Can you have Medi-Cal, Medicare, Individual, Employer Group and OHC Other Health Insurance, at the same time?
how much does each one pay?
Which pays first?
Can you still pick which doctor and hospital you go to?
Can you have Private – OHC Other Health Insurance &
Medi Cal at the Same time?
- Yes,
- You can have Medi-Cal even though you have Other Health Coverage (OHC) through individual or group private health (or dental) insurance coverage.
- See the email we rec’d May 17th from Medi Cal to clarify some of these issues.
- Read the rest of the page on which plan pays first, etc. namely, the other plan.
- If you qualify for Medi Cal, you cannot get Covered CA Subsidies.
If you don't #want Medi-Cal
Can you buy private insurance?
- If your income qualifies for Medi-Cal, you can buy Insurance coverage (FREE QUOTES), but there won't be ANY subsidies. You pay the full premium. However, if it's Medi Cal Share of Cost, it's not considered Minimum Essential Coverage, so you could get subsidies.
- Please note that the Private Plan pays first and Medi Cal won't pay if the doctor isn't a Medi Cal provider. Since Medi Cal is virtually HMO that might be difficult to have both plans pay.
- FAQ's
- Which Pays first Medi Cal or other coverage?
- Choose HMO Plan
- FAQ & Clarification of Mandatory HMO Enrollment
- Friendly Agent's Blog on how to have different plans for different members of the family.
Which Insurance Plan pays #first
Medi-Cal or OHC Other Health Coverage?
- Under federal law, your private health insurance must be billed first before billing Medi-Cal. Medi-Cal may be billed for the balance, including your other plans co-payments, co-insurance and deductibles. See below about if you have a Medi Cal HMO. Also, you may have a problem if you went to a provider that isn’t a Medi Cal doctor. You may not quote this page. It’s a summary of what we have footnoted and linked to from official documents & law. Cite only those.
- Denti – Medi Cal and other dental plans See page 19 of Dental Member Handbook
- If you are in a HMO – Managed Care Providers coordination may be difficult and/or you can’t get a Medi Cal HMO, but must have fee for service, see our FAQ’s and response from the Medi Cal Ombudsman for more details.
- See the email we rec’d May 17th from Medi Cal to clarify some of these issues
Jump to section on:
- Introductory Brochure to Medi Cal
- Reference Materials
- Mandate to report other coverage
- Cal Medi Connect – Medi Medi
- Which Pays first Medi Cal or other coverage?
- Can you get Private Coverage?
- Basic Law on Coordination of benefits
- FAQ & Clarification of Mandatory HMO Enrollment
- Choose HMO Plan
- Medicare
Contact Us - Ask Questions - Get More Information
[email protected]
By submitting the information below , you are agreeing to be contacted by Steve Shorr a Licensed Sales Agent by email, texting or Zoom to discuss Medicare or other Insurance Plans as relevant to your inquiry. This is a solicitation for Insurance
Medi-Cal Managed Care HMO – Health Care Options
Here you can review and choose the HMO that you want to deliver your Medi-Cal health Care.
- Get a lot more detail & analysis on Medi Cal HMO providers see our webpage on that
Medi Cal Fee for Service
What is Medi Cal #Fee for Service?
FFS Fee for Service
Under FFS Fee for Service, the California state pays enrolled Medi-Cal providers directly for covered services provided to Medi-Cal enrollees. It is the enrollee’s responsibility to find a physician who accepts Medi-Cal. CHFS.org *
How much does Medi Cal pay?
Medi-Cal Fee for Service will pay the maximum that they are allowed to!
Here’s information what Full Scope Medi Cal * or see what the HMO’s Evidence of Coverage say, and Denti -Cal Cover. Of course Medi Cal will deduct the payment amount, from your other health plan, if any.
Medi-Cal will not pay higher charges of a provider’s bill when the provider has an agreement with the OHC carrier/plan to accept the carrier’s contracted rate as payment in full. See our webpage on negotiated rates. The Medi-Cal provider must submit an Explanation of Benefits or denial letter from the OHC along with the Medi-Cal claim. If Medi-Cal later discovers OHC, Medi-Cal will bill the OHC for the Medi-Cal services.
If you have a Medi-Cal share of cost you must pay it before Medi-Cal will pay for your service.
For Medi Cal HMO’s check out each one’s summary of benefits and EOC’s Explanation of Benefits.
How do I find a provider that accepts Medi Cal?
Sorry there isn’t a Fee For Service provider directory. Try calling Medi Cal @ 1-800-541-5555. You may need to call providers to see if they accept FFS Medi-cal. Email from Ombudsman 1.26.2021 *
See the email we rec’d May 17th from Medi Cal to clarify some of these issues
(HIPP) Health Insurance Premium Payment Program/Cost Avoidance
The Health Insurance Premium Payment (HIPP) program is a voluntary program for qualified beneficiaries with full scope Medi-Cal coverage. HIPP approved Medi-Cal eligible beneficiaries shall receive services that are unavailable from third party coverage and offered by Medi-Cal. Learn More
How to stay in Fee for Service or Apply for Fee for Service considering the mandatory enrollment in HMO Managed Care?
FFS Fee for Service FAQ’s
- Are you prohibited from getting a Medi Cal HMO managed care plan if you have other coverage?
- See the response from the Medi Cal Ombudsman below!
- Contrast that with the more recent reply from Medi Cal here!!!
- Definitions:
- Coordination of Benefits (COB): The process of determining which insurance coverage (Medi-Cal, Medicare, commercial insurance or other) has primary treatment and payment responsibilities for members with more than one type of health insurance coverage
- Fee-For-Service (FFS): This means you are not enrolled in a managed care health plan. Under FFS, your doctor must accept “straight” Medi-Cal and bill Medi-Cal directly for the services you got.
- I don’t see that commercial insurance excludes one from enrolling in the Medi Cal HMO
- Please note, I’m not an authorized Medi Cal representative and nothing I say changes any Medi Cal rules. On my soapbox, I’m upset that Covered CA expects us to facilitate enrollment, without compensation.
- Please keep in mind that only healthcare providers enrolled in Medi-Cal will be reimbursed by Medi-Cal for your care. The best way to ensure that you will not have to pay for your medical care is to ask your provider before your appointment if they accept Medi-Cal. If you already have a provider that you like, be sure to check to see if they are part of the provider network for any plan you select.
- Response from the Ombudsman
- That is correct, having private insurance does block a Medi-Cal beneficiary from being enrolled in a Medi-Cal Managed Care Plan.
- Office of the Ombudsman 358
Managed Care Operations Division
Dept. of Health Care Services
Phone: (888)452-8609
Fax (916) 440-7438
[email protected]
- Office of the Ombudsman 358
- That is correct, having private insurance does block a Medi-Cal beneficiary from being enrolled in a Medi-Cal Managed Care Plan.
#Report changes as they happen - within 30 days! 10 CCR California Code of Regulations § 6496 10 days for Medi Cal 22 CCR § 50185
IRS Form 5152 - Report Changes
- Our Steve's - VIDEO on how to report changes to Covered CA
- Steve's Video on MAGI Income
- Covered CA Video on how to report changes
- Visit our webpage on how to report changes
Do you have to #tell or Report to Medi Cal that you have other coverage?
If you are a Medi-Cal beneficiary and have individual or group private health (or dental) insurance coverage, you are required by federal and state law to report it. You can report it directly to Department of Health Care Services (DHCS) by visiting their webpage on that.
You can also report it to your county eligibility worker, your health care provider, and/or to the Local Child Support Agency (LCSA), when there is an absent parent who may be responsible for your child(ren)’s medical care, or in establishing paternity of a child born out of wedlock. If you fail to report any private health insurance coverage that you have, you are committing a misdemeanor.
The State of California is mandated to find out if you have other health coverage or if it’s available and to collect payment from liable third parties, like a car accident. Thus, you must assign rights to medical support and help locate liable third parties, even going so far as to helping to establish paternity of children born outside of marriage so that the state may seek payment for medical services provided to the child.
- See our webpage on
What do I do if my other health plan sends a check to me?
Send any payment you get directly from an insurance carrier for services paid by Medi-Cal or medical support payment you get from the absent parent to DHCS at:
Department of Health Care Services
Third Party Liability and Recovery Division
Cost Avoidance Section
P.O. Box 997424, MS 4719
Sacramento, CA 95899-7424
If you have other health insurance coverage, the computer system will be coded to show other health insurance. If this information is incorrect you can contact your county eligibility worker to temporarily override this information.
Better yet you can report your other Insurance Information ONLINE!
If you are having a claims payment problem with a provider, you may call the Beneficiary and HIPAA Privacy Help Desk at (916) 636-1980.
If you have both Medicare and Medi-Cal, aka Medi Medi Medicare (not Medi-Cal) will pay for most prescription drugs for Medi-Cal beneficiaries who are eligible for Medicare Part A (hospital) or Part B (outpatient). Here’s our webpage on Medicare Part D (drug coverage) “Medi-Cal What it Means to you” Section 12
#Autism
See our new webpage on Autism
Basic Law on Coordination of Benefits
Basic Law & Rules on #Coordination of Benefits
Benefits When You Have Coverage under More than One Plan
When Coordination of Benefits Applies
This coordination of benefits (COB) provision applies when a person has health care coverage under more than one Plan.
The order of benefit determination rules below govern the order in which each Plan will pay a claim for benefits.
The Plan that pays first is called the Primary Plan. The Primary Plan must pay benefits in accordance with its policy terms without regard to the possibility that another Plan may cover some expenses.
The Plan that pays after the Primary Plan is the Secondary Plan. The Secondary Plan may reduce the benefits it pays so that payments from all Plans do not exceed 100% of the total Allowable Expense. §1300.67.13 * UHC EOC
References & Links
More Explanations of #COB Coordination of Benefits
- Delta Dentals Explanation
- “Working Spouse Rule”
- Health Care Reform Dependent Coverage vs Spousal Coverage
- How about an HSA (Health Savings Account) rather than buying extra policies?
-
Supplemental Plans, like Colonial & AFLAC
- There might be some cases where a COB provision is not allowed – like HIPAA policies for when COBRA ends.
- Individual Plans cannot have this clause per CCR California Code of Regulations 1300.67.13 BUT, they might require that you cancel other coverage. Blue Cross EOC Page 5
- With COBRA protections and HIPAA availability when you lose Group Insurance, it probably is no longer necessary to keep an individual plan, “just in case.” The extra premium, would probably be better spent on Life or Disability Insurance.
- Life Insurance does not have a co-ordination of benefits clause. They will ask on the application though if you have other coverage to prevent over insurance and to make sure there is insurable interest.
- See also Balance Billing
What if your doctor charges more than the negotiated rate? - Employer Dental & Individual Dental?
Technical Resources
- Subrogation if you get in an accident and someone else can be sued
- CA Insurance Code §10270.98 Group Health Insurance Co-Ordination of Benefits
#Dentala Co Ordination of Benefits
-
Coordination of Benefits (COB) Non-Duplication of Benefits Delta Flyer
- Delta Dental – COB Co-Ordination of Benefits only on Group Policies
- Denti Cal Member Handbook
-
- Such clauses means that the secondary plan will not pay any benefits if the primary plan paid the same or more than what the secondary plan allows for that dentist.
- For example, if both the primary and secondary carrier pay for the service at 80 percent level but the primary allows $100 and the secondary carrier normally allows $80 for the same treatment, the secondary carrier would not make any additional payment. However, if the primary carrier only pays 50 percent of the dentist’s allowed fee, then the secondary carrier would reduce its payment by the amount paid by the primary plan and pay the difference. In this case, the secondary carrier would pay $14 ($80 x 80 percent – $50 = $14).
- Dual coverage saves money for you and your group by sharing the total cost of dental benefits between two carriers. Containing costs is an important part of Delta Dental’s plan to keep you smiling.
- understanding non duplication
- Nonduplication COB – In the case of nonduplication COB, if the primary carrier paid the same or more than what the secondary carrier would have paid if it had been primary, then the secondary carrier is not responsible for any payment at all. ADA.org
-
How does dual coverage and COB work?
- With non-duplication of benefits, the primary carrier pays its portion first and the secondary carrier, instead of paying the remainder, calculates what it would have paid if it were the primary carrier and subtracts what the other plan paid.
- For example, if the primary carrier paid 80 percent, and the secondary carrier normally covers 80 percent as well, the secondary carrier would not make any additional payment. However, in the same scenario, if the primary carrier paid 50 percent, the secondary carrier would pay up to 30 percent. Dental Dental
-
-
(a) This section shall only apply to a health care service plan covering dental services or a specialized health care service plan contract covering dental service pursuant to this chapter.
-
(b) For purposes of this section, the following terms have the following meanings:
-
(1) “Coordination of benefits” means the method by which a health care service plan covering dental services or a specialized health care service plan contract, covering dental services, and one or more other health care service plans, specialized health care service plans, or disability insurers, covering dental services, pay their respective reimbursements for dental benefits when an enrollee is covered by multiple health care service plans or specialized health care services plan contracts, or a combination thereof, or a combination of health care service plans or specialized health care service plan contracts and disability insurers.
-
-
Please note, I’m not an attorney nor an authorized claims representative for any Insurance Carrier.
-
-
-
Medicare #DualCoverage
Publication - 02179
-
VIDEO how two plans coordinate and pay your claim.
- Medicare.Gov on how Medicare works with other insurance.
- Employer obligation to report # of employees to Medicare
- Explanation from Cal Broker Magazine Sept 2019
- Sample Small Employer Group Health Plan
- Medicare & Other Insurance CA Health Care Advocates Fact Sheet pdf
#Subrogation
Medicare's Right to collect from other Coverage
- You're Medicare Advantage plan has the right and responsibility to collect - subrogate for covered Medicare services for which Medicare is not the primary payer.
- According to CMS regulations at 42 CFR sections 422.108 and 423.462, Anthem MediBlue Access (PPO), as a Medicare Advantage organization, will exercise the same rights of recovery that the Secretary exercises under CMS regulations in subparts B through D of part 411 of 42 CFR and the rules established in this section supersede any state laws. Anthem MediBlue Access (PPO) Evidence of Coverage
- Medi-Cal (for People with Medicare) – 04-19-23 Hi Cap CA Health Care Advocates
Medicare Secondary Payer Recovery Process
Click to Enlarge
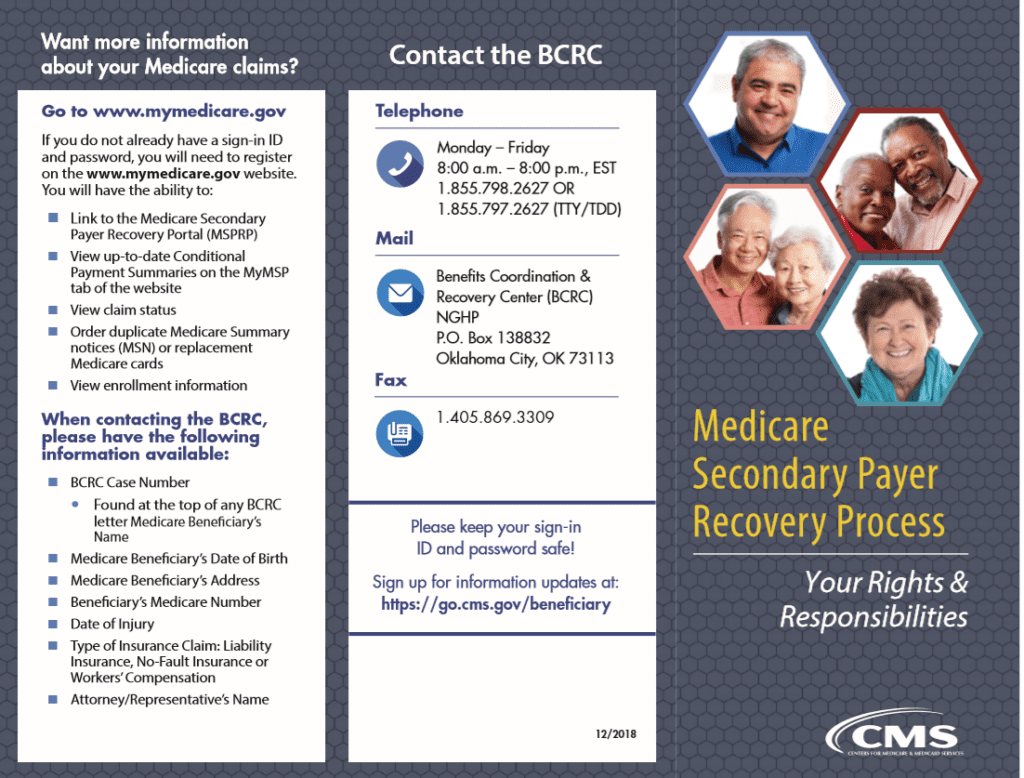
Benefits Coordination & Recovery Center (BCRC)—
The BENEFITS COORDINATION & RECOVERY CENTER (BCRC) acts on behalf of Medicare to collect and manage information on other types of insurance or coverage that a person with Medicare may have, and determine whether the coverage pays before or after Medicare.
BCRC acts on behalf of Medicare to obtain repayment when Medicare makes a conditional payment, and the other payer is determined to be primary – the one that pays 1st.
How are claims paid if you have #Medicare &
Other Insurance?
Dual Coverage?
If you have questions about how Medicare works with other coverage, you’ve come to the right page. Hopefully, we’ve or our links will answer all your questions on dual coverage here. If not, use the FAQs / Ask Us a Question feature below.
We’ve also included the relevant pamphlets from Medicare.
- Medicare Guide to Dual Coverage who pays first publication # 02179
- Medicare website, on dual coverage
- Medicare’s Subrogation Right to collect from other insurance
FAQ’s
I have Medicare and:
- I have Medicaid.
- I’m 65 or older and have group health plan coverage based on my current employment (or the current employment of a spouse of any age), and my employer has 20 or more employees.
- I’m under 65, entitled to Medicare because I have a disability (other than ESRD), I’m covered by a large group health plan because I or a family member is still working.
- I work for a small company that has a group health plan.
- I have a domestic partner with group health insurance coverage.
- I have declined or dropped employer-offered coverage.
- I’m retired, 65 or older and have group health plan coverage from my former employer.
- I’m retired, under 65 and disabled (other than by ESRD), and have group health plan coverage from my former employer.
- I have COBRA continuation coverage.
- I’m in a Health Maintenance Organization (HMO) Plan or an employer Preferred Provider Organization (PPO) Plan that pays first. Who pays first if I go outside the employer plan’s network?
- I get health care services from the Indian Health Service.
- I have more than one other type of insurance or coverage.
- I have TRICARE.
- I have Veterans’ benefits
- I have ESRD and group health plan coverage.
- I have coverage under the Federal Black Lung Program.
- I have a claim for no-fault or liability insurance.
- I filed a workers’ compensation claim.
If you still have questions, email us, * set a meeting, * ask us a question right on this page, you don’t have to even leave your name.
AI Generated
- Transition, Not Termination: The program didn’t disappear; it transitioned into MMPs for better care coordination.
- Integrated Care: MMPs provide all Medicare (Part A, B, D) and Medi-Cal services together, just like Cal MediConnect aimed to.
- Availability: These plans operate in former Cal MediConnect counties (LA, Orange, Riverside, San Bernardino, San Diego, San Mateo, Santa Clara) and are expanding statewide.
- No Coverage Gap: Members were automatically moved, so there was no break in coverage. [1, 2, 4, 5, 6, 7, 8, 9]
#Understanding Medi-Cal Long Term Care
Archive Rev 2001
- CANHR California Advocates for Nursing Home Reform
- Our Webpage on Redetermination Requalification
- Our webpage on how to qualify for Medi Cal Nursing Home Benefits
- When will California's Medi-Cal Will Pay for a Nursing Home, Assisted Living, or Home Care Nolo.com
- Long-Term Services and Supports in Medi-Cal Fact Sheet CHCF.org
- canhr.org/overview-of-medi-cal-for-long-term-care