Medicare coverage of Hospice, Palliative & respite care
What about Medi Gap, Medicare Advantage & ACA/Obamacare?
Official Medicare #Hospice Publication # 02154 

- Palliative Care VIDEO
- Palliative care, which focuses on providing relief from the symptoms and stress of serious illness, offers an extra layer of support. Learn more at chcf.org
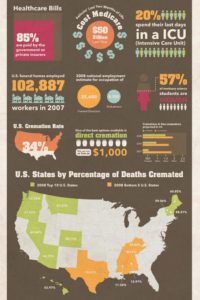
Costs of the last 2 months of life
See our webpage on
- Long Term Care
- Final Expense Policies
- Hospice End of Life Care
- Set a Zoom Meeting
- Our main webpage on Hospice
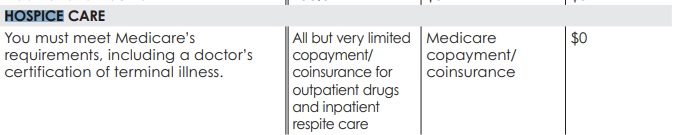
Hospice Coverage
Introduction
Hospice is a program of care and support for people who are terminally ill (with a life expectancy of 6 months or less, if the illness runs its normal course) and their families. Here are some important facts about hospice:
■ Hospice helps people who are terminally ill live comfortably.
■ Hospice isn’t only for people with cancer.
■ The focus is on comfort (palliative care), not curing an illness.
■ A specially trained team of professionals and caregivers provide care for the “whole person,” including physical, emotional, social, and spiritual needs.
■ Services typically include physical care, counseling, drugs, equipment, and supplies for the terminal illness and related conditions.
■ Care is generally given in the home.
■ Family caregivers can get support.
To qualify for hospice care, a hospice doctor and your doctor (if you have one) must certify that you’re terminally ill, meaning you have a life expectancy of 6 months or less. When you agree to hospice care, you’re agreeing to comfort care (palliative care) instead of care to cure your illness. You also must sign a statement choosing hospice care instead of other benefits Medicare covers to treat your terminal illness and related conditions. Publication 02154
Depending on your terminal illness and related conditions, the plan of care your hospice team creates can include:
any or all of these services:
- Doctor services
- Nursing care
- Medical equipment (like wheelchairs or walkers)
- Medical supplies (like bandages and catheters)
- Prescription drugs for symptom control or pain relief
- Hospice aide and homemaker services
- Physical therapy services
- Occupational therapy services
- Speech-language pathology services
- Social work services
- Dietary counseling
- Grief and loss counseling for you and your family
- Short-term inpatient care (for pain and symptom management)
- Short term respite care
- Any other Medicare-covered services needed to manage your pain and other symptoms related to your terminal illness and related conditions, as recommended by your hospice team medicare.gov/hospice-care
- When you choose hospice care, you decide you no longer want care to cure your terminal illness and/or your doctor determines that efforts to cure your illness aren’t working.
- How Well Does Medicare Cover End-of-Life Care? It Depends on What Type
A new study analyzed the experiences of more than a million patients in their final months of life. University of Colorado 7/2024
Medicare won’t cover any of these once your hospice benefit starts:
- Treatment intended to cure your terminal illness and/or related conditions. Talk with your doctor if you’re thinking about getting treatment to cure your illness. As a hospice patient, you always have the right to stop hospice care at any time.
- Prescription drugs to cure your illness (rather than for symptom control or pain relief).
- Care from any hospice provider that wasn’t set up by the hospice medical team. You must get hospice care from the hospice provider you chose. All care that you get for your terminal illness must be given by or arranged by the hospice team. You can’t get the same type of hospice care from a different hospice, unless you change your hospice provider. However, you can still see your regular doctor or nurse practitioner if you’ve chosen him or her to be the attending medical professional who helps supervise your hospice care.
- Room and board. Medicare doesn’t cover room and board if you get hospice care in your home or if you live in a nursing home or a hospice inpatient facility. If the hospice team determines that you need short-term inpatient or respite care services that they arrange, Medicare will cover your stay in the facility. You may have to pay a small copayment for the respite stay.
- Care you get as a hospital outpatient (like in an emergency room), care you get as a hospital inpatient, or ambulance transportation, unless it’s either arranged by your hospice team or is unrelated to your terminal illness and related conditions. medicare.gov/hospice-care
Contact your hospice team before you get any of these services or you might have to pay the entire cost.
Resources & Links
- NPR Home Hospice can be tough on families 1.21.2020
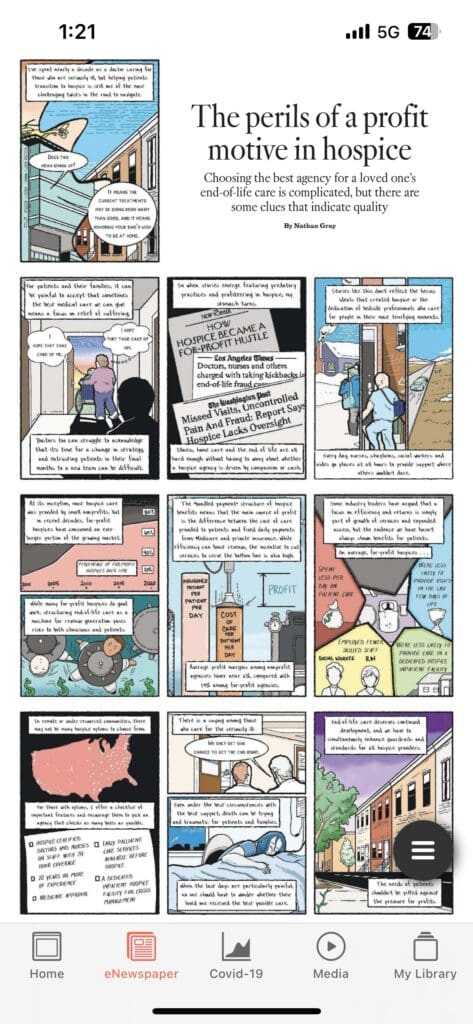
- Southern California doctor sentenced to prison in multimillion-dollar hospice fraud scheme LA Times 12/2024
Contact Us - Ask Questions - Get More Information - Schedule a Zoom Meeting
[email protected]
By submitting the information below , you are agreeing to be contacted by Steve Shorr a Licensed Sales Agent by email, texting or Zoom to discuss Medicare or other Insurance Plans as relevant to your inquiry. This is a solicitation for Insurance
Your costs in Original Medicare
- $0 for hospice care.
- You may need to pay a copayment of no more than $5 for each prescription drug and other similar products for pain relief and symptom control while you’re at home. In the rare case your drug isn’t covered by the hospice benefit, your hospice provider should contact your Medicare drug plan to see if it’s covered under Part D Rx
- You may need to pay 5% of the Medicare-approved amount for inpatient respite care.
- Medicare doesn’t cover room and board when you get hospice care in your home or another facility where you live (like a nursing home).
- If you pre planned got Long Term Care or Home Health Care those may.
To find out how much your test, item, or service will cost, talk to your doctor or health care provider. The specific amount you’ll owe may depend on several things, like:
- Other insurance you may have
- Medi Gap, Medicare Advantage?
- How much your doctor charges
- Whether your doctor accepts assignment
- The type of facility
- Where you get your test, item, or service medicare.gov/hospice-and-respite-care
Your Costs in Hospice
Long Term Care Coverage
Hospice, Euthanasia, Links & Resources
- LA Times – Hospice and caring for spouses 12.22.2014
- Hospice Information – Fraud Scams – CA Health Care Advocates
- Medicare Hospice Benefit. What it is, and is not. Don’t Fall for the “sales pitch”!
- Thursday, November 16, 2023 » View Webinar » View Slides, Sample Questions for Hospices, Q&A » View Survey
- Medicare Hospice Benefit & What It’s Not
- April 27, 2023 » View Webinar » View Slides
- Understanding the Medicare Hospice Benefits
- September 22, 2022 » View Webinar » View Slides
This webinar goes over:- What hospice is and what it is not
- How to access the hospice benefit
- Avoid being a victim of hospice fraud
- September 22, 2022 » View Webinar » View Slides
- How Well Does Medicare Cover End-of-Life Care? It Depends on What Type
A new study analyzed the experiences of more than a million patients in their final months of life. Anschutz School of Medicine - How to Prevent Hospice Fraud
- October 24, 2019 » View Webinar » View Materials: SMP slides; Judy Thomas’ slides; Sheila Clark’s slides; hospice infographic
- Southern California doctor sentenced to prison in multimillion-dollar hospice fraud scheme LA Times *
- Medicare Hospice Benefit. What it is, and is not. Don’t Fall for the “sales pitch”!
- Find hospice care
- Los Angeles times opinion on hospice at home doctor-patients-send-home-to-die
- Medicare Home Health Cuts Could Have Ripple Effect on Hospice, Palliative Care
- Hospices in Four States to Receive Extra Scrutiny Over Concerns of Fraud, Waste and Abuse
- A service is “medically necessary” or a “medical necessity” when it is reasonable and necessary to protect life, to prevent significant illness or significant disability, or to alleviate severe pain. (2014 ACA Sample EOC Page 166) CA WIC §14059.5
- Compare & Contrast Palliative & Hospice Care NIH.Gov
- hospice news.com/medicare-home-health-cuts-could-have-ripple-effect-on-hospice-palliative-care
- My Place Heath (SCAN?)
- myPlace Health specializes in providing value-based, comprehensive care and coverage for older adults with significant needs so they can thrive in the homes they love and in the communities they cherish. Our myPlace PACE (Program of All-Inclusive Care for the Elderly) model provides seamless primary care, integrated health plan coverage, personalized social engagement, and customized services – all at no cost if you are eligible for Medi-Cal or both Medicare and Medi-Cal.
- Medicare Processing Manual – Hospice Claims 78 pages
- y Jewish Learning.com hospice & palliative care
- Chabad Redondo Beach Facebook Live – you don’t need a Facebook account Jewish Perspective on End of Life Care
- Hospice Reform in CA
- California revises the End of Life Option Act. Supporters say the new law removes ‘bureaucratic barriers.’ LA Times
- cedars-sinai.org/ca-aid-in-dying-law
- ucla health.org/california-end-life-option-act
- ‘Disturbing’: Experts troubled by Canada’s euthanasia laws
- The Clinical, Ethical and Legislative Case for Medical Aid in Dying in New York
- Making it easier for dying people to die Euthanasia
- California Hospice Licensure and Oversight Auditor State of CA March 2022*
- Medical Assistance in Dying in Canada 2023 Canada.Ca
- How to get death certificate if someone dies at home
CA Dept of Aging – Home & Long Term Care Booklet
Please note, there are updates all the time, double check everything.
#Taking Care of Tomorrow Booklet
NAIC Shoppers Guide to Long Term Care
Skilled Nursing Homes
How does Medicare pay for #SkilledNursing Homes - 10153 11359
Our Introductory You Tube VIDEO based on this manual
- Your costs for Skilled Nursing in Original Medicare You pay:
-
Days 1–20: $0 for each benefit period .
- Days 21–100: $194.50 coinsurance per day of each benefit period.
-
Days 101 and beyond: All costs. Medicare.gov *
-
- Clinical Guidelines explain the coverage so much better and in logical order!
- The two-midnight rule and Medicare Advantage: 7 updates Beckers Payer.com 2/2024
- Medi Cal Payments Fall Far Short of Covering Care Costs at Nursing Homes Skilled Nursing News.com 11/2024
- Medicare's VIDEO Nursing Home / Long-Term Care
- Planning for Discharge from a Health Care Setting VIDEO
- Long Term #Acute Care Publication # 11347
- Long-Term Acute Care Hospital (LTACH) Clinical Guidelines - Oscar
- Differences between Skilled Nursing, Long Term Acute Care & Inpatient Rehabilitation Facility
- Our FAQ on Sub Acute Care
- Find & compare nursing homes, hospitals & other providers near you Medicare.Gov
- Learn more about providers
- Calculate Cost of Long Term Care in your Area Genworth
- "Hospital at Home" Programs Improve Outcomes, Lower Costs But Face Resistance from Providers and Payers
- Pro Seniors Medicare & Skilled Nursing
- Medicare doesn't pay for:
- Our Webpagse on Long Term Care
Anthem Medicare Supplement - Get Quotes, Information and ONLINE Enrollment - No extra charge for our help