Email us for more Information [email protected]
Kaiser Health Plan #Highlights Small Biz
- We are Kaiser Authorized Agents Broker # 5268 and are happy to help you get coverage at no extra charge to you. Kaiser compensates us to help you.
- Appoint us as your Kaiser Broker
- Direct Business ---- Covered CA
- Employer Group [email protected]
- No Extra Charge 17 Reasons how it will benefit you
- Employer Group Quotes
- Individual Quotes & Enrollment - Direct *** Covered CA
Kaiser is like the Xerox of HMO’s, they have been selected as the ACA – Obamacare “Bench Mark” plan. It’s the name that people know. Kaiser has excellent rates and great service. Kaiser compensates us to help you at no additional charge. Our authorized agent code is #5268.
Its a win win for everyone.
Get instant rates and benefits, by using our Complementary, no obligation quote engine, key in your census and have the computer do it or send us an excel spreadsheet
Just Enter your census or securely send us an excel spreadsheet or a list of employees and get instant proposals for California
Health Coverage #Guide
Art Gallagher
Health Care Reform FAQ's
Understanding Health Reform
***********************************
Compliance #Assistance Guide from DOL.Gov Health Benefits under Federal Law
- Health Care Reform Explained Kaiser Foundation Cartoon VIDEO
- Choosing a Health Plan for Your Small Business VIDEO DOL.gov
- ACA Quick Reference Guide California Small Group Employers Revision 2020 Word & Brown
- kff.org/health-policy-101/
Kaiser Small Employer #Administrative Manual
Rev January 2023
- See Administrative Manual for Grace Periods, adding & terminating employees, etc.
- Kaiser Member Resource Guide
- account.kp.org/business/forms-and-documents
Find doctors & locations
- Passport – Access to Care
- Member Resource Guide
- kaiserpermanente.org/get-care/traveling
- Getting care away from home
- get care while away from home. Visit kp.org/travel or call 951–268–3900 for more information.
#Forms
-
- account.kp.org/business/forms-and-documents
- Small Business Group Administration Forms
- Quotit
#Renewal Information
small business service tips on account.kp.org and click on “Making health plan changes at renewal.” Member Tools
Renewal FAQ’s
Kaiser Small Business Employer #Portal Log In Account Services
Video introduction and review training resources for employers and brokers.
- Kaiser’s Customer Account Services website is a powerful tool that will simplify your healthcare administration 24 hours a day, 7 days a week.
- Website quick reference guide
- Sign In
- Enroll/Terminate Employees & Dependents
- Update Membership Information
- View Real-Time Membership
- View Monthly Bill & Six Months of Previous Bills
- Starting August Billing will be ONLINE ONLY, unless you specifically OPT for it!
- View Real-Time Balances & Pay Your Bill Online
- And Much More!
- Get a preview of online account services and use our online account services user ID request form to request access For more information or to schedule your free online training:
- Please email us at: [email protected] or
- call 1-800-731-4661, option 3.
- Please email us at: [email protected] or
#Contact & Service
Who to Contact besides [email protected]:
- California Service Center at [email protected].
- Member Services
- Kaiser Service (800) 789-4661
- Call center @ 800 464 4000 *
- 800 773 1370
- Broker ONLY Portal
- Broker ONLY – Forms Etc.
- • California Service Center at 800-790-4661, option 1, for benefit and eligibility requirements, including membership enrollment/terminations, COBRA, and Medicare/Medicaid
- • Client Services Unit at 800-790-4661, option 2, for open enrollment packets, brochures, contract copies, EOCs and 5500 Schedule A
- • Self-Service Web Support, at 800-790-4661, option 4
- • Broker of Record Changes at 877-762-8247
Kaiser #Member Services
- Kaiser Service – 800 464 4000
- Kaiser Resource Guide
- Wellness & Member Tools
- Kaiser Healthy Life Styles Wellness Programs
- Health Care Reform - Mandated Preventative Care
- For Better Health Management & Prevention
- Care away from home – travel
- healthy.kaiserpermanente.org/southern-california/support
- my.kp.org/caps/easy-online-access/
- Member Portal Set Up
- Welcome to Kaiser
- When you register on kp.org, you'll get access to my health manager—the feature that enables you to take care of your health and view parts of your health record, all in one place*. And that frees up time for the fun stuff.
- Once you register, you can:
- e-mail your doctor's office
- view select test results
- order prescription refills (and have them mailed to you, with free shipping)
- request or cancel routine appointments
- review recent past office visits
- see a list of your recent immunizations and allergies
- act for a family member (e-mail your child's doctor, and more)
- receive our monthly e-newsletter
- When you register on kp.org, you’ll get access to my health manager—the feature that enables you to take care of your health and view parts of your health record, all in one place*. And that frees up time for the fun stuff.
- Broker ONLY - Forms Etc.
Kaiser & Blue Shield
Treatment Cost #Estimator Tool
requires sign in
The tool is for all Kaiser Members that are enrolled on Deductible or Health Savings Account Plans. The cost estimates are for services that are marked "after deductible" to give members an idea of the cost of those services.
- 2021 Kaiser Sample Fee List
- How do I know what level of service I will get billed for?
- BLUE SHIELD Treatment Cost Estimator – for PPO Members
- Cost Helper.com what people are paying for health services
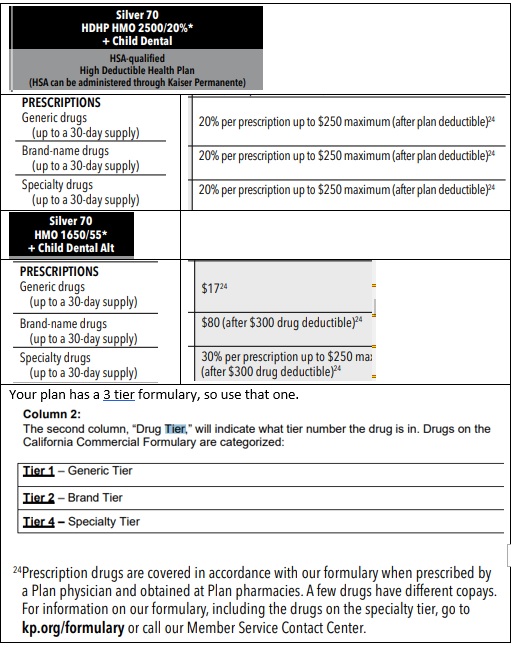
How to find what Medications in the Formulary for #psoriasis
Kaiser Drug Formulary Use the CA Commercial Formulary
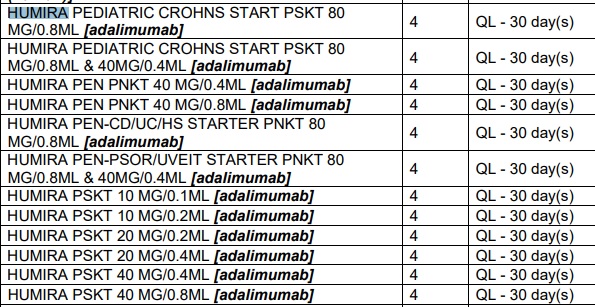
I'm checking to verify if your group has a 2 or 3 tier formulary. Also, we will check the Co-Pays and Tiers for your group...
See plan highlights for general information and your co pays
Your group has the option of The Silver 70 HMO 1650/55 and The Silver 70 HDHP 2500/20% HMO
What do the abbreviations mean?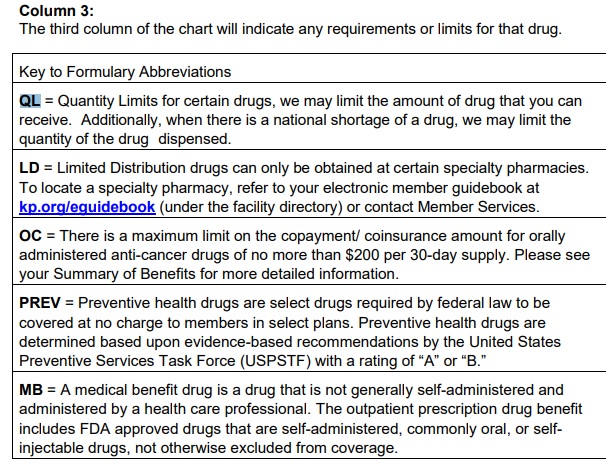
Use Ctrl F to search for the Rx you want to check out
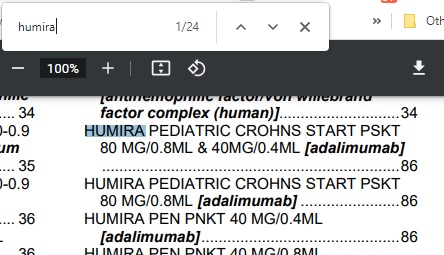
Tier level and quantity level - See highlights above for co pays or just wait till I get the EOC
Just as an FYI - See our webpage Q & A for Medicare Part D Rx on Enbrel & Humira
Taltz list price is $6k/month per their website
Kaiser Small Group Evidence of Coverages
Please review the Formulary Exception Process on page 54
EOC #2 - Kaiser Permanente for Small Business Combined Evidence of Coverage and Disclosure Form for {SAMPLE}Kaiser Permanente Silver 70 HMO 1650/55 + Child Dental Alt INFGroup ID: {PID} EOC Number: 2
See also the EOC on grievances - our webpage on grievances and appeals.
I haven't seen where Metal Level has anything to do with the formulary, in fact it's probably prohibited, as only the co pays and deductibles are supposed to be different. Here's where we did extensive research on Flomax and shouldn't it be covered on a Platinum Plan?
FYI - Medicare Part D has a shopping tool, that tells you at ONE time, all the plans and if they cover what prescriptions - I'm not aware of a feature like that for Small Group or Individual.
Resources & Links
- Kaiser Group Website – Don’t forget, there is no additional charge for us to help you
- Employer – Employee – Forms & Applications (Scroll Down when you get there)
- Covered CA SHOP or
- Cal Choice allows employees to pick whichever Insurance Company or HMO they want
- 15 Reasons to pick Steve Shorr Insurance
- Point of Service plan – allowing you to visit PPO Doctors with the PHCS Network – Provider Search
- Click here for a simple explanation of the Four Metal Tiers and the 10 essential benefits. Please note that ACA – Obamacare does NOT include Adult Dental, Long Term Care or Disability Income.
-
- Broker ONLY – Forms Etc.
Broker ONLY
- 2025 Small Group Plan Highlights
- Quality care in Monterey
- Mental health and wellness care resources
- Broker resources
- https://account.kp.org/business/plans-listing/small-business
- https://account.kp.org/business/california/small-business/plan-rates-and-highlights
- https://account.kp.org/business/forms-and-documents
- https://account.kp.org/business/broker/california/client-support/renewals/small-business-renewal-information
- https://account.kp.org/content/dam/kp/bcssp/shared/ca/documents/working-with-kp/2025/sb-medicare-creditable-coverage-ca-en-2025.pdf
- https://account.kp.org/business/broker/california/working-with-kp/compliance/kaiser-permanente-policies
- https://account.kp.org/business/broker/california/marketing-and-sales-materials/small-business
- https://account.kp.org/content/dam/kp/bcssp/shared/ca/documents/resource-library/2025/sb-sales-portfolio-snapshot-ca-en-2025.pdf
- https://account.kp.org/business/shared/ca/plans/2025/sb-simplifying-health-care-for-small-businesses-brkr-fillable-ca-en-2025.pdf
- https://account.kp.org/business/plans-listing/small-business
- https://account.kp.org/business/forms-and-documents





https://business.kaiserpermanente.org/california/healthy-employees/innovation/employee-health-innovations-resource
https://business.kaiserpermanente.org/california/healthy-employees/innovation/virtual-care-healthy-workforce
https://business.kaiserpermanente.org/california
https://www.cms.gov/marketplace/about/oversight/other-insurance-protections/prescription-drug-data-collection-rxdc
https://account.kp.org/business/broker/california/news-and-announcements/2024/pharmacy-reporting-rxdc-frequently-asked-questions
https://account.kp.org/business/broker/california/news-and-announcements/2025/get-care-support-southern-california-wildfires
https://healthy.kaiserpermanente.org/southern-california/alerts/southern-california-fires
What medications are in the formulary for psoriasis?
Enbrel,
Humira,
Stelara,
Talz, and others
See FAQ Above