What is the MLR – Medical Loss Ratio Rule
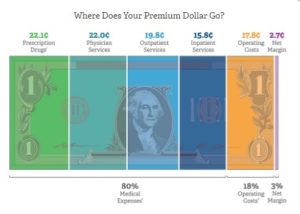
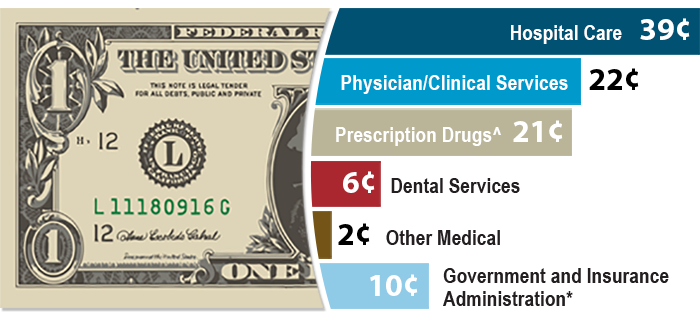
80% to claims – 20% Administrative & Profit
Definition & Explanation
MLR – Medical Loss Ratio Rule
The MLR – Medical Loss Ratio Rule requires Insurance Companies to at least spend 80 percent of premium dollars on medical services – claims, over all, not on each policyholder. If they don’t, they have to give refunds – rebates. * CMS.Gov * NAIC * (health care.gov) Thus, a higher premium plan MUST pay more in claims, a lower premium plan, can cut claims… by decreasing benefits such as,
- deductibles,
- co-pays,
- limiting the number of doctors you can see – narrow networks,
- metal levels and
- limited Rx formularies.
- FYI UHC & Anthem Medicare Advantage Plans in 6 states got suspended for not following the MLR Rule! Modern Health Care *
- the medical loss ratio rule, was touted by the Obama administration as a tool for lowering premiums, but in the long run, it may be having the opposite effect. Modern Health Care 3.14.2020
- Why insurers are cutting broker pay for exchange plans Adverse selection – Open Enrollments Modern Health Care 4.13.2022
- Risk Adjustment in Medicare Advantage
- California Health Care Foundation MLR Resources
Do your part to keep costs down by
- watching your weight,
- preventative care
- Social Distancing
- Who pays for rioting & looting?
- and wellness programs
- COVID Precautions – Hospitalizations Payments may increase rates! Vaccinations? InsureMeKevin.com
- BROKER ONLY – Warner Pacific
- proposed Office of Health Care Affordability AP News 3.14.2022
What’s on this page?
Medical Loss Ratio 80% Claims - 20% Operating Costs & Profit
Image from BCBS.com
Steve's Explanation of MLR Medical Loss Ratio
More Video's
- Kaiser Health News - Medical Loss Ratio
- Department of Managed Health Care on MLR in Affordable Care Act
- White House – YouTube Channel on Health Care Reform
- Tom Petersen Insurance 101 History of Lloyds to present EXCELLENT!!!
- Our Webpage on MLR & Actuarial Value
Rebates – You get a refund if the Insurance Company
collected too much $$$ to pay 80% of premium in Claims
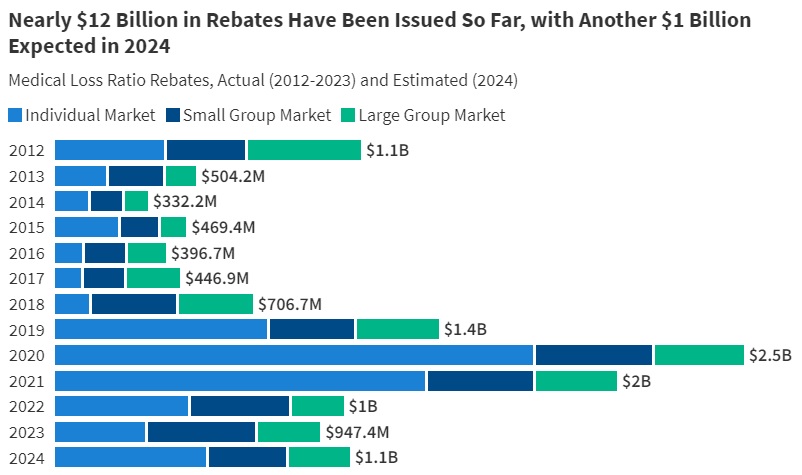
#Rebates Return of Excess Premium
- Anthem 2023 Rebates

- Source KFF
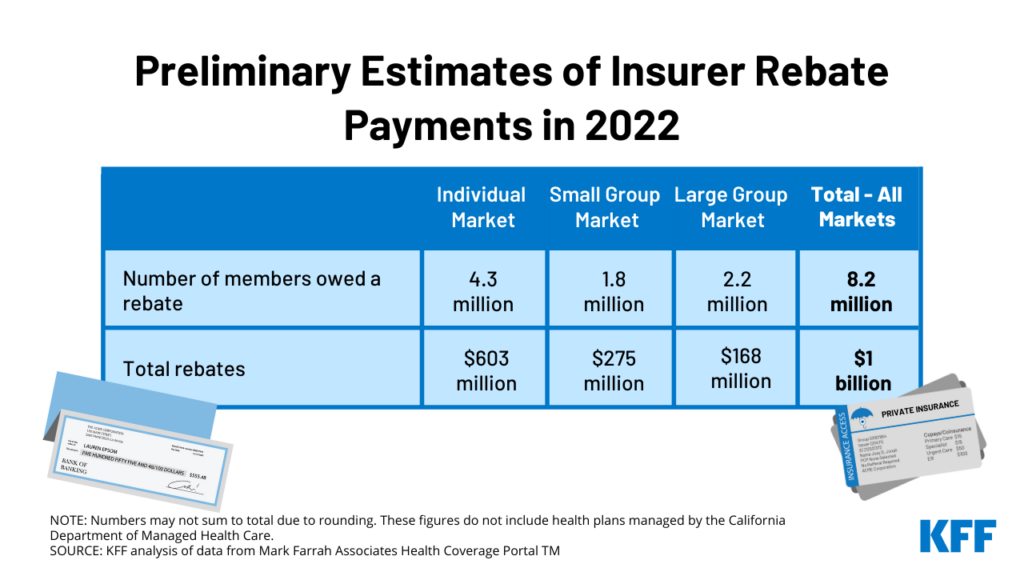
- $1 Billion in Rebates to for 2022 for Setting Premiums Too High Relative to Medical Costs Read More CNBC * Kff.org

- roughly $141 per plan member in the individual market,
- $155 per member in the small group market and
- $78 per member in the large group market, Kff.org
- UHC United Health Care show great profits during pandemic LA Times 10.15.2020 *
- FAQ on how to distribute rebates to employees
- Blue Cross Group Rebates for 2019 *** FAQ’s
- Tools & Research to find MLR Medical Loss Ratio
- Covered CA *
- CMS.gov *
2019 Rebates
Aetna
- aetna.com/affordable-care-act-employers
- Then click on “Minimum Medical Loss Ratio”
- What states are getting Rebates?
- What types of plans are getting rebates?
Industry
Insurers will owe massive MLR rebates next year, even if 2020 is normal Modern Health Care *
There might be rebates for 2018
Kaiser Family Foundation, in a report published this week, said 2018 was “the most favorable year in the ACA-compliant market’s history.” The insurers were so profitable, in fact, that they’ll have to rebate a record $800 million in overcharges to consumers by Sept. 30. The expectation, however, was that the market would eventually stabilize. That’s exactly what has happened. Financial conditions in the individual market began to improve in 2016, when average premiums first began to outpace claims. By last year, when average monthly premiums per enrollee were $559, they outpaced average per capita claims by $167. * Los Angeles Times 5.8.2019 *
Due to some better-than-expected claims results, along with cost-saving measures that have been implemented, Anthem’s Medical Loss Ratio (MLR) dropped below 80% over the 2015-2017 period.
What does this mean? It means that Anthem clients who were enrolled in the 2017 calendar year are getting some money back.
- The annualized rebates will average approximately $142 per member over a 12-month period.
- The rebate checks are distributed directly to the employer and should be sent by September 8th.
- The employer has the option to distribute the rebate to employees or apply it toward future premiums.
- Cal-COBRA members will receive a check directly from Anthem.
- Anthem is required to inform employees that their employer is receiving a rebate. Employee letters are required to be mailed and will be sent by September 18th.
Anthem is committed to providing access to high-quality health care providers and services while working to drive down cost in the health care system. In addition, Anthem is striving to improve its customers’ experience, and efficiently managing their costs is part of that experience.
- Blue Shield – Employer Rebates 11.1.2016 CA Health Line
- Blue Shield accused of not giving high enough rebates for 2014 – LA Times 6.28.2016 – Lawsuit filed CA Health Line 7.18.2016 * 9.20.1206 Talking points for Small Biz Rebates for 2015
- The LA Times reports on 8.5.2015 that Blue Shield (talking points) will pay out $83 million for 2014 an average of $136/policy holder and $21 million to 19,000 small employers, about $1,000.
- Health Net 2014 results – no rebates
- CA Companies appear to have fine tuned their premiums and claims to meet the MLR Rule and do not have to refund any money for 2013 (Word & Brown Survey) Learn More in Blue Cross Presentation.
- Rebates were expected to be 1.3 Billion in 2012!LATimes 4.27.2012 The Hill 5.2014 $332 Million in 2013 – as companies are fine tuning their rates to comply with the rule. Modern Health Care United Health Care has announced a $3,500,000 refund to CA Small Biz. Blue Cross, Blue Shield & Kaiser $50 million LA Times 6.2.2012 Nor, no one can say that Insurance is a Scam, it’s simply a mechanism to share the losses. If you want to pay less premium and are willing to take more of the risk yourself, avoid the 20% “handling charge,” take the Bronze Plan, where you pay 40% of the essential covered benefits. Click here for more info from United Health Care
- Blue Shield is voluntarily limiting net income to 2% and giving refunds.
- Merced Property & Casualty Co out of biz due to Paradise Camp Fire LA Times 12.3.2018 *
Testimonials & Accolades
Thank you so much for your assist in navigating this complicated insurance process.
I feel so lucky to find you!
I would like to contact you if I have any questions in the future because you are the only one who can give me a clear answer in this field.
I really, really appreciate you. 🙏
Julie L
Read our other clients testimonials and/or write one
Actuarial Value
What is #actuarial value and how does it affect premiums?
The actuarial value of a health insurance policy is the percentage of the total covered expenses that the plan covers, on average for a typical population. [Age & Zip Code] For example, a plan with a 70% Silver actuarial value means that consumers would on average pay 30% of the cost of health care expenses through features like deductibles and coinsurance. The amount that each enrollee pays will vary substantially by the amount of services they use.
The health reform law specifies a benchmark level of coverage for the purposes of premium subsidies using actuarial values. Premium subsidies will be tied to Silver plans, which have an actuarial value of 70%. Additional subsidies for people making between 100 and 250% of the poverty level limit cost sharing and raise the actuarial value of Silver plans. Our calculator also illustrates premiums and subsidies for Bronze plans, which have an actuarial value of 60%. Bronze plans represent the minimum level of coverage most people are required to maintain under health reform, and these plans will have higher cost sharing on average. Regardless of the level of actuarial value, insurers will have to cover a defined set of health care services and cap the total amount of cost sharing required of consumers at defined levels, but can generally otherwise vary the structure and degree of cost sharing so long as minimum actuarial value thresholds are met.
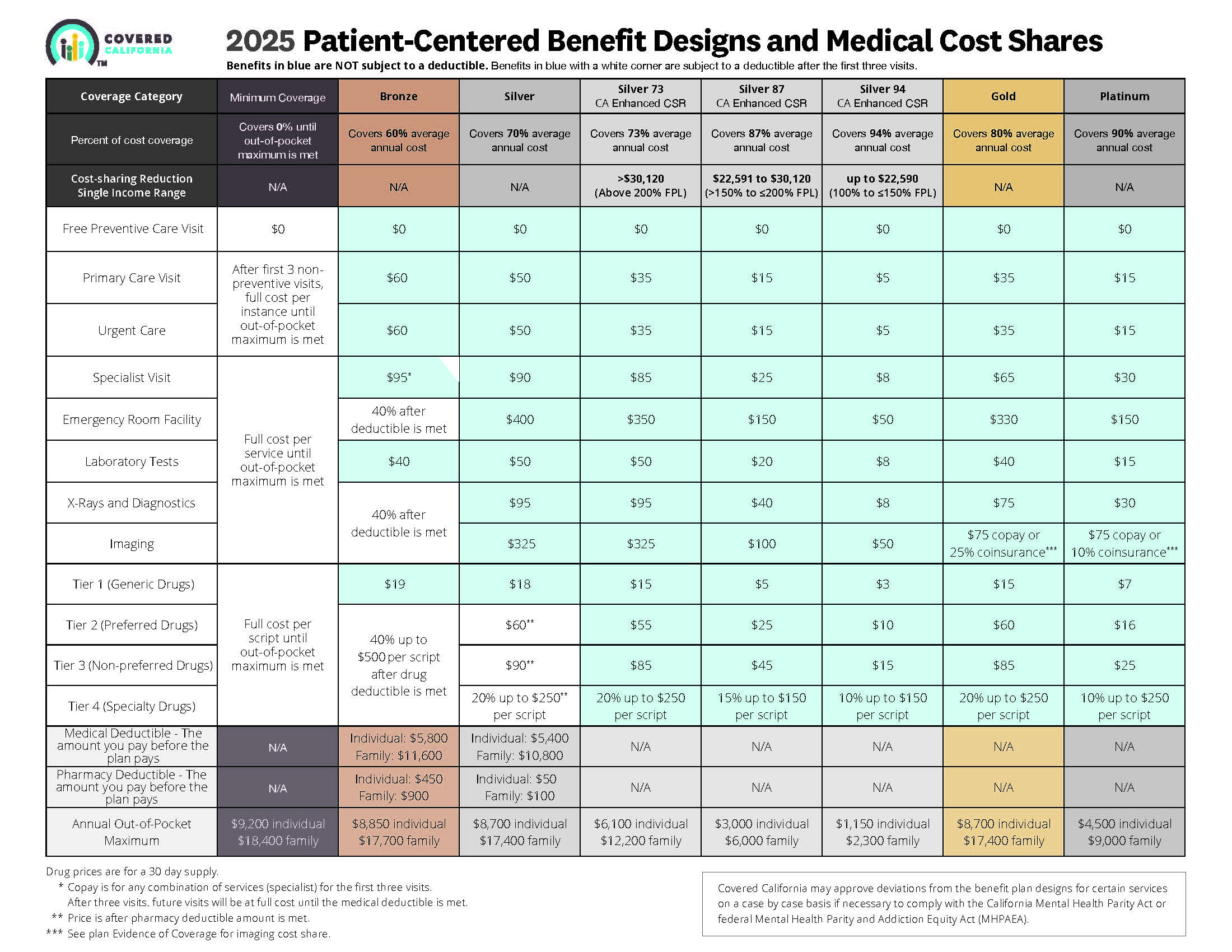
- Graphic Summary of the four metal levels & percent of cost of coverage
- 45 CFR 156.140 Metal Levels of Coverage
- Kaiser Foundation 6 page pdf summary
Market Stabilization
Guide to the Rule Making Process 11 pages pdf
Metal Level Chart showing Actuarial Value
- 2025 Source
- Source and see a sharper image 2024 Patient Centered Designs * *
- Covered CA bulletin on new and improved Enhanced Silver CSR Cost Sharing Reduction
- Do you think your medical bills will be higher or lower than average for your age & zip code?
- Expected Payout (AV)
- MLR Medical Loss Ratio
- Bronze 60%
- Enhanced Silver 70% - 94% Gold 80% Platinum 90%
- Metal Levels are based on Expected Claims Payment - that is the actuarial value (AV).
- Renewal Tool Kit
- Did you notice LOWER deductibles & Co Pays???
- This is one way Health Care Reform hopes to make shopping and comparing Instantly - easier. So, if you get a lower priced plan with less or fewer benefits, co-pays, deductibles you simply pay more when you have a claim. Don't worry, there is a stop loss - maximum out of pocket OOP, of say $7k so that you won't break the bank.
- All plans cover the 10 Federal essential benefits and CA mandated benefits.
- Our main webpage on Metal Levels
Agents Role
The #Agents Role – Part in the Medical Loss Ratio Calculation
MLR (Medical Loss Ratio) define their commissions as part of the medical expense and failed. The argument by insurance agents was a senseless argument. healthcare exchanges under the new law.
These exchanges are not yet up and running but it is easy to picture them to be akin to Amazon.com (AMZN) by necessity and by law, insurance companies will have to display their products in easy to understand and easy to compare formats. In some ways, the migration will be similar to the migration of retail from the likes of Best Buy (BBY), Barnes & Noble (BKS), and Borders to Amazon.com. At least in retail there are numerous good reasons for the masses to go to the brick and mortar stores. With regard to health insurance the argument for procurement through agents is very weak. Forbes
The hope of the insurance agents had risen because of the recent backing by the National Association of Insurance Commissioners.
In a recent ruling, the Department of Health and Human Services dashed all hopes.
Now the only hope left is H.R.1206, the Professional Health Insurance Advisors Act, a pending bill in Congress that would exclude compensation paid to independent insurance producers for the purposes of MLR.forbes.com
THE MEMBERS OF THE NATIONAL ASSOCIATION OF INSURANCE COMMISSIONERS, THEREFORE RESOLVE THAT:
Congress should expeditiously consider legislation amending the MLR provisions of the PPACA in order to preserve consumer access to agents and brokers, and;
The Department of Health and Human Services should take whatever immediate actions are available to the Department to mitigate the adverse effects the MLR rule is having on the ability of insurance producers to serve the demands and needs of consumers and to more appropriately classify producer compensation in the final PPACA MLR rule. naic.org
The insurer has no incentive to operate more efficiently or to reduce premiums. Companies would pay brokers as much or as little as they want because any amount would be paid from increased premiums, and the 7.2 points of “excess” MLR could be shaved to please investors by further raising premiums.
The impact of the broker payment exclusion cannot be considered in a vacuum.
If broker commissions are not subject to those limits, insurance companies have every incentive to shift as much administrative burden to brokers as they can, because broker commissions would be subject to no limits. naic.org/
Loss of Agent Services under Health Care Reform? Forbes 6.29.2012
https://www.scpr.org/news/2015/04/29/51313/some-brokers-encounter-hard-times-under-the-afford/
All our plans are Guaranteed Issue with No Pre X Clause
Quote & Subsidy #Calculation
There is No charge for our complementary services
Watch our 10 minute VIDEO
that explains everything about getting a quote
- Our Quote Engine Takes all the complexity out of using pencil and paper to figure out the premiums per the Obamacare/ACA rules under CFR §1.36B-3 *
- Get more detail on the Individual & Family Carriers available in CA
Actual Law, Regulations and more detail
General highlights of the regulations include:
- Rate Increases must be certified by an Actuary CA SB 1163 New Ballot Measure Prop 45 requires Deparment of Insurance Approval
- MLR (Medical Loss Ratio)rebates will be sent to policy holders,which include employers or employee organizations as well as individual plan policyholders.
- Insurers may distribute rebates to employers; in turn, employers would need to issue rebates to employees, based on employee contributions.
- Policyholders are potentially eligible for a rebate determined on a “block” basis. The “block”is defined by:
- Organization size (individual; small or large employer group)
- Legal entity issuing coverage
- State of issuance
- Limited medical and expatriate international plans handled separately
- Small group is defined as 2-50 employees unless a state defines it differently until at least 2016.
- For the 2011 reporting year, issuers of limited medical (mini-med) and expatriate international plans are subject to separate calculation rules.
- The plan’s numerator of the total claims incurred and expenditures for activities that improve health care quality would be multiplied by two.
- Carriers will be required to complete additional quarterly reporting through 2011.
- After reviewing this additional reporting, these adjustments will be revisited by the Secretary for 2012 and beyond.
- Broker commissions will be included in the MLR calculation.
- Non-U.S. insurance companies do not file MLR.
A preliminary analysis of the regulation and the data from this survey support four key points:
- Initial compliance costs (especially accounting, auditing, and contracts with providers and employers) will likely exceed the estimates that accompanied the regulation by a substantial amount for many health plans.
- Plans serving the individual and small-group markets are the most likely to be affected.
- There is no guarantee that the federal MLR rule will lower health costs and premiums. In fact, the incentives under the rule may lead to higher administrative costs, higher-cost benefits, and higher premiums.
- The rule could reduce the number of health plans competing in some markets. ahip hi wire.org Like Aetna and PacifiCare leaving the CA Individual Market
The rate review regulation process
Consumer Resources
- CMS.Gov on MLR
- Insure Me Kevin.com – How are premiums determined 3.9.2017
- Patient Protection and Affordable Care Act (PPACA)
- Government Tool to find out about Rate Increases or Loss Ratio for each Insurance Company
- health care.gov FAQ Value for Premium $$$
- Health Net paid the minimums in 2011 and will not be sending rebates Aetna met minimums in CA
- YouTube Channel
- Blue Cross Memo on MLR – Medical Loss Ratio’s
#Insubuy Travel Health Insurance
Instant Quotes, Details and ONLINE Enrollment
Steve talks about International Travel Insurance VIDEO
US State Department - Travel - Insurance
Our webpage on Travel Insurance
#Code of Federal Regulations (CFR)
PART 158—ISSUER USE OF PREMIUM REVENUE: REPORTING AND REBATE REQUIREMENTS
Proposed Rules CMS 9930 P 10.27.2017
Contents
§158.101 Basis and scope.
§158.102 Applicability.
§158.103 Definitions.
Subpart B—Calculating and Providing the Rebate
§158.210 Minimum medical loss ratio.
§158.211 Requirement in States with a higher medical loss ratio.
§158.220 Aggregation of data in calculating an issuer’s medical loss ratio.
§158.221 Formula for calculating an issuer’s medical loss ratio.
§158.230 Credibility adjustment.
§158.231 Life-years used to determine credible experience.
§158.232 Calculating the credibility adjustment.
§158.240 Rebating premium if the applicable medical loss ratio standard is not met.
§158.241 Form of rebate.
§158.242 Recipients of rebates.
§158.243 De minimis rebates.
§158.244 Unclaimed rebates.
§158.250 Notice of rebates.
§158.251 Notice of MLR information.
§158.260 Reporting of rebates.
§158.270 Effect of rebate payments on solvency.
Regulations
- December 1, 2010 OCIIO–9998–IFC: Health Insurance Issuers Implementing Medical Loss Ratio (MLR) Requirements Under the Patient Protection and Affordable Care Act – Opens in a new window (PDF – 2 MB)
- Technical Appendix Interim Final Rule for Health Insurance Issuers Implementing Medical Loss Ratio (MLR) Requirements under the Patient Protection and Affordable Care Act (PDF – 300 KB)
- Technical Correction (December 30, 2010) Technical Correction to the Medical Loss Ratio Interim Final Rule – Opens in a new window (PDF – 59 KB)
- December 7, 2011 CMS-9998-FC: Medical Loss Ratio Requirements under the Patient Protection and Affordable Care Act – Opens in a new window CMS-9998-IFC2: Medical Loss Ratio Rebate Requirements for Non-Federal Governmental Plans – Opens in a new window
- May 16, 2012 CMS-9998-F: Medical Loss Ratio Requirements under the Patient Protection and Affordable Care Act – Opens in a new window
- May 16, 2012 CMS-9998-IFC3: Medical Loss Ratio Requirements under the Patient Protection and Affordable Care Act; Correcting Amendment – Opens in a new window
- November 30, 2012 CMS-9964-P: HHS Benefit and Payment Parameters for 2014, and Medical Loss Ratio – Opens in a new window
- March 11, 2013 CMS-9964-F: HHS Benefit and Payment Parameters for 2014 – Opens in a new window
Guidance
- December 17, 2010 OCIIO Technical Guidance: Process for a State to Submit a Request for Adjustment to the Medical Loss Ratio Standard of PHS Act Section 2718 (PDF – 35 KB)
- April 26, 2011 CCIIO Technical Guidance: Submission of 2011 Quarterly Reports of MLR Data by Issuers of “Mini-med” and Expatriate Plans (PDF – 26 KB)
- May 13, 2011 CCIIO Technical Guidance: Questions and Answers Regarding the Medical Loss Ratio Interim Final Rule (PDF – 75 KB)
- May 19, 2011 CCIIO Technical Guidance: Deadline for Submission of 2011 First Quarter MLR Data by Issuers of “Mini-med” and Expatriate Plans (PDF – 26 KB)
- July 18, 2011 CCIIO Technical Guidance: Questions and Answers Regarding the Medical Loss Ratio Interim Final Rule (PDF – 66 KB)
- February 10, 2012 CCIIO Technical Guidance: Questions and Answers Regarding the Medical Loss Ratio Interim Final Rule (PDF – 94 KB)
- March 30, 2012 Memo to Insurance Companies: Medical Loss Ratio Annual Reporting Procedures (PDF – 96 KB)
- April 20, 2012 CCIIO Technical Guidance: Questions and Answers Regarding the Medical Loss Ratio Regulation (PDF – 101 KB)
- May 15, 2012 Memo to Insurance Companies: Guidance for Medical Loss Ratio Annual Reporting Form (PDF – 66 KB) Memo to Insurance Companies: Guidance for Medical Loss Ratio Notices of Rebates (PDF – 67 KB)
- May 24, 2012 CCIIO Technical Guidance: Questions and Answers Regarding the Medical Loss Ratio Reporting Form (PDF – 91 KB)
- May 30, 2012 CCIIO Technical Guidance: Questions and Answers Regarding the Medical Loss Ratio Reporting Requirements (PDF – 83 KB)
- July 17, 2012 CCIIO Technical Guidance: Questions and Answers Regarding the Medical Loss Ratio Reporting and Rebate Requirements (PDF – 69 KB)
- March 29, 2013 Memo to Insurance Companies: Guidance for 2012 Medical Loss Ratio Annual Reporting Form (PDF –119 KB) Memo to Insurance Companies: Announcement Regarding Training for 2012 Medical Loss Ratio Reporting Period (PDF – 125 KB)
- April 5, 2013 CCIIO Technical Guidance: Questions and Answers Regarding the MLR Reporting and Rebate Requirements (PDF – 139 KB)
- May 30, 2013 CCIIO Technical Guidance: Question and Answer Regarding the Requirement that Issuers of Certain Health Insurance Coverage Sold as Fixed Indemnity Insurance Submit an Annual Medical Loss Ratio (MLR) Report to the Secretary (PDF – 89 KB)
- July 2, 2013 CCIIO Technical Guidance Questions and Answers Regarding the Medical Loss Ratio Reporting and Rebate Requirements [PDF, 109KB]
- December 30, 2013 CCIIO Technical Guidance (CCIIO 2013—0004): Question and Answer Regarding the Medical Loss Ratio Reporting and Rebate Requirements [PDF, 120KB]
Nearly 4,400 small businesses in California will share in $3.5 million in rebates from insurance giant UnitedHealth Group
about $98 each for nearly 36,000 small-business employees and dependents
Other companies are expected to disclose the size of their customer rebates later this week and send out money by Aug. 1.
Under the federal and state laws, insurers must spend at least 80% of premiums collected on medical care for individual and small-group policies, which cover businesses with 50 or fewer workers
it’s up to employers to decide how they share those savings under the federal law. Some employers may split the rebate money based on the percentage workers contribute to their annual premiums or they could reduce next year’s premium by a similar amount.
but the rules don’t address the larger issue of rising medical costs.
“Rebates are one way to adjust the price of insurance,” Johnston said, “but the bigger issues are containing cost and extending coverage.”latimes.com






https://www.cms.gov/medicare/health-drug-plans/medical-loss-ratio
I want to figure out how to distribute rebate to employees
The DOL provides three options for distributing rebates:
Reduce subscribers’ portions of the annual premium for the subsequent policy year for all subscribers covered under any group health policy offered by the plan.
Reduce subscribers’ portions of the annual premium for the subsequent policy year for only those subscribers covered by the health policy on which the rebate is based.
Provide a cash refund only to subscribers who were covered under the group health policy on which the rebate is based. Word & Brown