Medicare Advantage CMS Marketing Guidelines
Communication and Training Rules
Mandated Recorded Meetings
Sales Process Meetings must be #recorded
Agents and brokers will need to record all sales calls with beneficiaries in their entirety including the enrollment process. The recordings must be retained in a HIPAA compliant manner for 10 years. This will apply to new and existing clients.
- 42 CFR § 422.2274 (g) (2) (ii) Records all calls with beneficiaries in their entirety, including the enrollment process.
- CMS confirmed that the regulations at §§ 422.2274(g)(2)(iii) and 423.2274(g)(2)(iii) are for coverage year 2023 enrollment, beginning Oct. 1, 2022, and require all calls be recorded, including the calls regarding the enrollment process, setting appointments, educational and casual conversations with beneficiaries via personal cell phones. If a prospect does not wish to be recorded, the transaction must end. Broker Bulletin *
- Medicare Advantage Marketing Policies Contract Year 2023 – Frequently Asked Questions
- CMS Monitoring Activities and Best Practices during the Annual Election Period
- Effective October 1, 2023, the only calls required to be recorded are marketing, sales and enrollment calls. General calls, such as setting appointments, are no longer included in the requirement. FAQ CMS.Gov * Blue Shield Agent Bulletin * CMS Definition of Marketing *
- AGA 2024 Summary
What is considered a sales call?
- Anything that falls under the “chain of enrollment’ which is defined as the events from the point when a beneficiary becomes aware of an MA/PDP plan to the end of the enrollment process. This means when you are calling leads, scheduling appointments, collecting drug and provider lists and conducting education meetings and phone enrollments. All of these calls would fall under this guidance.
- Medicare Supplements are not included in the new call recording rules however, if you are selling a Medicare Supplement in tandem with a Prescription Drug Plan, the call would need to be recorded due to the Part D discussion.
- Zoom meetings will also need to be recorded. Only in person, face to face marketing and sales appointments are excluded, however any follow up calls to related to sales and completing the enrollment process would need to be recorded. Sales calls conducted on cell phones also fall under the recording guidelines. Ptt Financial *
Website and Sales Call Disclaimer
We don’t offer every plan Ptt Financial
Bibliography, Resources & Links
- Our Webpages on:
- Federal Register Medicare Program; Contract Year 2023 Policy and Technical Changes to the Medicare Advantage and Medicare Prescription Drug Benefit Programs;
- Regulators Aim to Curb Medicare Plan Lead-Generation Firms Read More>>> Think Advisor.com
- commpartners.com/issues/2022-07-28
- wsj.com/celebrity-medicare-sales-pitches-are-toned-down-after-scrutiny
- Third Party Marketing Organization disclaimer § 422.2267(e)(41)
- 42 CFR § 422.2274 – (same on ECFR.gov) Agent, broker, and other third-party requirements – recording calls
- Broker ONLY Jarvis
What’s on this page?
- Scope of Appointment – Permission to have a meeting
- Illegal to say this is the “Best” plan
- Official brochure on Medicare Advantage Plans with Steve’s Introductory Video
- What are Star Ratings?
- Official Medicare & You with Steve’s Introductory Video
- Mandated Recordings
#Understanding Medicare Advantage Plans (PDF) #12026
- MAPD Plans look like a great deal, as the "premium" is paid by fee from the Federal Government, on average $2k/year.Kff * MAPD Plans must cover all A & B services Medicare.Gov * generally they also cover Part D Rx.
- That's why the premium is very low or ZERO!
- Set a Zoom Meeting
- We can now do SOC Scope of Appointment, before the Meeting via a 3 minute recorded meeting 2 days before. AHIP Training Module 4 Page 14 *
- #Intake Form Berwick Needs Assessment Form - We can better prepare for the meeting
- Medicare Advantage (Medicare Part C): An Overview Hi Cap
- HMO - Narrow Networks?
- HI Cap CA Health Care Advocates Fact Sheet
- Do I just sign up with a Medicare Advantage Company and automatically get * Parts A & B or do I have to get those from Medicare.Gov * VIDEO
- Get Quotes, Full Information and Enroll
- MANDATED wording!: Think Advisor * ‘‘We do not offer every plan available in your area. Any information we provide is limited to those plans we do offer in your area. Please contact Medicare.gov or 1–800–MEDICARE to get information on all of your options.’’
- We disagree with the above wording, as we can use the same tools on Medicare.gov as they do!
- FYI a 4.27.2022 HHS Office of the Inspector General report found that MAPD plans denied 13% of prior authorizations that would have been covered under original Medicare (Conversely, Medi Gap, just follows what Medicare pays.)
- 88% of MAPD enrollees are happy
-
MAPD plans often include Dental & Part D - Rx Prescriptions and often have NO premiums!
-
How is that possible?
-
The Federal Government pays them around $700/month to handle your medical care. You must continue to pay your Medicare Part B premium of about $170/month. It's best to apply when you turn 65 for the supplement plans or advantage plans, as that's the main "Open Enrollment" period, guaranteed issue for any plan.
-
-
-
Medicare Advantage Plans also have an annual open enrollment now known as AEP Annual Election Period October 7 to December 15th.
-
Additional Coverage is important as Medical Bills are increasing Seniors Credit Card Debt or leading to possible bankruptcy?
- If You Have Problems with Your Medicare Advantage Plan
- forbes.com/how-insurers-can-navigate-the-costs-of-medicare-advantage-benefits
- politico.com/medicare-advantage-plans-congress
- Uncle Sam wants you to help stop insurers' bogus Medicare Advantage sales tactics
- ca health advocates/using-ai-to-deny-care
- Dodging the Medicare Enrollment Deadline Can Be Costly
- Medicare Advantage Increasingly Popular With Seniors — But Not Hospitals and Doctors
- Medicare Advantage is bad for patients and bad for investors
- When Medicare Advantage Plans Terminate Coverage
- Medi-Cal D-SNP Feasibility Study
Scope of Appointment
#Scope of Appointment Forms SOC
Permission and agreement to hear a presentation on
Medicare Advantage or Part D Rx
- Blue Cross SOC
- Blue Shield Scope of Appointment SOA 2022 Rev.
- AARP – UHC
- SCAN
- We can now do SOC’s via recorded phone or Zoom meeting! Per AHIP Training Module 4 page 12 www.SteveShorr.com/Meeting
- Needs Assessment Questionnaire – so we can help you better, fit your needs. (Berwick)
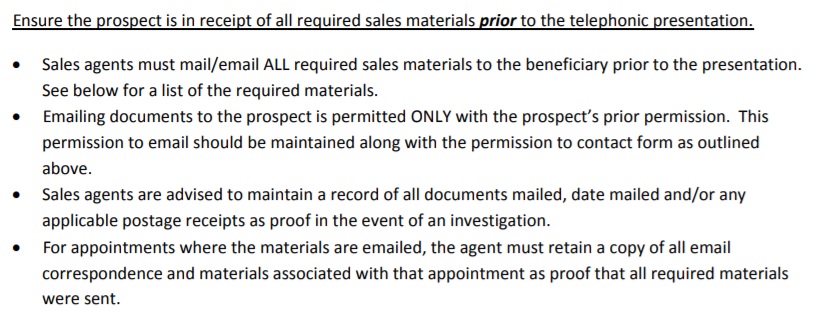
MAPD & Part D Rx Telephone & Face to Face Meetings
require a Scope of Appointment
Before a sales meeting, the agent must obtain a completed and signed Scope of Appointment form from each for example both husband and wife Medicare-eligible consumer – prospect present at a telephonic or in-person one-on-one plan presentation of a Medicare Advantage and/or Prescription Drug Plan product
Agents are required that when conducting marketing activities, in-person or telephonically, that they nor their Plan/Part D Sponsor Insurance Company may not market sell or present any health care related product during a marketing appointment beyond the scope that the beneficiary agreed to before the meeting CMS 2018 Marketing Rules – 70.4.3
The Plan/Part D Sponsor must document the scope of the appointment prior to the appointment
SOA documentation is subject to the following requirements:
The documentation may be in writing, in the form of a signed agreement by the beneficiary, or a recorded oral agreement.
Any technology (e.g., conference calls, fax machines, designated recording line, pre-paid envelopes, and email) can be used to document the scope of appointment.
Marketing Standards (g) Market any health care related product during a marketing appointment beyond the scope agreed upon by the beneficiary, and documented by the plan, prior to the appointment (48 hours in advance, when practicable). and (h), 422.2268(g)
Interpretation?
Humana’s guidance & interpretation 10.2015
Click on image to enlarge
Definition Marketing Activities
20 – Communications and Marketing Definitions 42 CFR §§ 422.2260, 423.2260
Communications means activities and use of materials to provide information to current and prospective enrollees. This means that all activities and materials aimed at prospective and current enrollees, including their caregivers and other decision makers associated with a prospective or current enrollee, are “communications” within the scope of the regulations at 42 C.F.R. Parts 422, 423 and 417.
Marketing is a subset of communications and includes activities and use of materials that are conducted by the Plan/Part D sponsor with the intent to draw a beneficiary’s attention to a MA plan or plans and to influence a beneficiary’s decision-making process when selecting a MA plan for enrollment or deciding to stay enrolled in a plan (that is, retention-based marketing). Additionally, marketing contains information about the plan’s benefit structure, cost sharing, and measuring or ranking standards.
FAQs / Ask Us a Question
Hey fellow agents:
Let’s meet for lunch, video conference and talk about it.
My guess is, only other agents are googling for this page.
How about we meet and exchange ideas?
Email me, [email protected] or set a meeting time.
Well this get’s confusing…
Guidance on Plain Meaning Rule and how to read and interpret law, rules & statutes
Secret Shopper’s Check List 423.2262,
Review and distribution of marketing materials 423.2268 (g) and (h)
Standards for Part D marketing 42 CFR 422.2262, Marketing Materials
2016 Research
70.9.3 Scope of Appointment 2016 – Medicare Marketing Rules
42 CFR 422.2262 Review & Distribution of Marketing Materials
422.2268(g) and (h) can’t market what’s not listed in the scope of appointment
423.2262 Part D Rx Review of marketing materials
423.2268 (g) and (h) Part D can’t market what’s not in scope of appointment
Medicare Training Wikipedia – Meeting
COVID Coverage
Agent ONLY COVID Rules
Scope of Appointment – Telephone & Face to Face Meetings”
FAQ’s
- Hello Steve, thanks for getting into the weeds of this. It can be confusing even after AHIP. My question is: are communications with the prospect still considered ‘marketing’ even after the SOA has been signed? If so, the rules requiring plan benefits information to only be communicated through specific CMS-approved formats would seem to prevent an agent from discussing any plan benefits via email, or even over the phone if not following an official CMS-approved script.
For instance, if a prospect sends me an email requesting that I share information about $0 premium MA plans and I have them fill out an SOA, I might then send an email saying ‘Company X and Y both have zero-premium plans in your area, let’s schedule a call to talk more…’
In effect, by typing out that email I’ve just shared plan benefits information in a non-cms approved format. This interpretation of the rules seems prohibitively burdensome. My upline tells me that marketing rules don’t apply the same way after the SOA, but I’ve never seen that stated as such in any compliance training I’ve taken. What am I missing?
- My biggest grip with AHIP and company training, is that they don’t show the actual law, brochure or Medicare Official Information, but use power point and then forbid agents to show it to anyone. IMHO it’s worthless!!!
Definition Marketing Activities
20 – Communications and Marketing Definitions 42 CFR §§ 422.2260, 423.2260
Communications means activities and use of materials to provide information to current and prospective enrollees. This means that all activities and materials aimed at prospective and current enrollees, including their caregivers and other decision makers associated with a prospective or current enrollee, are “communications” within the scope of the regulations at 42 C.F.R. Parts 422, 423 and 417.Marketing is a subset of communications and includes activities and use of materials that are conducted by the Plan/Part D sponsor with the intent to draw a beneficiary’s attention to a MA plan or plans and to influence a beneficiary’s decision-making process when selecting a MA plan for enrollment or deciding to stay enrolled in a plan (that is, retention-based marketing). Additionally, marketing contains information about the plan’s benefit structure, cost sharing, and measuring or ranking standards.
These rules change… here’s the draft for 2019 See page 6, it looks like the same defintion
- My biggest grip with AHIP and company training, is that they don’t show the actual law, brochure or Medicare Official Information, but use power point and then forbid agents to show it to anyone. IMHO it’s worthless!!!
- do you need a new scope of appointment each time you contact a prospect?
- The link broke… just google it
- This is “crazy!” do we need an SOC to respond to an email?
- Link broke – Google it
- 70.4.3 – Scope of Appointment
- 42 CFR 422.2262, 422.2268(g) and (h), 423.2262, 423.2268 (g) and (h)
- When conducting marketing activities, in-person or telephonically, a Plan/Part D Sponsor may not market any health care related product during a marketing appointment beyond the scope that the beneficiary agreed to before the meeting. The Plan/Part D Sponsor must document the scope of the appointment prior to the appointment. Distinct lines of plan business include MA, PDP and Cost Plan products. If a Plan/Part D Sponsor would like to discuss additional products during the appointment in which the beneficiary indicated interest, but did not agree to discuss in advance, the Plan/Part D Sponsor must document a second scope of appointment (SOA) for the additional product type to continue the appointment.
- SOA documentation is subject to the following requirements:
- The documentation may be in writing, in the form of a signed agreement by the beneficiary, or a recorded oral agreement. Any technology (e.g., conference calls, fax machines, designated recording line, pre-paid envelopes, and email) can be used to document the scope of appointment.
Date of appointment
Beneficiary contact information (e.g., name, address, telephone number)
Written or verbal documentation of beneficiary or appointed/authorized representative agreement
The product type(s) (e.g., MA, PDP, MMP) the beneficiary has agreed to discuss during the scheduled appointment
Agent information (e.g., name and contact information)
A statement clarifying that:
– beneficiaries are not obligated to enroll in a plan
– current or future Medicare enrollment status will not be impacted
– that the beneficiary is not automatically enrolled in the plan(s) discussed
- The documentation may be in writing, in the form of a signed agreement by the beneficiary, or a recorded oral agreement. Any technology (e.g., conference calls, fax machines, designated recording line, pre-paid envelopes, and email) can be used to document the scope of appointment.
- A beneficiary may sign an SOA at a marketing/sales event for a future appointment. Marketing/sales events, as defined in section 70.5, do not require documentation of beneficiary agreement.
- Note: Business reply cards (BRC) separate and independent from a marketing piece, must be submitted in HPMS if benefits and/or costs information is mentioned or the BRC is used as an agreement to be contacted, confirmation of attendance to a sales/marketing event, or request for additional information. Plans/Part D Sponsors should
include a statement on the BRC informing the beneficiary that a sales person may call as a result of their returning a BRC. See section 90.2 for information on the material submission process. - https://www.cms.gov/Medicare/Health-Plans/ManagedCareMarketing/Downloads/CY-2018-Medicare-Marketing-Guidelines_Final072017.pdf#page=45
- I don’t find this in the current version…
- So, it appears that one only needs an SOC for appointments, not answering questions via email.
- I myself love Zoom meetings with screen sharing, as I can show the benefits using the approved summary of benefits for the respective company. That way, I’m not saying anything, the prospect and I are simply reviewing approved material. So, I wouldn’t say Company X & Y have Zero premiums, I’d send the Summary of Benefits and let the client look.
- While not required and I don’t represent Humana… I’ve taken their advise to heart, in all my sales endevors. That way no one can say I said something that wasn’t correct. I insist they go by the law or actual brochure, not what they think I said or may have said in error.
- I don’t see any difference in emailing before or after a SOC
- Is a scope of appointment required if benefits are going to be discussed prior to a beneficiary enrolling on their own via the PURL?
- Personalized URL (PURL): Receive commissions when Medicare beneficiaries use your personalized URL (non-agent-assisted) to enroll online in a WellCare plan.
- I don’t see any way around the mandate to get a scope of appointment. Check with your agency manager.
- https://www.cms.gov/Medicare/Health-Plans/ManagedCareMarketing/Downloads/CY2019-Medicare-Communications-and-Marketing-Guidelines_Updated-090518.pdf
- Scope of Appointment Must be documented for all marketing activities, in-person, telephonically, including walk-ins to Plan/Part D sponsor or agent offices
- The term “marketing” is referenced at Section 1851(h) and 1860 D-4 of the Social Security Act (the Act), as well as in CMS regulations. The scope of the definition of “marketing materials” extends beyond the public’s general concept of advertising materials.
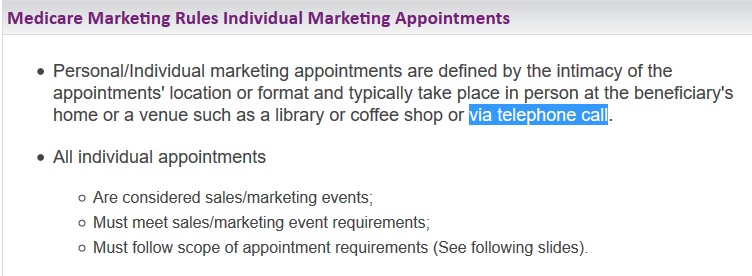
- 70.4.2 – Personal/Individual Marketing Appointments 42 CFR 422.2268(f)-(h), 423.2268(f)-(h)
All Plans/Part D Sponsors conducting one-on-one appointments with beneficiaries, regardless of the venue (e.g., in home, telephonic, or library), must follow the scope of appointment (SOA) guidance (see section 70.5.3). - If a person registers for a marketing seminar for a specific plan/carrier and wants to sign up, is A scope of appointment still required since they obviously registered for the event.
- Yes! One of the things I hate about all these rules, is the AHIP and Company training that we are not allowed to share and is secret.
- Here’s excerpts from something I found it google to answer your question:
- There are two types of sales events, formal and informal. At a marketing/sales event, plan representatives may discuss plan specific information like premium, cost-sharing, and/or benefits, as well as, distribute and/or collect enrollment applications.”
- Formal marketing/sales events are structured events of an audience/presenter style with a sales person providing specific plan information via a specific CMS approved sales presentation.
- Don’ts
- Require or otherwise use personal contact information, collected for purposes of a raffle or other event giveaway, as means of permission for future contact.
- Require the completion of or pressure event attendees to fill out a sign in sheet or business reply card (‘thank you’ card).
- ***Thus, there is NO Registration!
- SCOPE OF APPOINTMENTS (SOA) and Individual Appointments Practices
- Don’t Begin discussing MA or PDP plans prior to the beneficiary signing the SOA Form.
- cms.gov Google new link
- 50.2 – Marketing/Sales Events
42 CFR §§ 422.2268(b)(1-5), 423.2268(b)(1-5)
Marketing/Sales Events are designed to steer or attempt to steer potential enrollees, or the retention of current enrollees, toward a plan or limited set of plans. The following requirements apply to all marketing/sales events:- Plans/Part D sponsors must submit scripts and presentations to CMS prior to use, including those to be used by agents/brokers;
Sign in sheets must clearly be labeled as optional;
Health screenings or other activities that may be perceived as, or used for, “cherry picking” are not permitted;
Plans/Part D sponsors may not require attendees to provide contact information as a prerequisite for attending an event; and
Contact information provided for raffles or drawings may only be used for that purpose.
- Plans/Part D sponsors must submit scripts and presentations to CMS prior to use, including those to be used by agents/brokers;
- Scope of Appointment (Communications)
- Must be documented for all marketing activities, in-person, telephonically, including walk-ins to Plan/Part D sponsor or agent offices
- 50.2 – Marketing/Sales Events
Marketing & Research Tools
Can’t say this is the “#Best Plan.”
Medicare Advantage Plans
- Medicare Advantage Plans 40.4 – Prohibited Terminology/Statements
- You can’t
- Use absolute superlatives (e.g., “the best,” “highest ranked,” “rated number 1”) and/or qualified superlatives (e.g., “one of the best,” “among the highest rank”) unless they are substantiated with supporting data provided to CMS as a part of the marketing review processes or they are used in logos/taglines.
- If the material is submitted via the File & Use program, the supporting data must be included, along with the materials that use an absolute superlative.
- The superlatives used and the data provided must be in context and may not mislead consumers. For example, a Plan/Part D Sponsor that is the only plan in the area that received a 5-star rating in customer service, but received an overall rating of 3 stars, may not promote itself as the highest ranked plan in a service area where other plans have a higher overall rating. CMS.gov 2015 * 42 CFR 422.2262 General Communications , 422.2264 Beneficiary Contact,, 423.2268(e) Standards for Part D Sponsor communications and marketing *
- You can’t
- § 422.2262 General communications materials and activities requirements.
- MA organizations may not mislead, confuse, or provide materially inaccurate information to current or potential enrollees.
- (a) General rules. MA organizations must ensure their statements and the terminology used in communications activities and materials adhere to the following requirements:
- (1) MA organizations may not do any of the following:
- (i) Provide information that is inaccurate or misleading.
- (ii) Make unsubstantiated statements, except when used in logos or taglines.
- (iii) Engage in activities that could mislead or confuse Medicare beneficiaries, or misrepresent the MA organization. 42 CFR § 422.2262
- (1) MA organizations may not do any of the following:
- (a) General rules. MA organizations must ensure their statements and the terminology used in communications activities and materials adhere to the following requirements:
- MA organizations may not mislead, confuse, or provide materially inaccurate information to current or potential enrollees.
30.7 – Prohibited Terminology/Statements
Plans/Sponsors are prohibited from distributing communications that are materially inaccurate, misleading, or otherwise make misrepresentations or could confuse beneficiaries.
Plans/Part D sponsors may not:
Claim that they are recommended or endorsed by CMS, Medicare, or the Department of Health & Human Services (DHHS);
Use unsubstantiated absolute or qualified superlatives or pejoratives;
Note: Unsubstantiated absolute and/or qualified superlatives may be used in
logos/taglines.
Market that they will not disenroll individuals due to failure to pay premiums; or,
Use the term “free” to describe a zero-dollar premium, reduction in premiums (including Part B buy-down), reduction in deductibles or cost sharing, low-income subsidy (LIS), cost sharing for individuals with dual eligibility.
Note: Medical Savings Account (MSA) plans may not imply that the plan operates as a supplement to Medicare. CMS.gov 9.2018 * 42 CFR §§ 422.2264, 423.2264, 422.2268(a)(2), 423.2268(a)(2)
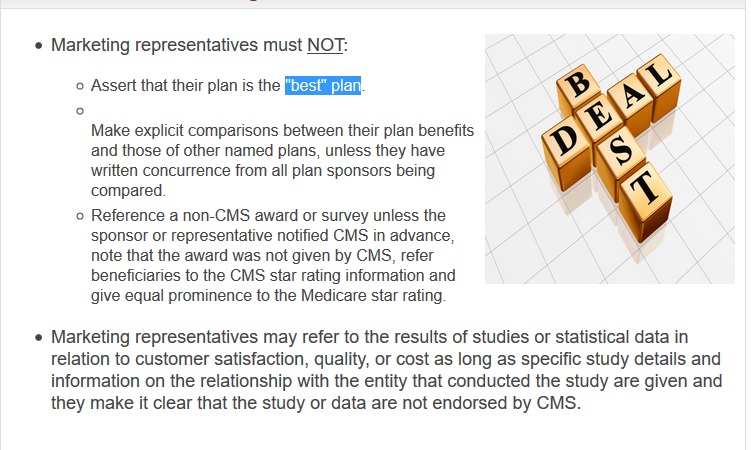
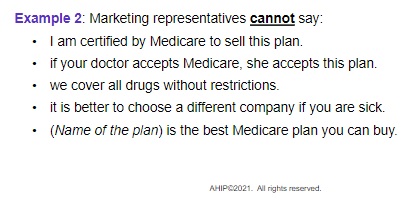
Don’t
- Use qualified or absolute superlatives.
- EXAMPLE: ”One of the best”, “among the highest ranked” or refer to the plan you are marketing/selling as “the best, the highest ranked”, “rated number one”, etc.
- Compare an Anthem Plan (including Amerigroup and Simply Healthcare) to another Plan by name or inference unless you have written concurrence from all plan sponsors being compared, or using CMS Star rating documents. Anthem.com
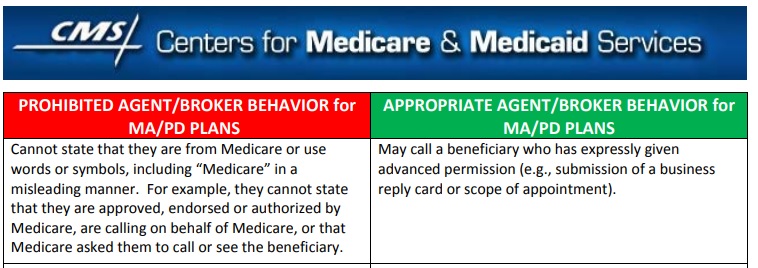
Medicare plans and people who work with Medicare can’t:
- Charge you a fee to process your enrollment into a plan.
- Steer you into a particular plan.
- Communicate incorrect information about their plan type or use inappropriate statements like their plan is “the best” or “highest ranked.” * CA Health Care Advocates * Medicare.Gov
Medicare-Medicaid Plan (MMP) Marketing Information & Resources
This is a technical page, that will cross most anyone’s eyes.
- Marketing rules for health plans
People representing Medicare plans aren’t allowed to: Learn More - Uncle Sam wants you to help stop insurers’ bogus Medicare Advantage sales tactics
- 2025 MA and Part D Final Rule
- outlines new guidelines for compensation to agents, brokers, Third-Party Marketing Organizations (TPMOs) and Field Marketing Organizations (FMOs).
- standardization and eliminating bias in agent plan recommendations to help consumers find the plan that best meets their health care needs.
- outlines new guidelines for compensation to agents, brokers, Third-Party Marketing Organizations (TPMOs) and Field Marketing Organizations (FMOs).
- Medicare Communications 2.9.2022 pdf 53 pages & Marketing Guidelines Webpage:
- PFFS Plans
- Addendum: Model Language for Sales Presentation cms.gov
- Broker ONLY materials – We can summarize for you… If you are a licensed agent or broker, email us with your broker license #.
General Information
Model Material Updates
- Quality Improvement Organization (QIO) Updates (PDF)
- CY 2021 MMP & MSHO Member Material Updates Memo (PDF)
Model Materials
- MMP & MSHO Plan Errata (04/15/2019) (DOCX)
- CY 2020 Explanation of Benefits – Drug-Only (DOCX)
- CY 2020 Explanation of Benefits – Integrated (DOCX)
State-Specific Information
California
- CY 2020 California MMP Model Materials Memo (PDF)
- CY 2020 California MMP Marketing Guidance Memo (PDF)
- CY 2020 California MMP Marketing Guidance (PDF)
- Member ID Card (2020) (ZIP)
- Member Handbook English (2020) (ZIP)
- Member Handbook Spanish (2020) (ZIP)
- Provider & Pharmacy Directory – English & Spanish (2020) (ZIP)
- Summary of Benefits – English & Spanish (2020) (ZIP)
- List of Covered Drugs – English & Spanish (2020) (ZIP)
- Delegated Notices (2020) (ZIP)
- Integrated Denial Notices (2020) (ZIP)
- Annual Notice of Change – English & Spanish (2020) (ZIP)
- CA Insurance Code 787 (i)
- All advertisements used by agents, producers, brokers, solicitors, or other persons for a policy of an insurer shall have written approval of the insurer before they may be used.

Free educational materials for health care professionals on CMS programs, policies, and initiatives. Get quick access to the information you need.
- Publications & Multimedia
-
- Publications
- MLN Matters Articles
- Multimedia
- Events & Training
-
- Calls & Webcasts
- Web-Based Training
- News & Updates
-
- MLN Connects® Newsletter
- Electronic Mailing Lists
- Social Media
- Continuing Education
- Earn continuing education credit
Star Ratings – Legal Codes
Part C—MEDICARE+CHOICE PROGRAM
AKA MAPD Medicare Advantage
Legal Codes
- Plain English on Part C – Medicare Advantage
- Sec. 1851. Eligibility, election, and enrollment
- Sec. 1852. Benefits and beneficiary protections
- Sec. 1853. Payments to Medicare+Choice organizations
- Sec. 1854. Premiums and Premium Amounts
- Sec. 1855. Organizational and financial requirements for Medicare+Choice organizations; provider–sponsored organizations
- Sec. 1856. Establishment of standards
- Sec. 1857. Contracts with Medicare+Choice organizations
- Sec. 1858. Special Rules for MA Regional Plans
- Sec. 1859. Definitions; miscellaneous provisions
42 CFR Part 422 – MEDICARE ADVANTAGE PROGRAM
- SUBPART A — General Provisions (§§ 422.1 – 422.6)
- SUBPART B — Eligibility, Election, and Enrollment (§§ 422.50 – 422.74)
- SUBPART C — Benefits and Beneficiary Protections (§§ 422.100 – 422.133)
- SUBPART D — Quality Improvement (§§ 422.152 – 422.158)
- SUBPART E — Relationships With Providers (§§ 422.200 – 422.220)
- SUBPART F — -Submission of Bids, Premiums, and Related Information and Plan Approval (§§ 422.250 – 422.270)
- SUBPART G — Payments to Medicare Advantage Organizations (§§ 422.300 – 422.324)
- SUBPART H — Provider-Sponsored Organizations (§§ 422.350 – 422.390)
- SUBPART I — Organization Compliance With State Law and Preemption by Federal Law (§§ 422.400 – 422.404)
- SUBPART J — Special Rules for MA Regional Plans (§§ 422.451 – 422.458)
- SUBPART K — –Application Procedures and Contracts for Medicare Advantage Organizations (§§ 422.500 – 422.527)
- SUBPART L — Effect of Change of Ownership or Leasing of Facilities During Term of Contract (§§ 422.550 – 422.553)
- SUBPART M — Grievances, Organization Determinations and Appeals (§§ 422.560 – 422.626)
- SUBPART N — Medicare Contract Determinations and Appeals (§§ 422.641 – 422.696)
- SUBPART O — Intermediate Sanctions (§§ 422.750 – 422.764)
- SUBPART P — S [Reserved]
- SUBPART T — Appeal procedures for Civil Money Penalties (§§ 422.1000 – 422.1094)
- SUBPART V — Medicare Advantage Marketing Requirements (§§ 422.2260 – 422.2276)
- Chapter 1 – General Provisions [PDF, 76KB]
- Chapter 3 – Marketing Guides Instructions [PDF, 47KB]
- Chapter 4 – Benefits and Beneficiary Protections [PDF, 522KB]
- Chapter 5 – Quality Assessment [PDF, 387KB]
- Chapter 6 – Relationships With Providers [PDF, 146KB]
- Chapter 7 – Risk Adjustment [PDF, 1MB]
- Chapter 8 – Payments to Medicare Advantage Organizations [PDF, 194KB]
- Chapter 9 – Employer/Union Sponsored Group Health Plans [PDF, 208KB]
- Chapter 10 – MA Organization Compliance with State Law and Preemption by Federal Law [PDF, 44KB]
- Chapter 11 – Medicare Advantage Application Procedures and Contract Requirements [PDF, 294KB]
- Chapter 12 – Effect of Change of Ownership [PDF, 70KB]
- Chapter 13 – Medicare Managed Care Beneficiary Grievances, Organization Determinations, and Appeals Applicable to Medicare Advantage Plans, Cost Plans, and Health Care Prepayment Plans (HCPPs), (collectively referred to as Medicare Health Plans) [PDF, 426KB]
- Chapter 14 – Contract Determinations and Appeals [PDF, 54KB]
- Chapter 15 – Intermediate Sanctions [PDF, 45KB]
- Chapter 16a – Subchapter A – Private Fee-for-Service (PFFS) Plans [PDF, 198KB]
- Chapter 16b – Subchapter B – Special Needs Plans [PDF, 273KB]
- Chapter 17a – Subchapter A – TEFRA Cost Based Payment Processes and Principles [PDF, 132KB]
- Chapter 17b – Subchapter B – Payment Principles for Cost-Based HMOs and CMPs [PDF, 283KB]
- Chapter 17c – Subchapter C – Cost Apportionment for Cost-Based HMOs and CMPs [PDF, 60KB]
- Chapter 17d – Subchapter D – Medicare Cost Plan Enrollment and Disenrollment Instructions
- Chapter 17f – Subchapter F – Benefits and Beneficiary Protections [PDF, 227KB]
- Chapter 18a – Subchapter A – Cost-Based Payment Process and Principles [PDF, 100KB]
- Chapter 18b – Subchapter B – Payment Principles for Cost-Based HMOs and CMPs [PDF, 168KB]
- Chapter 18c – Subchapter C – Cost Apportionment for Cost-Based HMO/CMPs [PDF, 145KB]
- Chapter 21 – Compliance Program Guidelines and Prescription Drug Benefit Manual Chapter 9 – Compliance Program Guidelines [PDF, 289KB]
- Help with File Formats and Plug-Ins
Related Links
What are Medicare Plan #Star Ratings?
The Overall Star Rating combines scores for the types of services each plan offers: What is being measured? For plans covering health services, the overall score for quality of those services covers many different topics that fall into 5 categories:
- 2025 Star Ratings released Reuters
- cms.gov/2025-medicare-advantage-and-part-d-star-ratings
- KFF News
- CMS ordered to recalculate UnitedHealthcare’s 2025 MA stars
A Texas federal judge has sided with UnitedHealthcare in determining regulators messed up calculating its Medicare Advantage quality scores for next year. Learn More
- Staying healthy: screenings, tests, and vaccines: Includes whether members got various screening tests, vaccines, and other check-ups that help them stay healthy.
- Managing chronic (long-term) conditions: Includes how often members with different conditions got certain tests and treatments that help them manage their condition.
- Member experience with the health plan: Includes ratings of member satisfaction with the plan.
- Member complaints and changes in the health plan’s performance: Includes how often Medicare found problems with the plan and how often members had problems with the plan. Includes how much the plan’s performance has improved (if at all) over time.
- Health plan customer service: Includes how well the plan handles member appeals.
For plans covering drug services, the overall score for quality of those services covers many different topics that fall into 4 categories:
- Drug plan customer service: Includes how well the plan handles member appeals.
- Member complaints and changes in the drug plan’s performance: Includes how often Medicare found problems with the plan and how often members had problems with the plan. Includes how much the plan’s performance has improved (if at all) over time.
- Member experience with plan’s drug services: Includes ratings of member satisfaction with the plan.
- Drug safety and accuracy of drug pricing: Includes how accurate the plan’s pricing information is and how often members with certain medical conditions are prescribed drugs in a way that is safer and clinically recommended for their condition.
For plans covering both health and drug services, the overall score for quality of those services covers all of the topics above.
More links
- Study: 87% of Medicare Advantage plans could lose one or more stars in 2023 ratings
- modern healthcare.com/star-ratings-declines
- Health Affairs.org
- Medicare 2020 Part C & D Star Ratings Technical Notes 184 pages
- q1medicare.com
- Fact Sheet on star ratings
- cms.gov/PerformanceData
- Financial Incentives Tied to Medicare Star Ratings: Impact on Influenza Vaccination Uptake in Medicare Beneficiaries
42 CFR Part 422, Subpart D – Quality Improvement
- § 422.152 — Quality improvement program.
- § 422.153 — Use of quality improvement organization review information.
- § 422.156 — Compliance deemed on the basis of accreditation.
- § 422.157 — Accreditation organizations.
- § 422.158 — Procedures for approval of accreditation as a basis for deeming compliance.
2015 Medicare Advantage Capitation Rates Payment Policies
CMS imposes record number of fines 1st quarter 2015 Modern Health Care
Public Events Secret Shopping Tool CY 2014
Technical & Research Links
Medicare Modernization Act Wikipedia
Guidance for Eligibility, Enrollment and Disenrollment procedures for Medicare Advantage (MA) plans, including MA-PD plans, is provided in Chapter 2 of the Medicare Managed Care Manual.
Congressional Budget Office on how Medicare Advantage Plans Work
Medicare Marketing Website
Medicare Marketing Guidelines
FAQ’s
The Medicare Improvements for Patients and Providers Act (MIPPA)
Summary Public Law No: 110-275 Text – 105 Pages
42 CFR Part 422, Subpart V – Medicare Advantage Marketing Requirements
- § 422.2260 — Definitions concerning marketing materials.
- § 422.2262 — Review and distribution of marketing materials.
- § 422.2264 — Guidelines for CMS review.
- § 422.2266 — Deemed approval.
- § 422.2268 — Standards for MA organization marketing.
- § 422.2272 — Licensing of marketing representatives and confirmation of marketing resources.
- § 422.2274 — Broker and agent requirements.
- § 422.2276 — Employer group retiree marketing.

https://leginfo.legislature.ca.gov/faces/billNavClient.xhtml?bill_id=202320240AB3221
https://www.managedhealthcareexecutive.com/view/improving-your-2026-ma-star-ratings-insights-and-recommendations
https://www.federalregister.gov/documents/2024/04/23/2024-07105/medicare-program-changes-to-the-medicare-advantage-and-the-medicare-prescription-drug-benefit
Medi Medi Rules
https://www.cms.gov/medicare/medicaid-coordination/plans/mmp-marketing-information-resources
https://youtu.be/K8WOkSlqRNI?si=jMSS6iqWoACcfi0C
https://nabip.org/media/9070/nabip-medicare-comment-letter-final.pdf
chrome-extension://efaidnbmnnnibpcajpcglclefindmkaj/https://nabip.org/media/9070/nabip-medicare-comment-letter-final.pdf