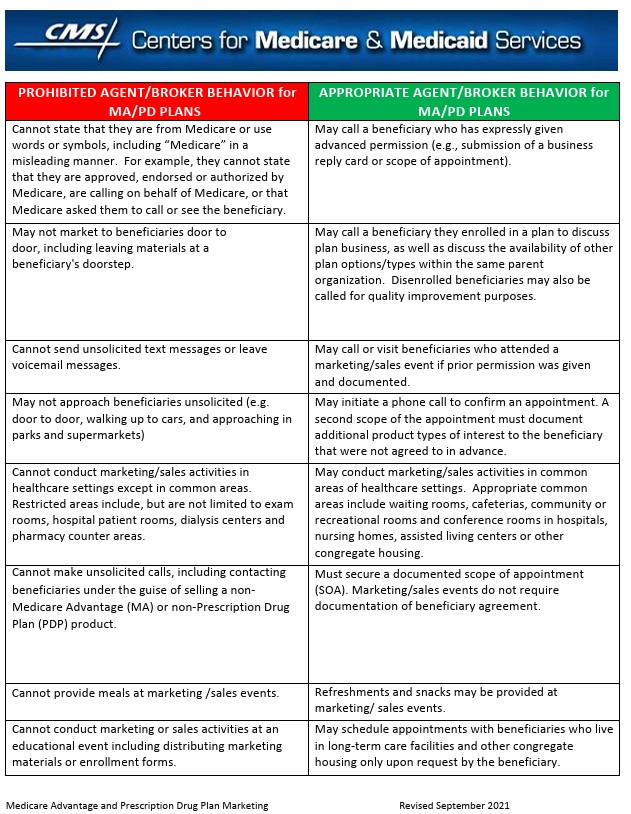
Medicare Advantage CMS Marketing Guidelines
Communication and Training Rules
CMS Simple Prohibitions
one page guide
- medicare.gov/Sales-rules-medicare-plans
- People representing Medicare plans aren’t allowed to:
- Uncle Sam wants you to help stop insurers’ bogus Medicare Advantage sales tactics NPR *
What is Marketing Content?
AI Summary
- Government affiliation disclaimer: Your website must clearly state you are not affiliated with or endorsed by Medicare or any government agency. If your business name includes “Medicare,” a “non-government entity” statement must be placed directly below it.
- TPMO disclaimer: You must include a specific disclaimer (The “We do not offer every plan available…” statement) on your website and in any electronic communications with beneficiaries. The specific wording depends on whether you offer all or only some plans in the area.
- Marketing plan accuracy: You cannot advertise benefits that are not available in the service area where the marketing appears, unless it’s a local/regional media ad where reaching other areas is unavoidable.
- Filing and approval:
- All marketing websites must be filed yearly with CMS.
- You must file the site with the carrier first, which can take time.
- You must obtain prior approval from the insurance company to use specific plan details or logos.
- Misleading content:
- Avoid using superlatives (e.g., “best plan”)
“#Best Plan.”
unless you have supporting data from the current or prior year and cite it.
- Do not use words or symbols that imply endorsement or approval by Medicare or any other government agency. CMS.gov 2015 * 42 CFR 422.2262 General Communications , 422.2264 Beneficiary Contact,, 423.2268(e) Standards for Part D Sponsor communications and marketing CA Health Care Advocates
- Avoid creating a misleading impression that you or your website is part of the government.
- Do not post “confidential and proprietary, agent use only” materials to your website.
- Avoid using superlatives (e.g., “best plan”)
- Targeting rules: You cannot target potential enrollees based on income or health status, unless it’s a special needs plan (SNP).
- Other restrictions:
Medicare Learning Network
- Publications & Multimedia
- News & Updates
- Medicare Advantage Plans hit with Penalties Insure Me Kevin.com 2015 *
- AHIP
- Medicare Managed Care Eligibility and Enrollment
- Managed Care Marketing
- Medicare Marketing Guidelines
- 42 CFR Part 422 – Subpart V – Medicare Advantage Communication Requirements
- Contract Year 2025 Medicare Advantage and Part D Final Rule (CMS-4205-F) CMS.gov *
- Plain Language for agents
- Attorney Summary JDSupra.com
- Hall & Render Marketing Definition
-
Federal regulations define marketing as “communication materials and activities which meet specific intent and content standards.” 42 CFR §§422.2260 and 423.2260.
-
Intent is determined by considering if the material or activity:
-
(a) draws a beneficiary’s attention to a plan or plans;
-
(b) influences a beneficiary’s decision-making process when making a plan selection; or
-
(c) influences a beneficiary’s decision to stay enrolled in a plan (that is, retention-based marketing).
-
-
On the other hand, content is determined by considering if a material or activity mentions:
-
(a) the plan’s benefits, benefits structure, premiums or cost-sharing;
-
(b) measuring or ranking standards (for example, Star Ratings or plan comparisons); or
-
(c) rewards and incentives.
-
-
-
Effective July 10, 2023, any material or activity which mentions any benefit – including
-
vision,
-
dental,
-
hearing or
-
premium reduction –
-
-
will be considered marketing by CMS and, as such, must be submitted via CMS’s HPMS system for review and approval. CMS hopes that this change will help protect beneficiaries from potentially misleading marketing activities.
-
Definition Marketing Activities
20 – Communications and Marketing Definitions 42 CFR §§ 422.2260, 423.2260
- Hall & Render Marketing Definition
-
Review and distribution of marketing materials 423.2268 (g) and (h)
- 42 CFR 422.2262 Review & Distribution of Marketing Materials
- 423.2262 Part D Rx Review of marketing materials
-
Standards for Part D marketing 42 CFR 422.2262, Marketing Materials
- 42 CFR PART 422—MEDICARE ADVANTAGE PROGRAM
- PART 423—VOLUNTARY MEDICARE PRESCRIPTION DRUG BENEFIT Part D Rx
What’s on this page?
- Scope of Appointment – Permission to have a meeting
- Illegal to say this is the “Best” plan
- Official brochure on Medicare Advantage Plans with Steve’s Introductory Video
- What are Star Ratings?
- Official Medicare & You with Steve’s Introductory Video
- Mandated Recordings
More Codes & Info?
- § 422.2274 Agent, broker, and other third-party requirements.
- Contract Year 2026 Policy and Technical Changes to the Medicare Advantage Program, Medicare Prescription Drug Benefit Program, Medicare Cost Plan Program, and Programs of All-Inclusive Care for the Elderly (CMS-4208-F) CMS *
#Understanding Medicare Advantage Plans (PDF) #12026
- Set a Zoom Meeting
- We can now do SOC Scope of Appointment, before the Meeting via a 3 minute recorded meeting 2 days before. AHIP Training Module 4 Page 14 *
- #Intake Form - Please email us [email protected] for the form - That way we can better analyze your situation to give you the answers to your needs and questions.
- Get Quotes, Full Information and Enroll
- MANDATED wording!: Think Advisor * ‘‘We do not offer every plan available in your area. Any information we provide is limited to those plans we do offer in your area. Please contact Medicare.gov or 1–800–MEDICARE to get information on all of your options.’’
- We disagree with the above wording, as we can use the same tools on Medicare.gov as they do!
- Visit our general webpage on Medicare Advantage for much more detail and information.
Marketing & Research Tools