern Health Care * 400 page Rule CMS 9909 * HHS.Gov * CMS.Gov * CMS Requirements * Modern Health Care – Ending Surprise Billing won’t solve Medical Debt problem * Providers flexing debt collection muscles * Feds had been looking into CA’s legislation to craft something on a National Level Modern Health Care 8.30.2019 *
- Surprise-Billing Law Loophole: When ‘Out of Network’ Doesn’t Quite Mean Out of Network
- Justice for ER patients ‘ambushed’ by bills
- A Mom Owed Nearly $102,000 for Hospital Care. Her State Attorney General Said to Pay Up
- CMS closes thousands of No Surprises Act complaints, directs $4M in relief
- New No Surprises Act Guidance Builds On Recent Final Rule
- DOL FAQ’s
- Issue Brief: Balance Billing Prohibitions and the No Surprises Act
- First Colonoscopy Cost $0. Second Cost $2,185. Why? KHN.org
- His-and-Hers Cataract Surgeries, But His Bill Was 20 Times as Much
- The $18,000 Breast Biopsy: When Having Insurance Costs You a Bundle
- 20% of adults say they’ve received a surprise medical bill despite ban
- Providers are calling for more time to implement estimate requirement in surprise bill rule
- Most U.S. hospitals not sharing price information for joint replacement as required
- 51% OF HOSPITALS STILL NOT ADHERING TO PRICE TRANSPARENCY LAWS
- cms.gov/fact-sheets/surprise-billing
- HHS Announces Rule to Protect Consumers from Surprise Medical Bills
- Federal Agencies Release Interim Final Rule to Implement the No Surprises Act
- LA Times explanation of no surprises act 1.18.2022
- Our webpage on Medical Debt, Bankruptcy & Consumer Guide to Medical Debt
- Providence.org – Difference between Urgent and Emergency Care
- Editorial – East Bay Times 6.23.2016
- dana-farber.org/right to good faith estimate of costs
- stanford health care.org/no-surprises-act * VIDEO *
- Insurers estimate No Surprises Act blocked 2M bills in two months Modern Health Care 5.24.2022
Citations
- 1986 Emergency Medical Treatment and Active Labor Act (EMTALA) CMS.gov (Definition Emergency 2014 Evidence of Coverage Page 80) requires any hospital participating in Medicare (which nearly all do) to provide emergency care to anyone who needs it, the government often indirectly bore the cost of those without the ability to pay.[51][52][53] Wikipedia
- ACA – still problems with balance billing for out of network providers (CA HealthLine 2.18.2015)
- Bisnar Chase Law Firm
- Kaiser Foundation on Balance Billing
- law.uh.edu
- PROSPECT MEDICAL GROUP INC v. NORTHRIDGE EMERGENCY MEDICAL GROUP
- Health & Safety Code 1371.4.
- latimes.com/surprise-medical-bills
- Anthem in some states is not paying for an ER visit if you could’ve gone to urgent care
- Federal Register
Doctors at Hospital #must take hospital negotiated rate
- AB 72, Bonta. on State Website
- Emily Bazar CA Healthline 6.26.2017 Plain Language Explanation
- Pending Legislation to block surprise medical bills 89.3 KPCC 6.20.2016 AB 72
Blue Shield – Announcement
California Assembly Bill (AB) 72 Out-Of-Network Coverage and Member Cost-Sharing
New California law Effective July 1, 2017, this new state law protects individuals from receiving unexpected “surprise or balance” medical bills from an out-of-network (OON) doctor when receiving inpatient and outpatient non-emergency care and services at an in-network healthcare facility such as a hospital, clinic, lab, imaging center or other healthcare facility.
Changes to out-of-network coverage and cost-sharing When individuals go to an in-network facility for care but receive services from an out-of-network doctor or healthcare provider, they only have to pay their in-network cost-sharing amount that counts toward the annual deductible and annual out-of-pocket maximum limits according to their health plan. An out-of-network doctor should only bill individuals after both parties have received a copy of the Explanation of Benefits (EOB) that reflects the correct in-network cost-sharing amount owed for the care received. If for any reason the out-of-network doctor or healthcare provider receives payment that is more than the cost share allowed, the out-of-network doctor must refund the overpayment within 30 days. Below is a list of affected Blue Shield health plans
More explanation from Blue Shield in a private email 8.14.2017
ALL hospitalizations require pre-auth unless they are an emergency. In this pre-auth process, the provider(s) and the Plan are coordinating and acknowledging in-network. This process prohibits people from using out of network providers for procedures ~ If while in the hospital, a person requires additional care that was outside the original scope of the intent, they cannot be charged as out of network. I used anesthesiologist’s as an example in the meeting as it is that issue that we have all been dealing with for years and years.
Members will receive an endorsement letter.
#Advocates Guide to Surprise Medical Bills
- Hidden Cost of Surprise Medical Bills 3.3.2016 Time Magazine
- heart bypass surgery, replacement of one valve and repair of another. raging infection that required powerful IV antibiotics to treat. spent a month in the hospital, some of it in intensive care, before she was discharged home.
- surprise: Bills totaling more than $454,000 for the medical miracle that saved her life. Of that stunning amount, officials said, she owed nearly $227,000 after her health insurance paid its part. Time.com 3.21.2019 *
- heart bypass surgery, replacement of one valve and repair of another. raging infection that required powerful IV antibiotics to treat. spent a month in the hospital, some of it in intensive care, before she was discharged home.
- Newscast about Hospitals being required to post rates - charges VIDEO
- PBS Trump Price Transparency Executive Order VIDEO
- Our webpage on Balance Billing & No Surprises
- Americans often "forced" to pay medical bills they don't owe, feds say CBS News
- Colorado's Supreme Court has ruled in favor of a woman who expected to pay about $1,300 for spinal fusion surgery but was billed more than $300,000 by a suburban Denver hospital that allegedly included charges it never disclosed she might be liable for. Read more: CBS News 5.19.2022
- What the Federal ‘No Surprises Act’ Means in California
- CA Department of Insurance Summary
Specimen Individual Policy #EOC with Definitions
Employer Group Sample Policy
It's often so much easier and simpler to just read your Evidence of Coverage EOC-policy, then look all over for the codes, laws, regulations etc! Plus, EOC's are mandated to be written in PLAIN ENGLISH!
- Find your own Individual EOC Evidence of Coverage
- It' important to use YOUR EOC not just stuff in general!
- Obligation to READ your EOC
- Plain Meaning Rule - Plain Writing Act
- Our Webpage on Evidence of Coverage
- OOP Out of Pocket Maximum - Many definitions are explained there.





https://qz.com/cms-hospital-pricing-rules-1851731141
https://www.dol.gov/agencies/ebsa/about-ebsa/our-activities/resource-center/publications/avoid-surprise-healthcare-expenses
After contacting my providers, it isn’t going to make much difference to them what I am on – Grandfathered or ACA Obamacare, because, unbelievably to me, my present Grandfathered costly plan reimburses them less than Medicare does!
This is a complete reversal of the 90s when my husband’s health insurance switched from private individual market to Medicare. After the switchover to Medicare, I had to fight for his treatment and doctors saw him as a one payment body in a bed. You wouldn’t believe how bad it was, all due to the difference in insurance..
Now I am hearing just the opposite — Medicare has less restrictions on authorizations and better reimbursement than private health insurance! Unfortunately for us seniors the anticipated cuts to Medicare due to the newly passed tax bill could put us right back to the 90s Medicare scenario.
Check our site map and visit our pages on Medicare