MAXIMUM 90 DAYS waiting period for
new employees to get on Group Health Plan
Maximum 90 Day Wait for New Employees
There is MAXIMUM of 90 DAYS waiting period for new employees to be enrolled on Employer Group Health Coverage 8.15.2014 SB 1034 * §2708 * Health & Safety Code 1357.51 (c)
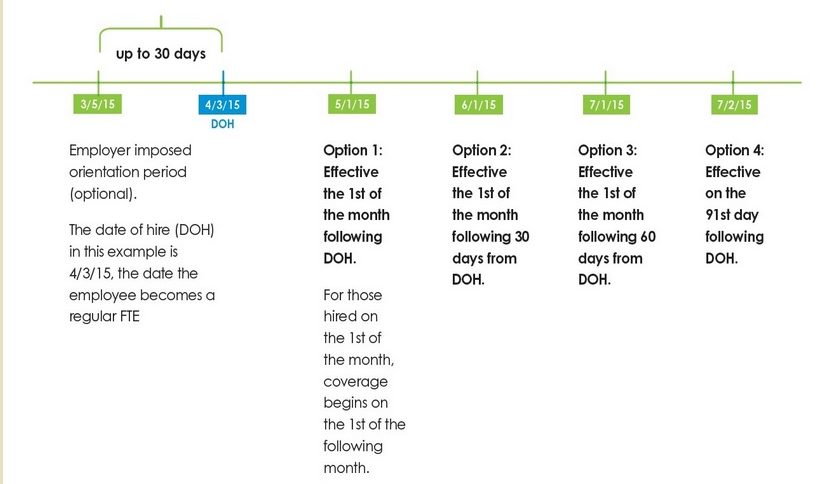
Check to your right or scroll down for a simplified chart of your options that comply with the law. Generally, 1st of the month after date of hire, 1st of month after 30 days, 60 days.
Here’s one companies options.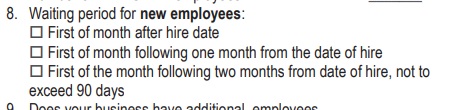
Check the administration page for the company who have – want to check out or check all company Employer Enrollment applications.
The interpretations and implementation can be quite confusing.
There are also Orientation periods Federal Register in addition to waiting periods and probation. All carriers, unless you have the question on the employer app, which Anthem does not will consider the hire date the permanent hire date unless they can prove with an employee manual that they have a 30 days admin period and the person was hired for the 30 days orientation period on 9/12 etc. If employer does not ask about orientation period it is stated that whatever hire date the employer put on the employee app is the permanent hire date.
Most Insurance companies only start coverage on the 1st of the month, thus 90 days probation may not actually work and be in-compliance with the law, thus the waiting period has to be shorter.
Be sure to read the most recent rulings & graphs from YOUR Insurance Company! See Carrier’s below, then go to their administrative page.
Insurance Company Bulletins
Group Health #Carriers
Employer Small Group Health Plans – Introduction
- Carriers – Companies Employer Group no index follow
- Aetna Employer Group Plan Coverage
- Blue Cross – Anthem – Employer Plans
- Blue Shield – Employer Group
- California Choice – Multiple Companies ONE Bill
- Health Net
- Kaiser Permanente – New Enrollment – Administrative
- Oscar – CIGNA + Oscar
- Sharp Health Plan
- SHOP – Covered CA for Small Business
- Sutter Employer Health Plans 2022
- United Health Plan UHC
Background and General Information
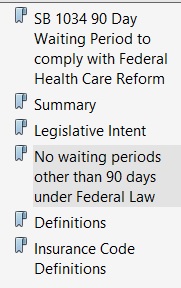
Background… of the maximum 90 rule
- There has been a lot of confusion regarding waiting periods due to the difference between the federal Affordable Care Act (ACA) requirement of 90 days and the California state requirement of 60 days (AB 1083). Recently the Department of Managed Healthcare (DMHC) notified health plans regarding their regulatory position on this issue. The DMHC indicated (their website) AB 1083 addresses the maximum waiting period permitted for California health plans. ACA amended ERISA law so their 90 day maximum applies to employers. Therefore, an employer could select a waiting period of up to 90 days. First of the month following 60 days is not compliant with AB 1083.
- This recent DMHC guidance resulted in changes to the waiting period options offered by some California health plans. With all of the other health reform changes you have to remember we want to provide this quick reference chart.
- Personally, I wish people would stop using the bill # and refer to the actual code.
- So, what is it, under CA Law & Health Care Reform, 60 or 90 day maximum waiting – probationary period for new employees?
- PPACA and CA regulations and law change DAILY!!!
- Waiting periods required by California health plans can be no longer than 60 days. Buck Consultants So, it can’t be 1st of month after 2 month probation period..
Is the Employer liable to pay hospitalization & medical expenses if
he or HR department makes an error and employee doesn’t get enrolled?
There was a court case in 1962 called Gediman v Anheuser Busch, Inc that is said to have prompted the need for employee benefits liability insurance. In this Anheuser Busch was held accountable to the estate of a former employee for providing incorrect information. Employee benefits liability coverage appeared on the market shortly after that case was decided.
Two of the typical exposures that would be considered an object of employee benefits liability coverage, when the employer, HR Department or Benefits Administrator does or doesn’t do:
(1) erroneously calculates the amount of pension program and an employee elects early retirement only to find out that the amount is considerably less; and
(2) forgets to enroll an employee for the company’s hospitalization program and the employee finds out about this omission following a serious illness Rough Notes.com *
With all the rules on Open Enrollment, Late Enrollment, Special Enrollment, Section 125, Insurance Company rules, it’s very difficult to correct a mistake and enroll the employee right away to correct an error. Read this article from ABD Consultion for more detail & explanation.
If an employee doesn’t want coverage – get a signed WAIVER. Here’s the enrollment forms, if there isn’t a separate waiver form, it’s generally included in the enrollment form.
Gediman v Anheuser Busch – Steve’s highlights
The court head that the District Court erred in awarding judgment under the pension plan but that plaintiffs were entitled to recover on the basis that defendant negligently, although in good faith, misinformed Mr. Barsi as to the consequences of the election that he made upon retirement
negligent communication, or failure to communicate with clarity, may give rise to liability;
Communication gaffes: a root cause of malpractice claims
A Failure to Communicate: Clarity v. Offense
to anyone acquainted with pension plan terminology, this does not mean at all what plaintiffs say it meant– namely, that Barsi owned this money just as if it were in a savings account.
the pension consultants did not ‘exercise that care and competence in obtaining and communicating the information which its recipient is justified in expecting.’
Barsi could not have been expected to know this without being told. Neither the Plan nor the employees’ booklet, so beautifully clear to the experienced draftsman, used the kind of language that is fully understandable by even an intelligent layman; perhaps it is just not possible to do so. When the action is on the contract, defendant may properly insist that the boundaries of its obligation are marked out by the technical terms used, whether Barsi understood them or not; but when Barsi sought advice and defendant gave this, it was bound to take account of the frailties of human understanding. By his letter of August 31, 1956, Barsi placed himself in defendant’s hands. Defendant was not required to accept him; it could have suggested he consult his own advisers. Having undertaken to advise, defendant was bound to advise clearly. ‘It is ancient learning that one who assumes to act, even though gratuitously, may thereby become subject to the duty of acting carefully, if he acts at all.’ Barsi had indicated that, acting on his own, he would choose the cash lump sum or the single premium annuity. If he was to be told that the lump sum could not be made available in the single payment that would permit capital gains treatment but that another course, a deferred cash distribution, would give this tax advantage, he should have been plainly warned that the risks incident to death, about which he had earlier been apprised with relation to the period prior to retirement, would continue until whatever date he picked for the distribution. Although we are sure everyone was acting in the best of faith, that needed statement was not forthcoming; instead, the memorandum made one of a dangerously lulling sort.
Enforcement of Maximum 90 waiting period
PENALTY
The penalty for administering a waiting period in excess of the 90-day maximum is the standard penalty for noncompliance with all of the Public Health Services Act health care reform mandates. That penalty is an excise tax of $100 per day with respect to each individual to whom the failure relates. The tax is imposed on the plan sponsor of single employer plans.
If the failure is discovered after the plan receives notice of an audit, the minimum excise tax is $2,500. For a violation that is “more than de minimis,” the minimum penalty increases to $15,000. The maximum penalty for unintentional failures by a single employer plan is the lesser of 10% of the amount paid by the employer during the prior tax year for group health plans or $500,000. Willis.com * graydon.law * Leavitt.com *
Resources & Links
- GUIDANCE ON 90-DAY WAITING PERIOD LIMITATION UNDER PUBLIC HEALTH SERVICE ACT § 2708 NOTICE 2012-59
- Guaranteed availability of coverage 45 CFR § 147.104 –
- Compliance Assistance Guide from DOL.Gov Health Benefits under Federal Law
Insurance Company Requirements to Offer Coverage to ALL employees
Client Links & Resources
- HN Bulletin ♦ HN Sept Bulletin
- Federal Register – Final Rules – Orientation Period – with our annotations and highlights
- 2708 Public Health Service Act – HR 3590 PPACA Page 43
Brother - Sister - Sibling Side Pages Subpages
View our website with your Desktop or Tablet for the most information
Health Coverage #Guide
Art Gallagher
Health Care Reform FAQ's
Understanding Health Reform
***********************************
Compliance #Assistance Guide from DOL.Gov Health Benefits under Federal Law
- Health Care Reform Explained Kaiser Foundation Cartoon VIDEO
- Choosing a Health Plan for Your Small Business VIDEO DOL.gov
- ACA Quick Reference Guide California Small Group Employers Revision 2020 Word & Brown
- kff.org/health-policy-101/
Employee’s guide to #COBRA –
Department of Labor
- EmployER's Guide to COBRA
- DOL on Health & Retirement benefits after job loss
- DOL on COBRA
- Legislation to make COBRA credible coverage
- FAQ CA Department of Insurance
- CA Department of Managed Health Care FAQ's
- Retirement and Health Care Coverage... Questions and Answers for Dislocated Workers
- Federal workers hit by layoffs have their own version of COBRA
Here's what private-sector benefits specialists should know about new hires coming in with "temporary continuation of coverage" benefits. - Navigating COBRA Continuation Coverage: What Employers and Brokers Need to Know
- Your Employer's Bankruptcy – How Will It Affect Your Employee Benefits?
*********
Art Gallagher Employers Guide to COBRA
- Our Webpage on COBRA & Cal COBRA
- Get Individual Guaranteed Issue ACA/Obamacare Quotes -
- Subsidies if you make less than 600% of Federal Poverty Level!
- No Pre X Clause!
- No wait for Open Enrollment as you get Special Enrollment when you lose COBRA or your Employer Group Plan!
Excerpt of Actual Law – HISTORICAL
ARTICLE 3.16. Nongrandfathered Small Employer Plans [1357.500 – 1357.516] Definitions 1357.500
(a) A small employer health care service plan contract shall not impose a preexisting condition provision upon any individual.
(b) A plan contract may apply a waiting period of up to 60 days as a condition of employment if applied equally to all eligible employees and dependents and if consistent with PPACA. A plan contract through a health maintenance organization, as defined in Section 2791 of the federal Public Health Service Act, may impose an affiliation period not to exceed 60 days. A waiting or affiliation period shall not be based on a preexisting condition of an employee or dependent, the health status of an employee or dependent, or any other factor listed in subdivision (h) of Section 1357.503. An affiliation period shall run concurrently with a waiting period. During the waiting or affiliation period, the plan is not required to provide health care services and no premium shall be charged to the subscriber or enrollees.
(c) In determining whether a waiting or affiliation period applies to any person, a plan shall credit the time the person was covered under creditable coverage, provided the person becomes eligible for coverage under the succeeding plan contract within 62 days of termination of prior coverage, exclusive of any waiting or affiliation period, and applies for coverage with the succeeding plan contract within the applicable enrollment period. A plan shall also credit any time an eligible employee must wait before enrolling in the plan, including any affiliation or employer-imposed waiting or affiliation period. However, if a person’s employment has ended, the availability of health coverage offered through employment or sponsored by an employer has terminated, or an employer’s contribution toward health coverage has terminated, a plan shall credit the time the person was covered under creditable coverage if the person becomes eligible for health coverage offered through employment or sponsored by an employer within 180 days, exclusive of any waiting or affiliation period, and applies for coverage under the succeeding plan contract within the applicable enrollment period.
(d) An individual’s period of creditable coverage shall be certified pursuant to subsection (e) of Section 2704 of Title XXVII of the federal Public Health Service Act (42 U.S.C. Sec. 300gg-3(e)).
(Added by Stats. 2012, Ch. 852, Sec. 3. Effective January 1, 2013.) 42 U.S.C. § 300gg-7, Section 10198.7(c) of the California Insurance Code, as amended by Statutes 2013-2014, 1st Ex. Sess., ch. 1, § 7 and Section 13575.1(c) of the California Health and Safety Code, as amended by Statutes 2013-2014, 1st Ex. Sess., ch. 2, § 2, and all of my qualified employees have complied with the waiting period For specifics – Please check the rules for each Insurance Company. Here’s a Summary Chart for all CA Small Employer Insurance Companies ♦ Later Version? ♦
(n) “Affiliation period” means a period that, under the terms of the health care service plan contract, must expire before health care services under the contract become effective
Health Reform §2708 42 US §300gg requires that Employees be eligible within 90 days. DOL Guidance 2012-02 national underwriter.com Health Reform Facts Q & A 249 Final Federal Ruling 2.2014
However, in CA it will be 60 days.


My hire date was July 9th but I didn’t receive benefits until January 1st.
When I looked on my health insurance paperwork it shows my hire date as November 17th.
We also accrued 1 week vacation a year but when I tried to take a vacation day in December I was told i didn’t have any available yet which makes sense since they switched my hire date.
Is it legal to change my hire date like that and delay my benefits?
I can’t legally tell you what is legal.
Sample Blue Cross Employee Application
Section G: Terms, Conditions and Authorizations
Please read this section carefully before signing the application
All statements and answers I have given are true and complete. I understand it is a crime to make or cause to be made a knowingly false or fraudulent material statement or material representation to an insurance company for the purpose of defrauding the company. Penalties may include imprisonment, fines or a denial of insurance benefits. I understand all benefits are subject to conditions stated in the Group Contract and coverage document.
In signing this application I represent that:
I have read or have had read to me the completed application, and I realize any acts of fraud or intentional misrepresentation of material fact in the application may result in loss of coverage within 24 months following the issuance of the coverage.
I understand that coverages will become effective on the date established by the provisions of the group policy, contract and certificates issued thereunder
You might also check with SHRM.org
Does your company have an orientation” period?
Are Cobra benefits are available to employees if they resign before the 90 day probation period is completed?
We will get into COBRA benefits and how long you have to be enrolled in a plan on our COBRA Page.