What does “medically necessary”, “medical necessity” & IMR mean?
Medical Necessity
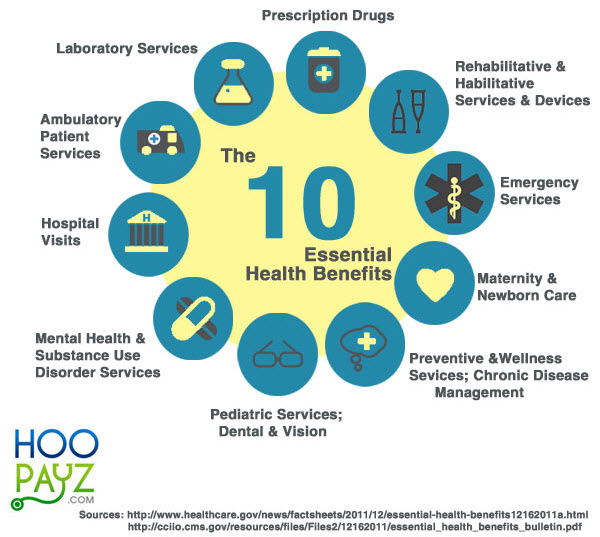
A service is “medically necessary” or a “medical necessity” when it is reasonable and necessary to protect life, to prevent significant illness or significant disability, or to alleviate severe pain. (2014 ACA Sample EOC Page 166) * CIGNA’s Definition * CA WIC §14059.5
Medically Necessary shall mean health care services that a Physician, exercising professional clinical judgment, would provide to a patient for the purpose of preventing, evaluating, diagnosing or treating an illness, injury, disease or its symptoms, and that are:
In accordance with generally accepted standards of medical practice, Illinois Dept of Insurance Definition
The Five Dimensions of the Medical Necessity Definition
- The contractual scope of coverage: whether proposed treatment is explicitly included or excluded in the health plan contract
- Whether the proposed treatment is consistent with professional standards of practice
- Patient safety and setting of the treatment
- Whether the treatment is medical in nature or for the convenience of the health professional or patient and family
- Treatment cost samhsa.gov
most definitions incorporate the principle of providing services which are “reasonable and necessary” or “appropriate” in light of clinical standards of practice
Medicare defines “medical necessity” as services or items reasonable and necessary for the diagnosis or treatment of illness or injury or to improve the functioning of a malformed body member. Glossary Meeicare.Gov
Resources & Links
The Criteria (Clinical UM – Utilization Management)
for establishing the medical necessity of a service:
The service is appropriate for symptoms, diagnosis, and treatment of a condition, illness, or injury; provided for diagnosis, direct care, or treatment; in accordance with the standards of good medical practice; not primarily for the convenience of the member or member’s provider; the most appropriate supply or level of service that can be safely provided to the member. samhsa.gov/
Clinically appropriate, in terms of type, frequency, extent, site and duration, and considered effective for the patient’s illness, injury or disease, and Not primarily for the convenience of the patient, Physician or other health care provider, and not more costly than an alternative service or sequence of services at least as likely to produce equivalent therapeutic or diagnostic results as to the diagnosis or treatment of that patient’s illness, injury or disease.
For these purposes, generally accepted standards of medical practice means standards that are based on credible scientific evidence published in peer-reviewed medical literature generally recognized by the relevant medical community, Physician specialty society recommendations and the views of Physicians practicing in relevant clinical areas and any other relevant factors. Blue Cross ppo_30_eoc Page 108
Visit our HSA page for Federal Definition of Medical Expenses
VIDEO's explaining Medical Necessity

If you know of a better video, please post in comments below or email us the link [email protected]
Excerpt from Insurance Policy – EOC Evidence of Coverage
- The Benefits of this Plan are provided only for Services which are Medically Necessary as defined in this section.
- Services which are Medically Necessary include only those which have been established as safe and effective, are furnished under generally accepted professional standards to treat illness, injury or medical condition, and which are:
- Consistent with the Plan’s medical policy;
- Consistent with the symptoms or diagnosis;
- Not furnished primarily for the convenience of the patient, the attending Physician or other provider; and
- Furnished at the most appropriate level which can be provided safely and effectively to the patient.
- If there are two (2) or more Medically Necessary Services that may be provided for the illness, injury, or medical condition, Blue Shield Life will provide benefits based on the most cost-effective Service.
- Hospital Inpatient Services which are Medically Necessary include only those Services which satisfy the above requirements, require the acute bed-patient (overnight) setting, and which could not have been provided in the Physician’s office, the Outpatient department of a Hospital, or in another lesser facility without adversely affecting the patient’s condition or the quality of medical care rendered. Inpatient services not Medically Necessary include hospitalization:
- For diagnostic studies that could have been provided on an Outpatient basis;
- For medical observation or evaluation;
- For personal comfort;
- In a pain management center to treat or cure chronic pain; and
- For Inpatient Rehabilitation that can be provided on an Outpatient basis. Copied from Blue Shield EOC
All our plans are Guaranteed Issue with No Pre X Clause
Quote & Subsidy #Calculation
There is No charge for our complementary services
Watch our 10 minute VIDEO
that explains everything about getting a quote
- Our Quote Engine Takes all the complexity out of using pencil and paper to figure out the premiums per the Obamacare/ACA rules under CFR §1.36B-3 *
- Get more detail on the Individual & Family Carriers available in CA
Oscar #Clinical Guidelines
Appear to be in Plain English!
- Noninvasive Positive Pressure Ventilation (CG003) English PDF
- Oxygen Therapy (CG005) English PDF
- Hospital Beds and Accessories (CG006) English PDF
- Pressure-Reducing Support Surfaces (CG007) English PDF
- Bariatric Surgery (Adults) (CG008) English PDF
- Bariatric Surgery (Adolescents) (CG009) English PDF
- Medicare.gov on Bariatric Surgery Costs
- Medical Nutrition Therapy (CG010) English PDF
- Oral Liquid Nutritional Supplements (CG011) English PDF
- Non-Covered #Experimental, Investigational, and Unproven Services (CG012) English PDF
- Acupuncture (CG013) English PDF
- Hyperbaric Oxygen Therapy (CG014) English PDF
- Treatment and Removal of Benign Skin Lesions (CG015) English PDF
- Sex Reassignment Surgery (Gender Affirmation Surgery) (CG017) English PDF
- The Longest Mile: Gender Affirming Surgery and Health Insurance Insure Me Kevin.com
- Balloon Ostial Dilation (CG018)
- Wearable Cardioverter-Defibrillator Devices (CG019)
- Home Care – Skilled Nursing Care (RN, LVN/LPN) (CG020) English PDF
- Home Care – Physical Therapy (PT) and Occupational Therapy (OT) (CG021) English PDF
- Home Care – Home Health Aides (HHA) (CG022) English PDF
- Home Care – Speech Language Pathology (SLP) Services (CG023) English PDF
- Colorectal Cancer Screening (CG024) English PDF
- Optical Coherence Tomography (OCT) (CG025) English PDF
- Autonomic Testing (CG026) English PDF
- Breast Imaging (CG027) English PDF
- Diabetes Equipment and Supplies (CG028) English PDF
- Insulin Delivery Systems and Continuous Glucose Monitoring (CG029) English PDF
- Bioengineered Skin and Soft Tissue Substitutes (CG030) English PDF
- BPH Treatment (CG031) English PDF
- Ambulatory Cardiac Event Monitoring (CG032) English PDF
- Botulinum Toxin (CG033) English PDF
- Glaucoma Surgery (CG034) English PDF
- Transcranial Doppler (CG035) English PDF
- Breast Procedures (CG036) English PDF
- Erectile Dysfunction (CG037) English PDF
- Home Births (CG038) English PDF
- Contact Lenses and Eyeglasses (CG039) English PDF
- Potentially Preventable Hospital Readmissions (CG040) English PDF
- Anesthesia and Sedation in Endoscopy (CG041) English PDF
- Skilled Nursing Facility Care (CG042) English PDF
- Prenatal Testing (CG043) English PDF
- Outpatient Physical Therapy & Occupational Therapy (CG044) English PDF
Medical Policies & Clinical UM Guidelines
- Like Lap Band Aetna Bulletin on Obesity Surgery (Gastric Bypass) (Lap Band)
- Cochlear Implants – Hearing
- Clinical Policy Bulletin Index
- Blue Cross Anthem Elevance
- Blue Shield Clinical Policies
How do I find a code.com ICD 9, 10, DRG, CPT, (Current Procedural Terminology) diagnosis code, Medical Billing, coding
- Magellan – Mental Health — Medical Necessity Guidelines for providers
- Care Guidelines Levels of Care – Service Definitions – Term Definitions
- Provider Handbook
- See our webpage on finding a Magellan Therapist – Shrink – Psychiatrist
- See our webpage on Mental Health
Independent Medical #Review (IMR) Program
VIDEO's
DMHC Help Center & Independent Medical Review VIDEO
An Independent Medical Review (IMR) is where expert independent medical professionals review specific medical decisions made by the insurance company. The California Department of Insurance (CDI) administers an Independent Medical Review program that enables you, the insured, to request an impartial appraisal of medical decisions within certain guidelines as specified by the law.
Health insurer delayed her MRI. Meanwhile, the cancer that would kill her was growing.
An IMR can be requested only if the insurance company’s decision involves:
- The medical necessity of a treatment,
- An experimental or investigational therapy for certain medical conditions, or
- A claims denial for emergency or urgent medical services.
It is important to note that the IMR process cannot be used for an insurance company decision that is based on a coverage issue. Only decisions regarding a disputed health care service, as it relates to the practice of medicine, that do not involve a coverage issue are qualified for the IMR program.
You are required to exhaust the internal appeals/grievance process of your particular insurance company before applying for an IMR with the CDI. Click here to read full article on Department of Insurance Website
- IMR on CA Department of Insurance Website
- What Is an Independent Medical Review?
- Who Can Request an Independent Medical Review?
- When Can an Independent Medical Review Be Requested?
- What Issues Are Eligible for an Independent Medical Review?
- What Issues Are Not Eligible for an Independent Medical Review?
- How Does the Independent Medical Review Program Work?
- What Are the Criteria Used in an Independent Medical Review Determination?
- Is There a Way to Process an Independent Medical Review More Quickly in Extraordinary Circumstances?
- Will an Independent Medical Review be Costly?
- Does Independent Medical Review Participation Prevent Future Legal Action?
- Are Medical Records Kept Confidential in the Independent Medical Review Process?
- How Do I Request an Independent Medical Review from the California Department of Insurance?
- Health Insurance Terms and Phrases
- The California Department of Managed Health Care (DMHC) The DMHC regulates HMOs and some PPOs in California – Try using the Insurance Company procedure first
- Complaint Form & IMR
- 1-888-HMO-2219
- [email protected]
- Contact Form
- CA Department of Insurance
- IMR – Independent Medical Review
- ONLINE complaint form insurance.ca.gov/complain
- Magellan Mental Health
- Policy Statement
- Magellan* provides procedures for the expeditious processing of requests for external appeal of adverse determinations through an Independent Review Organization as required by applicable law or customer contract.
- Purpose
- To establish standards to assure independent and timely review of disputed health care services to assure that appropriate, beneficial treatment interventions are made available to members. Magellan Mental Health
- National Health Law Program 12 page pdf on Internal Grievances & External Review in Service Denials in Covered CA Plans
- Milliman Waste Study
- Sections 10169 through 10169.5 of the California Insurance Code (CIC), which became effective January 1, 2001, explain the IMR process in detail. In addition, Section 10145.3 explains the IMR process as it relates to experimental or investigational therapies.
Our Web Pages on
- Medical Necessity – reasonable and necessary Independent Medical Review
- Appeal & Grievances? Medicare – Medi Cal – Covered CA
FAQ’s “Independent Medical Review”
- latimes.com/investigation-delays-los-angeles-hospitals-patients-deaths
- What would be the appropriate venue for a Knox Keene Violation involving a disabled child. We are enrolled in a locally governed managed medical plan & no one seems to understand that it always applies to a disabled child. We passed IMR. They took away my kids best treatment.
- I don’t know that Knox Keene violations is where you want to go…
- What does your Evidence of Coverage say about this issue?
- Try these links:
- dmhc.ca.gov/LawsRegulations knox keene
- dmhc.ca.gov/KKA This link is 1,118 pages of the Knox Keene act. See if you can find the relevant passage and send it to your plan.
- Whole Child Model Grievance Procedure dhcs.ca.gov/CCSGrievancesAFHP
- California Children’s Services Whole Child Model dhcs.ca.gov/CCS Whole Child Model
- What was the treatment? Why do you think it was the best? What’s wrong with the treatment they are offering?
- Pediatric Acute-onset Neuropsychiatric Syndrome (PANS) is a clinical diagnosis given to children who have a dramatic – sometimes overnight – onset of neuropsychiatric symptoms including obsessions/compulsions or food restriction. They are often diagnosed with obsessive-compulsive disorder (OCD) or an eating disorder, but the sudden onset of symptoms separates PANS from these other disorders. In addition, they may have symptoms of depression, irritability, anxiety, and have difficulty with schoolwork. The cause of PANS is unknown in most cases but is thought to be triggered by infections, metabolic disturbances, and other inflammatory reactions. med.stanford.edu/pans
- nimh.nih.gov/information-about-pans-pandas
- panda sppn.org/ppn-pans-diagnostic-guidelines/
- kids health.org/pandas
- wikipedia.org/Pediatric_acute-onset_neuro psychiatric_syndrome
- Treatment Overview liebertpub.com/
- PANDAS Although ASFA (Schwartz, 2016) provides a Category II recommendation grade 1B level of evidence for plasmapheresis or plasma exchange as a treatment for PANDAS and Sydenham’s chorea, there is still conflicting information in the published literature. The AAN guideline on plasmapheresis in neurologic disorders (Cortese, 2011) stated there is “insufficient evidence to support or refute the use of plasmapheresis in the treatment of acute obsessive compulsive disorders (OCD) and tic symptoms in the setting of PANDAS.” Swedo and colleagues (2012) proposed a set of diagnostic criteria for Pediatric Acute-onset Neuropsychiatric Syndrome (PANS) as modified from PANDAS criteria. The authors noted this new set of criteria would need to be validated in large trials. In a retrospective review in a large metropolitan area, Gabbay (2008) reported significant over diagnosis of PANDAS and subsequent therapies that included plasma exchange.
- Experimental Exclusion Experimental or Investigational Services: Services or supplies that are Experimental or Investigational. This exclusion applies to services related to Experimental / Investigational services, whether You get them before, during, or after You get the Experimental / Investigational service or supply.
- The fact that a service or supply is the only available treatment will not make it a Covered Service if it is Experimental / Investigational.
- If the Member has a life-threatening or seriously debilitating condition and the requested treatment is not a Covered Service because it is Experimental or Investigational, the Member may request an Independent Medical Review. eoc.platinum.
- Air Ambulance?
Medical Necessity – Knee &Hip Replacement — #Grievances Medicare”
- Check this instructional bulletin for your doctor

- DOCUMENT MEDICAL NECESSITY TO AVOID DENIAL OF CLAIMS
- CMS recognizes that joint replacement surgery is reserved for patients whose symptoms have not responded to other treatments. To avoid denial of claims for major joint replacement surgery, the medical records should contain enough detailed information to support the determination that major joint replacement surgery was reasonable and necessary for the patient. Progress notes should consist of more than just conclusive statements. Therefore, the medical record of the joint replacement surgical patient must specifically document a complete description of the patient’s historical and clinical findings. Both physicians and hospitals are responsible for ensuring a complete and accurate record.
- Joint Replacement Model extended for 3 years
- Unnecessary health care (overutilization, overuse, or overtreatment) is health care provided with a higher volume or cost than is appropriate.[1] In the United States, where health care costs are the highest as a percentage of GDP, overuse was the predominant factor in its expense, accounting for about a third of its health care spending ($750 billion out of $2.6 trillion) in 2012.[2]
- Factors that drive overuse include paying health professionals more to do more (fee-for-service), defensive medicine to protect against litigiousness, and insulation from price sensitivity in instances where the consumer is not the payer—the patient receives goods and services but insurance pays for them (whether public insurance, private, or both).[3] Such factors leave many actors in the system (doctors, patients, pharmaceutical companies, device manufacturers) with inadequate incentive to restrain health care prices or overuse.[1][4] This drives payers, such as national health insurance systems or the U.S. Centers for Medicare and Medicaid Services, to focus on medical necessity as a condition for payment. However, the threshold between necessity and lack thereof can often be subjective.
- Overtreatment, in the strict sense, may refer to unnecessary medical interventions, including treatment of a self-limited condition (overdiagnosis) or to extensive treatment for a condition that requires only limited treatment.
- It is economically linked with overmedicalization. wikipedia.org/Unnecessary_health_care
- medicare.gov/Surgical-Complications-Hip-Knee
- The most common reason for total knee replacement surgery is arthritis of the knee joint. Types of arthritis include osteoarthritis, rheumatoid arthritis and traumatic arthritis (arthritis which occurs as a result of injury). This arthritis causes a severe limitation in the activities of daily living, including difficulty with walking, squatting, and climbing stairs. Pain is typically most severe with activity and patients often have difficulty getting mobilized when seated for a long time. Other findings include chronic knee inflammation or swelling not relieved by rest, knee stiffness, lack of pain relief after taking non-steroidal anti-inflammatory medications and failure to achieve symptom improvement with other conservative therapies such as steroid injections and physical therapy. Osteonecrosis and malignancy are additional reasons to proceed with total knee replacement surgery. The goal of total knee replacement surgery is to relieve pain and improve or increase patient function.
- Total knee replacement surgery will be considered medically necessary when one or more of the following criteria are met:
- Unsuccessful history of appropriate conservative therapy (non-surgical medical management) that is clearly addressed in the pre procedure medical record. Non surgical medical management is usually implemented for 3 months or more to assess effectiveness. Conservative treatment as clinically appropriate for the patient’s current episode of care typically include one or more of the following:
- anti inflammatory medications,
- analgesics,
- flexibility and muscle strengthening exercises,
- supervised physical therapy [Activities of daily living (ADLs) diminished despite completing a plan of care],
- activity restrictions as is reasonable,
- assistive device use,
- weight reduction as appropriate, therapeutic injections into the knee as appropriate.
- Documentation Requirements
- The medical record must contain documentation that fully supports the medical necessity and justification of the
procedure performed. - cgsmedicare.com/
- The medical record must contain documentation that fully supports the medical necessity and justification of the
- Here are just 5 of MANY recent reports from the medical community showing that Cortisone DOES NOT FIX MY KNEE–it only masks pain and may cause damage!*Harvard Medical School, Cortisone Report, Apr. 1, 2019
- Corticosteroid Shots For Arthritis May Be Making It Worse, Studies Find
- *WebMD, “Disadvantages of Cortisone Injections.”
- *”Cortisone Injection Risks and Side Effects,” Emmanuel Konstantakos, MD Peer Reviewed, 2016, Arthritis Health
- *Dr. McAlindon. “We now know that these injections bring no long-term benefit, and may, in fact, do more harm than good by accelerating damage to the cartilage.”
This study was supported by the NIH’s NIAMS (R01-AR051361) and National Center for Advancing Translational Sciences - *Repeated corticosteroid injections to the joint may speed cartilage degeneration.
Credit Timothy E. McAlindon, M.D., M.P.H., of Tufts Medical Center, Boston. - Since my orthopedic surgeon has indicated that I need Total Knee Replacement, how can I over-ride the Medicare requirement that I have Cortisone Injections before I can have the surgery?
- All my extensive research shows that Cortisone is very damaging to skin, bones and surrounding tissue, just prolongs the damage to my knee, and means that I will be that much older perhaps necessitating a longer recovery.
- I am also an athlete and I am unable to participate in my numerous sports so waiting for Total Knee Replacement means it will be much harder to re-gain my fitness.
- Cortisone Injections are just another cost for Medicare (and me) when TKR will be the end result!
- kantor law.net/health-insurance-claims/
- See our other page on appeals
- I don’t have a grievance yet–so will see how my Appeal for a TKR now goes, since I’ve met the qualifications of “conservative treatments” over the course of the last 2-3 years!!!
- We need to use the exact proper terms.
- Grievance—A complaint about the way your Medicare health plan or Medicare drug plan is giving care. For example, you may file a grievance if you have a problem calling the plan or if you’re unhappy with the way a staff person at the plan has behaved towards you. However, if you have a complaint about a plan’s refusal to cover a service, supply, or prescription, you file an appeal.
- Appeal—An appeal is the action you can take if you disagree with a coverage or payment decision made by Medicare, your Medicare health plan, or your Medicare Prescription Drug Plan. You can appeal if Medicare or your plan denies one of these:
■ Your request for a health care service, supply, item, or prescription drug that you think you should be able to get
■ Your request for payment for a health care service, supply, item, or prescription drug you already got
■ Your request to change the amount you must pay for a health care service, supply, item or prescription drug
You can also appeal if Medicare or your plan stops providing or paying for all or part of a health care service, supply, item, or prescription drug you think you still need. - medicare.gov/Appeals.pdf
- Will see how my Appeal for a TKR now goes, since I’ve met the qualifications of “conservative treatments” over the course of the last 2-3 years!!!
- Please when using technical terms, define them and provide a URL.
/cgsmedicare.com/
- We need to use the exact proper terms.
- CMS recognizes that joint replacement surgery is reserved for patients whose symptoms have not responded to conservative treatments.
- Pre-surgical physical therapy progress notes are important in demonstrating how the patient has progressively worsened over a period of time. Noting that the patient has “failed conservative therapies” in the history and physical is a conclusive statement and should be supported by other specific, objective information in the patient’s medical record. cgsmedicare.com/total_knee_fact_sheet
- One or more of the below conservative treatments have been tried and failed for 3 months or
more except in special circumstances where delay of definitive care is not appropriate:- • Anti-inflammatory medication:
Duration of treatment
• Analgesic
• Home exercise: Duration of treatment
• Physical therapy: Duration of treatment
• Use of cane or walker: Duration of treatment
• Weight loss: Duration of treatment
• Brace: Duration of treatment
• Cortisone shot(s): Duration of treatment
• Visco-supplementation: Duration of treatment
- • Anti-inflammatory medication:
- mass.gov/knee-arthroplasty
A summary of the non-operative, conservative treatment(s) that have been tried and have been unsuccessful in managing the patient’s condition; - *****
- • A listing, description and outcomes of failed non-surgical treatments, such as:
- – Trial of medications (for example, Nonsteroidal anti-inflammatory drugs (NSAIDs)).
– Weight loss.
– Physical therapy.
– Intra-articular injections.
– Braces, orthotics or assistive devices.
– Physical Therapy and/or home exercise plans.
– Assistive devices (for example, cane, walker, braces (specify type of brace), and orthotics) cms.gov/jointreplacement
- – Trial of medications (for example, Nonsteroidal anti-inflammatory drugs (NSAIDs)).
- The average hospital charge for a total knee replacement (TKR) in the United States is $49,500 to $57,000 healthline.com/total-knee-replacement-surgery/costs
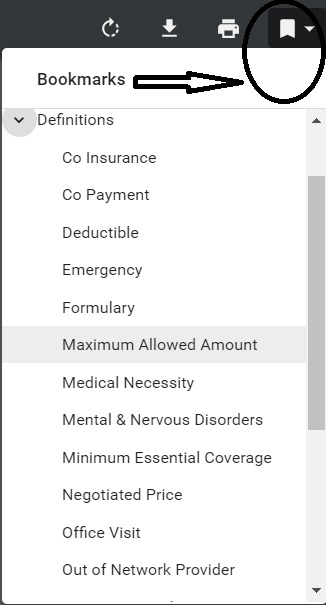
Specimen Individual Policy #EOC with Definitions
Employer Group Sample Policy
It's often so much easier and simpler to just read your Evidence of Coverage EOC-policy, then look all over for the codes, laws, regulations etc! Plus, EOC's are mandated to be written in PLAIN ENGLISH!
- Find your own Individual EOC Evidence of Coverage
- It' important to use YOUR EOC not just stuff in general!
- Obligation to READ your EOC
- Plain Meaning Rule - Plain Writing Act
- Our Webpage on Evidence of Coverage
- OOP Out of Pocket Maximum - Many definitions are explained there.


Does Medicare require prior approval for back surgery?
Currently, Medicare does not pre-authorize coverage of any item or service that will receive payment under Part A or B, except for custom wheelchairs. hhs.gov
The following hospital OPD services will require prior authorization when provided on or after July 1, 2020:
The following hospital OPD services will require prior authorization when provided on or after July 1, 2021:
Download the full list of HCPCS codes requiring prior authorization (PDF)
Provider Education for Required Prior Authorization (PA) Process for the Cervical Fusion with Disc Removal and Implanted Spinal Neurostimulators in the Hospital Outpatient Department (OPD) Setting
Medicare Requires Prior Authorization for Spine Procedures prior authorization for cervical spinal fusion (CPT® codes 22551 and 22552) and implanted spinal neurostimulator procedures (CPT code 63650) when performed in the hospital outpatient department. Visit the website for more details
I have cancer and want to try an experimental drug.
Can I get that in the USA?
Will my Insurance pay for it?
Insurance generally excludes experimental drugs Rx & treatment. See clinical guidelines for experimental above.
President Trump did sign the S 204 Right to Try Act for terminally ill patients.
The new Right to Try act allows patients with life-threatening diseases to bypass the FDA’s application process for “compassionate use” of experimental drugs.
Patients seeking access to “investigational drugs” now need only the approval of their physician and the drug manufacturer.
The new bill protects doctors and companies from the legal risks of allowing unapproved treatments unless they intentionally harm a patient.
The policy that patients must have exhausted all other approved treatments and clinical trial options remains.
Opponents say this won’t help much compared to compassionate use. BBC * Accc-Cancer.org * wikipedia *
Watch out for the rules under hospice where you give up the right to curative treatment.
What about Cosmetic Surgery? Liposuction?
This is something you will have to have your doctors office review with the insurance companies.
Is Liposuction Covered by Health Insurance?
Usually liposuction is not covered by health insurance. Because liposuction is a cosmetic surgical procedure it is not covered by medical insurance unless it has some therapeutic benefit. Female breast reduction surgery is often covered by insurance because surgical breast reduction often relieves chronic pain of the back and shoulders. When female breast reduction is accomplished by tumescent liposuction, insurance may reimburse the patient a portion of the liposuction surgical fees. Similarly, sometimes health insurance will cover liposuction for the treatment of subcutaneous lipomas (small fatty tumors just beneath the skin). Liposuction.com
Liposuction may also be used to treat certain medical conditions, including:
Benign fatty tumors (lipomas).
Abnormal enlargement of the male breasts (gynecomastia or pseudogynecomastia).
Problems with metabolism of fat in the body (lipodystrophy).
Excessive sweating in the armpit area (axillary hyperhidrosis).
Liposuction is not used to treat obesity. It will not get rid of cellulite or stretch marks. A Health Me.com
Here’s clinical bulletins on when these Insurance Companies might consider liposuction, medically necessary:
Oscar – Bariatric Surgery
Aetna – Obesity Surgery
Aetna Cosmetic Surgery
Aetna Abdominoplasty, Suction Lipectomy
More clinical bulletins from Aetna
What do I have to do to get Medicare to approve an MRI?
Sorry, your question is beyond our pay grade. See the CMS link below for complete details only an experienced MD could decipher.
https://www.medicare.gov/coverage/diagnostic-tests
Medicare Part B (Medical Insurance) covers medically necessary clinical diagnostic laboratory tests, when your doctor or practitioner orders them. These tests are done to help your doctor diagnose or rule out a suspected illness or condition. Medicare also covers some preventive services to help prevent, find, or manage a medical problem.
Diagnostic non-laboratory tests
Part B covers diagnostic non-laboratory tests when these apply:
Your doctor or other health care provider orders them.
They’re ordered as part of treating a medical problem.
Examples of diagnostic non-laboratory tests include CT scans, MRIs, EKGs, X-rays, and PET scans. These tests are done to help your doctor diagnose or rule out a suspected illness or condition. Medicare also covers some preventive services to help prevent, find, or manage a medical problem.
Bibliography:
National Coverage Determination (NCD) for Magnetic Resonance Imaging
https://health.costhelper.com/mri.html
A spinal MRI is used to find various spinal problems, including nerve damage or tumors. It typically costs $1,000-$5,000,