Dental & Vision Plans Direct & Covered California
individuals & Families
Employer Groups
Introduction To Dental Insurance
- Dental & Vision covers things like Root Canals, crowns, Dentures, Braces, routine cleaning, “deep cleaning” eye exams & glasses.
- Adult Dental & Vision for adults, as opposed to coverage for children is pretty much, but not totally excluded from Health Plans, as it’s not an essential benefit. Specimen Policy Page 118
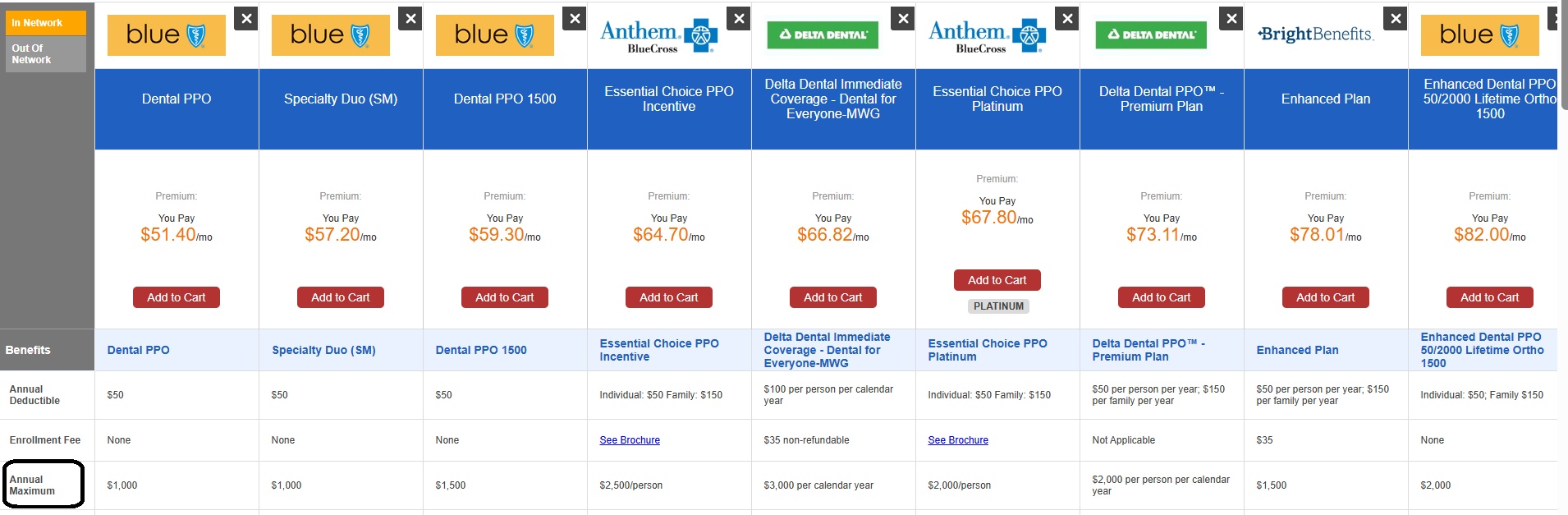
- Please note the maximum payouts/year are generally $1,000 or $1,500 and sometimes 6 months to one year waiting periods to get major services, There are also rules so that insurance companies can stay financially solvent like the 80% Medical Loss Ratio, rule and underwriting to avoid adverse selection so IMHO he more important issue is:
- What plans do you have to take care of your families financial issues and putting food on the table should the breadwinner pass away, not be able to do all the duties that his work requires or fully able to take care of himself?
- Note also that some conditions are covered under the health portion of your medical plan… It’s confusing ask your doctor, ask us [email protected] or your insurance companies member services or claims department.
- Here’s a problem someone had when going to their optometrist, but it was a medical issue Kff.org
- Explanation of Vision vs Medical by Associates in Eye Care
Get Quotes & Enroll
- Quotit – Online Quotes & Enrollment
- Delta Dental and Dental for Everyone
- Covered CA – Ask us [email protected] or log into your account and click on Select Dental Plan in right hand side under Actions
Try turning your phone sideways to see the graphs & pdf's?
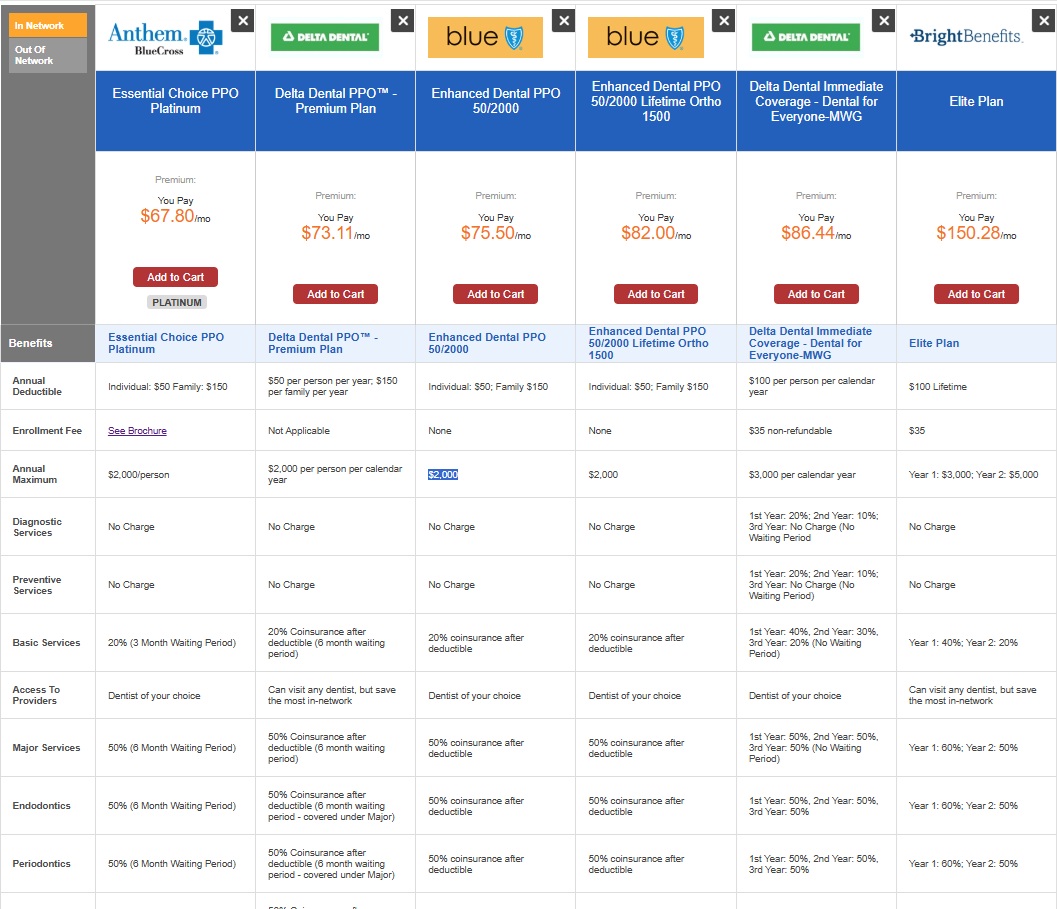
- In this video,
- I address a question about dental plans that may not meet expectations and how to effectively shop for better options.
- I explain the concept of medical loss ratio and emphasize the value of employer-sponsored dental plans.
- I guide you on how to access quotes through our dental page, where you can compare reputable plans side by side.
- Additionally, I highlight some specific plans, including their coverage details and waiting periods.
- If you have any questions or need assistance, feel free to reach out via email or schedule a Zoom meeting with me.
#Covered California Dental Insurance Plans
- Go into your Covered CA account or use our Instant No Obligation Quote Engine
- Dental Options – Add the plan you want to your cart
- Click on Shop for Dental
- One can only apply for Dental with Covered CA at Open or Special Enrollment email dated 6.12.2019 2:47 PM *
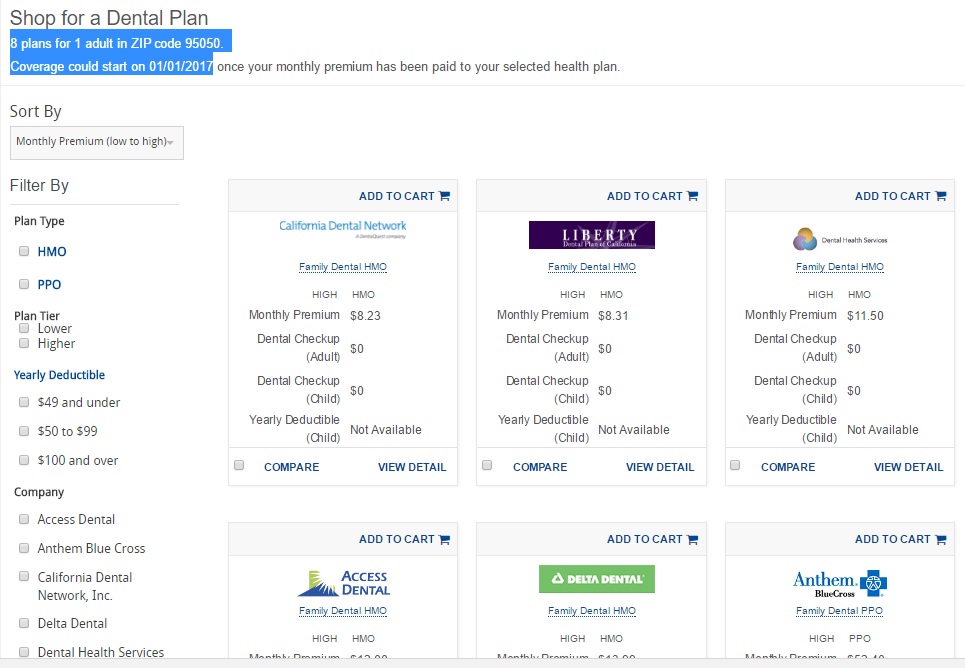
- Plans outside of Covered CA – Quotit Dental for Everyone
- Delta Dental Individual & Family™ Delta Dental PPO™ Family Dental Plan
- Delta Dental Individual & Family™ DeltaCare® USA Family Dental HMO
- If you have trouble locating the brochures, email us [email protected]
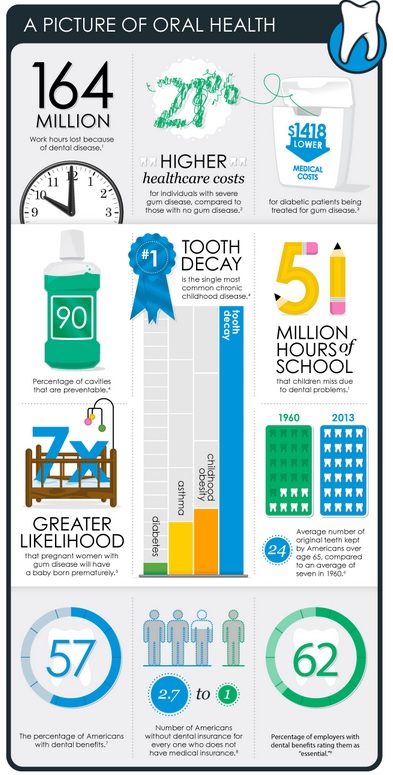
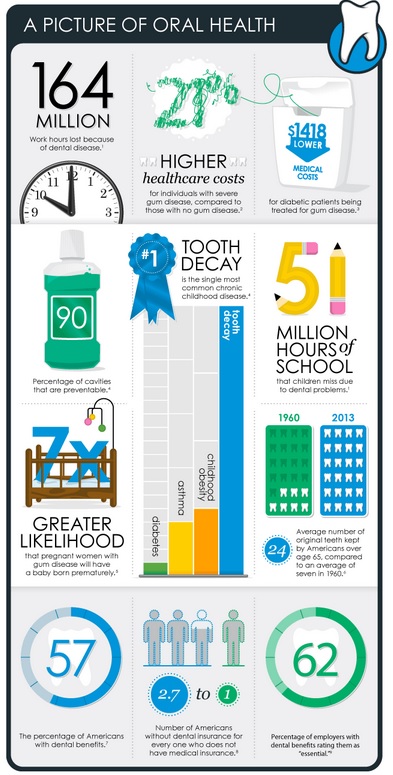
#Importance of Dental Coverage
Picture of Oral Health cdc.gov
- Dental For #Everyone, Instant Quotes - Online Enrollment
-

Delta Dental - Get Quotes & Enroll
- Quotit Quotes for Dental
All our Health plans are Guaranteed Issue with No Pre X Clause
Instant Quote & Subsidy #Calculation
There is No charge for our complementary services, we are paid by the Insurance Company.
- Our Quote Engine Takes all the complexity out of using pencil and paper to figure out the premiums per the Obamacare/ACA rules under CFR §1.36B-3 *
- We are authorized Brokers for Dental, Vision & Covered CA get instant quotes direct and in Covered CA with subsidy calculation for:
- Watch our 10 minute VIDEO that explains everything about getting a quote
#Delta Dental Direct

Delta Dental - Get Quotes & Enroll Affiliate Link
Be sure to put in our AGENT # 2094784
Delta Dental – Covered CA Plans
-
-
- Much more detail on Delta Dental our webpage
-
Dental For #Everyone,
has an excellent website with full brochures, Instant online quoting and enrollment
- Dental for Everyone includes quotes from
- Careington Discount Plan
- Bright Benefits
- Renaissance Dental
- Delta Dental
- AmFirst
- One of our colleagues on how Dental for Everyone Works.
- Some of our webpages on dental
- VSP Vision
Contact Us - Ask Questions - Get More Information - Schedule a Zoom Meeting
[email protected]
By submitting the information below , you are agreeing to be contacted by Steve Shorr a Licensed Sales Agent by email, texting or Zoom to discuss Medicare or other Insurance Plans as relevant to your inquiry. This is a solicitation for Insurance
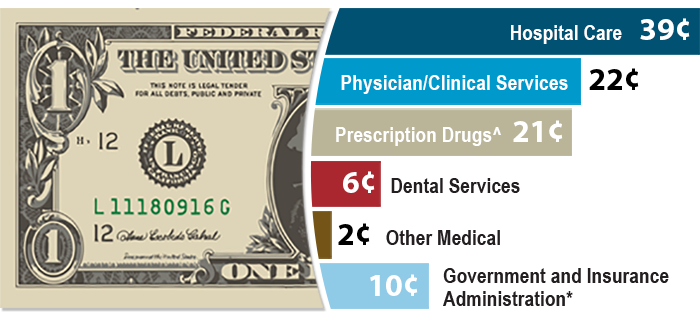
#Invisalign & Orthodonture
AI Overview of Invisalign
-
- How it Works: Patients wear a series of custom aligners for about 1-2 weeks each, gradually moving teeth into place.
- Treatment Time & Cost: Treatment can take as little as six months, though it varies by complexity
. Costs generally range from
-
$1,200 to over $10,000 with average cases often falling between $3,000 and $6,500.
- Key Benefits: Removable for eating, drinking, and brushing; no food restrictions; reduced discomfort compared to wires; improved oral hygiene.
- Process: An initial 3D digital scan (iTero) creates a precise treatment plan. Regular check-ups with a doctor are required.
- Suitability: Effective for adults, teens, and children, often addressing issues like crowding, gaps, and malocclusion.
- Invisilign.com on what dental plans cover orthodonture and Invisalign.
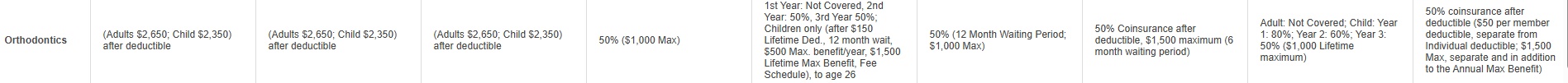
Medical Loss Ratio 80% Claims - 20% Operating Costs & Profit
So, why trade $$$ back and forth if you can afford not to?
Image from BCBS.com
Steve's Explanation of MLR Medical Loss Ratio
More Video's
- Kaiser Health News - Medical Loss Ratio video
- White House – YouTube Channel on Health Care Reform
- Tom Petersen Insurance 101 History of Lloyds to present EXCELLENT!!!
- Our Webpage on MLR & Actuarial Value
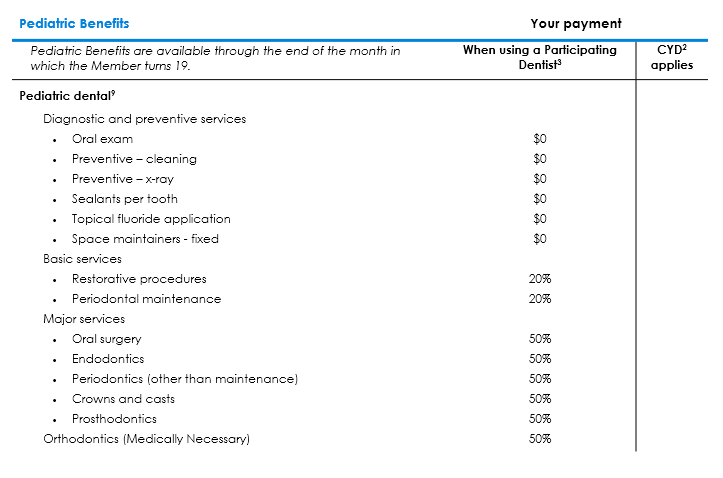
Pediatric – Children’s Dental
#Pediatric Dental and Vision
Pediatric Dental and Vision are Mandatory essential benefits under Section “J” 42 USC 18022 SB 951, even if there are no children on the policy. If there are no children, you are not getting charged see FAQ below for more detail.
- Resources & Links
- Blue Shield Trio HMO EOC Evidence of Coverage 2019 Page 50 for Dental & 112 for Vision
- Blue Shield Graphic on Pediatric Dental & Vision
- Covered CA – Ask us [email protected] or log into your account and click on Select Dental Plan in right hand side under Actions
- Delta Dental VIDEO Changes with Health Care Reform Pediatric Dental
- Children’s Vision Problems Often Go Undetected, Despite Calls for Regular Screening
- Insure Me Kevin.com explanation of Children’s Dental & Vision
Pediatric Dental from Summary of Benefits
Seniors
Also see our pages on:
Oral Health for #Seniors
Justice in Aging - Advocates Guide Updated 2025
- Denti-Cal under Medi Cal
- National Institute for Dental Research - Caregiver information
- Health.Gov tips for older adults
- nia.nih.gov/taking-care-your-teeth-and-mouth
- Dental Care - Medicare
Dental - Glossary – #Dictionary
- Sealants Fact Sheet
- Dental Site – Dr. Dorfman DDS Excellent Site for Dental Information
- Deep Cleaning explanation & coverage
- Dental Implants
- Sacramento Truck driver sudden dealth from tooth infection Sacramento Bee 1.31.2017
More Information
California
- 2025 plan brochures Brokers ONLYEnglish
- Direct – Not Covered CA
- Delta Dental Individual & Family™ Delta Dental PPO™ Family Dental PPO 1690 KB
- Delta Dental PPO™ Children’s Dental PPO for Small Businesses 1688 KB
Delta Dental PPO™ Family Dental PPO for Small Businesses 1690 KB
Delta Dental PPO™ Family Dental PPO for Small Businesses 949 KB
Delta Dental Individual & Family™ DeltaCare® USA Family Dental HMO 945 KB
DeltaCare® USA Children’s Dental HMO for Small Businesses 948 KB - California Brochures
- Delta Dental PPO Premium Plan covers implants at 50%, after a 12-month waiting period.
- Delta Dental Individual & FamilyTM Delta Dental PPOTM Family Dental Plan 669 KB
- Delta Dental PPOTM Children’s Dental PPO for Small Businesses 790 KB
- Delta Dental PPOTM Family Dental PPO for Small Businesses 794 KB
- Delta Dental Individual & FamilyTM DeltaCare® USA Family Dental HMO 872 KB
- DeltaCare® USA Children’s Dental HMO for Small Businesses 837 KB
- Members Resource WebPage
- Find a Dentist
- FAQ’s
- What do we need to give to Delta Dental to have the 6 month waiting period waived?
- Let’s check the EOC Evidence of Coverage and Summary of Benefits
- Attachment A Footnote 3 just says acceptable documentation. I suggest that your ID card and proof of payment for 6 months will suffice.
- Let’s check the EOC Evidence of Coverage and Summary of Benefits
- What do we need to give to Delta Dental to have the 6 month waiting period waived?
- Broker ONLY
More on dental
- Dental care reduces likelihood of hospitalization for people with diabetes or coronary artery disease Medical Press 5.6.2022
- The 2022 State of America’s Oral Health and Wellness Report Commissioned by Delta Dental Plans Association
- What drives buyers of individual Delta Dental plans?
- 77 Million Adults Do Not Have Dental Insurance
- CDA-sponsored bills seek more protections, increased oversight of dental insurance Bills would prohibit plans from imposing arbitrary waiting periods, denying coverage for preexisting conditions; require rate review and ERISA notice Learn More >> CDA * CA Legislature * California Benefits Review Program *
-
Steve on buying, shopping and best use of premium dollars
Dental Insurance VIDEOMORE VIDEOS
- What dental Insurance… should I buy???
- VIDEO the dentist attempts to give you some guidance about things to consider before buying a dental insurance plan, finance plans available, negotiating with your dentist
- Sacramento Truck driver sudden dealth from tooth infection Sacramento Bee 1.31.2017
- Health Savings Accounts?
- Video – how bad sugary drinks are for you
- What dental Insurance… should I buy???
Deep dental cleaning is also called periodontal scaling and
root planning, or SRP.
- Deep dental cleaning is also called periodontal scaling and root planning, or SRP. It’s similar to how a hygienist typically cleans your teeth but focuses on the outer surface of the roots and below your gum line. This special cleaning is needed when tartar buildup has caused infection of the gums. Pockets form, a widening of the gumline that has pulled away from the tooth. Loss of this connective tissue can lead to bone loss and, eventually, tooth loss. Learn More
- The Difference: Deep Dental Cleaning vs Regular Cleaning

- Image from Mouth Healthy.org
- You Tube VIDEO on deep cleaning
- If you’re a dentist check out Spear Education.com
- If you have recently sat in your dentist’s chair for a routine exam, or you plan to in the near future, you are already ahead of the 34% of Americans who skip their checkup.
- Let’s set the record straight: if your dentist has suggested a deep cleaning, it is important that you get one scheduled right away. my ideal dental.com
- Here’s how to avoid the need for a deep dental cleaning
- You can prevent gingivitis and periodontal disease and avoid the need for a deep dental cleaning. “Probably 95 to 98% of dental disease, and periodontal disease in particular, is preventable,” Dr. Crum says.
- Key to prevention is better home care. You’ve had the recommendations drilled into your head since you were a kid—brush twice a day and floss once a day. If traditional brushing and flossing aren’t cutting it for you, there are different home care tools you can try.
- People with manual dexterity issues or arthritis might do better with an electric toothbrush.People who don’t like wrapping floss around their fingers can use floss picks or power cleaners like Waterpiks.People who have larger spaces between their teeth can try small brushes for cleaning that area.
Visiting your dentist periodically is also key. Regular cleanings can catch gum disease early and keep the plaque and tartar from spreading below the gumline. considerable.com
Technical & Research Resources
- webb dental.com/
- tmj.org/
- Basic and general rules on Coordination of Benefits
- Appeals & Grievances our webpage
- Dental is an essential benefit under ACA/Obamacare CHCF.org
- Read the actual policy EOC for full details of the benefits our webpage
Our other pages on
Dental Coverage
We don't put a lot of effort into selling dental coverage. Generally it's a wash on paying premiums vs getting back claims payments. Unless it's employer group. Then the premiums are tax deductible under IRS Section 106.
Here's more information on how we feel about dental. Here's our page on implants, where we get lots of inquires, but few sales. Most people only seem to want dental coverage, after they've been told they need a lot of dental work. Not profitable for Insurance Companies. See our other pages for details & explanations. See our page on Medical Loss Ratio. Insurance Companies need to take in $1 to pay 80c in claims.
Medicare Plans
- Anthem Blue Cross
- Blue Shield – Medi-Gap – Any Medicare Provider
- Health Net Medi Gap
- UnitedHealthcare Medi Gap
- Scan
Individual & Family Plans
Dental For Everyone,
has an excellent website with full brochures, Instant online quoting and enrollment
One of our colleagues on how Dental for Everyone Works..
Employer Group Plans
- Medi-Cal