Dental & Vision Plans Covered California
individuals & Families
Employer Groups
Introduction To Dental Insurance
Dental & Vision covers things like Root Canals, crowns, Dentures, Braces, routine cleaning, “deep cleaning” eye exams & glasses.
Adult Dental & Vision for adults, as opposed to coverage for children is pretty much, but not totally excluded from Health Plans, as it’s not an essential benefit. Specimen Policy Page 118
Please note the maximum payouts/year are generally $1,000 or $1,500 and sometimes 6 months to one year waiting periods to get major services, There are also rules so that insurance companies can stay financially solvent like the 80% Medical Loss Ratio, rule and underwriting to avoid adverse selection so IMHO he more important issue is:
- What plans do you have to take care of your families financial issues and putting food on the table should the breadwinner pass away, not be able to do all the duties that his work requires or fully able to take care of himself?
Get Quotes & Enroll
- Quotit – Online Quotes & Enrollment
- Delta Dental and Dental for Everyone
- Covered CA – Ask us [email protected] or log into your account and click on Select Dental Plan in right hand side under Actions
- Dental Dictionaries
- Op Ed Glasses are still too damn expensive LA Times 1.11.2022
Try turning your phone sideways to see the graphs & pdf's?
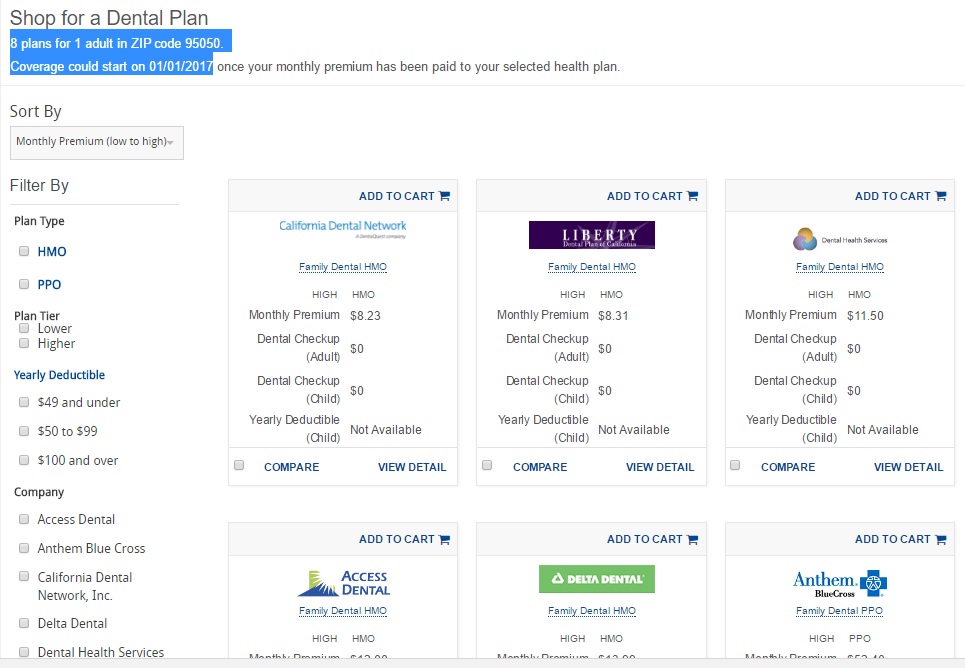
#Covered California Dental Insurance Plans
- Covered California Announces Premium Change for 2025 Dental Plans and Increased Choices for Consumers Throughout the State
- Go into your Covered CA account or use our Instant No Obligation Quote Engine
- Dental Options – Add the plan you want to your cart
- Click on Shop for Dental
- One can only apply for Dental with Covered CA at Open or Special Enrollment email dated 6.12.2019 2:47 PM *
- Plans outside of Covered CA – Dental for Everyone
Click to enlarge
- Delta Dental Individual & Family™ Delta Dental PPO™ Family Dental Plan
- Delta Dental Individual & Family™ DeltaCare® USA Family Dental HMO
- If you have trouble locating the brochures, email us [email protected]
#Covered CA Certified Agent
No extra charge for complementary assistance
- Get Instant Health Quotes, Subsidy Calculation & Enroll
- Appoint us as your broker
- Get Instant Health Quotes, Subsidy Calculation & Enroll
- Videos on how great agents are
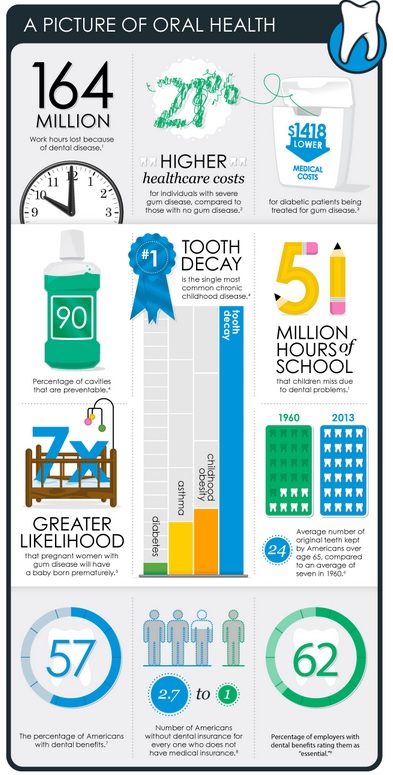
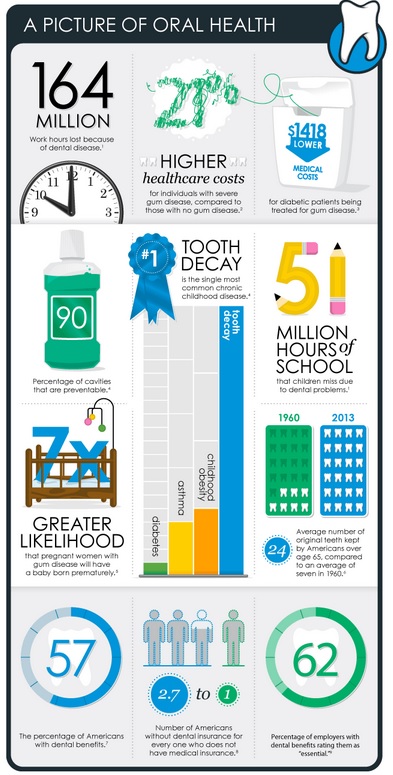
#Importance of Dental Coverage
Dental & General Health
Insurance 101?
We suggest that you check out Life Insurance, Disability, Long Term Care and Retirement as these risks may cause much more financial devastating to your budget than dental bills.
Picture of Oral Health
- Dental For #Everyone, Instant Quotes - Online Enrollment
-

Delta Dental - Get Quotes & Enroll
- Dental care reduces likelihood of hospitalization for people with diabetes or coronary artery disease Medical Press 5.6.2022
- The 2022 State of America’s Oral Health and Wellness Report Commissioned by Delta Dental Plans Association
- What drives buyers of individual Delta Dental plans?
- 77 Million Adults Do Not Have Dental Insurance
- CDA-sponsored bills seek more protections, increased oversight of dental insurance Bills would prohibit plans from imposing arbitrary waiting periods, denying coverage for preexisting conditions; require rate review and ERISA notice Learn More >> CDA * CA Legislature * California Benefits Review Program *
Steve on buying, shopping and best use of premium dollars
Dental Insurance VIDEO
MORE VIDEOS
- What dental Insurance... should I buy???
- VIDEO the dentist attempts to give you some guidance about things to consider before buying a dental insurance plan, finance plans available, negotiating with your dentist
- Sacramento Truck driver sudden dealth from tooth infection Sacramento Bee 1.31.2017
- Health Savings Accounts?
- Video - how bad sugary drinks are for you
#Delta Dental Direct

Delta Dental - Get Quotes & Enroll Affiliate Link
Be sure to put in our AGENT # 2094784
Delta Dental – Covered CA Plans
California
- 2025 plan brochures Brokers ONLY
English
- Direct - Not Covered CA
- Delta Dental Individual & Family™ Delta Dental PPO™ Family Dental PPO 1690 KB
-
Delta Dental PPO™ Children's Dental PPO for Small Businesses 1688 KB
Delta Dental PPO™ Family Dental PPO for Small Businesses 1690 KB
Delta Dental PPO™ Family Dental PPO for Small Businesses 949 KB
Delta Dental Individual & Family™ DeltaCare® USA Family Dental HMO 945 KB
DeltaCare® USA Children's Dental HMO for Small Businesses 948 KB - 2024 Brochures
- All about dental implants How these artificial teeth can help your smile
- Delta Dental Individual & Family™ Delta Dental PPO™ Family Dental PPO 421 KB
- Delta Dental PPO™ Children's Dental PPO for Small Businesses 401 KB
- Delta Dental PPO™ Family Dental PPO for Small Businesses 419 KB
- Delta Dental Individual & Family™ DeltaCare® USA Family Dental HMO 435 KB
- DeltaCare® USA Children's Dental HMO for Small Businesses 431 KB
- DeltaCare® USA Family Dental HMO for Small Businesses 432 KB
- California Brochures
- Delta Dental PPO Premium Plan covers implants at 50%, after a 12-month waiting period.
- Delta Dental Individual & FamilyTM Delta Dental PPOTM Family Dental Plan 669 KB
- Delta Dental PPOTM Children’s Dental PPO for Small Businesses 790 KB
- Delta Dental PPOTM Family Dental PPO for Small Businesses 794 KB
- Delta Dental Individual & FamilyTM DeltaCare® USA Family Dental HMO 872 KB
- DeltaCare® USA Children’s Dental HMO for Small Businesses 837 KB
- Members Resource WebPage
- Find a Dentist
- FAQ's
- We are interested in the Delta Dental PPO Premium Plan but have a few questions:
- What do we need to give to Delta Dental to have the 6 month waiting period waived?
- Let's check the EOC Evidence of Coverage and Summary of Benefits
- Attachment A Footnote 3 just says acceptable documentation. I suggest that your ID card and proof of payment for 6 months will suffice.
- Prior coverage In certain cases, a waiting period will be waived if a comparable dental insurance plan was terminated in the 30 to 60 days prior to the effective date of your new plan, but your former dental plan must include very similar coverage. Delta *
- Let's check the EOC Evidence of Coverage and Summary of Benefits
- Our current policy does not include orthodontics. Would this affect the waiting period for just the orthodontic coverages in Delta’s plan.
- It's not clear in footnote 3. I would say no, as you don't have comparable orthodontic coverage.
- Send me your ID Card and proof of payment and I can ask Delta.
- Delta said Will need a letter from the prior insurance company with the effective and end date, also the type of coverage the client had.
- Do you have a summary of benefits for the plan you have now?
- Can you just get the letter and we can get an authoritative answer.
- I'll research if there is any more detail... Pre Existing Conditions like before ObamaCare
- Send me your ID Card and proof of payment and I can ask Delta.
- It's not clear in footnote 3. I would say no, as you don't have comparable orthodontic coverage.
- What is the process for us to purchase the Delta Dental PPO Premium Plan from you?
- Use the affiliate link above and enroll online.
- Do the 2 cleaning per calendar year have to be spaced out in 6 month intervals?
- Attachment b page 4 states they pay for 2/year. No requirement to space them out.
- What do we need to give to Delta Dental to have the 6 month waiting period waived?
- We are interested in the Delta Dental PPO Premium Plan but have a few questions:
- Broker ONLY
Dental For #Everyone,
has an excellent website with full brochures, Instant online quoting and enrollment
- One of our colleagues on how Dental for Everyone Works.
- Some of our webpages on dental
- VSP Vision
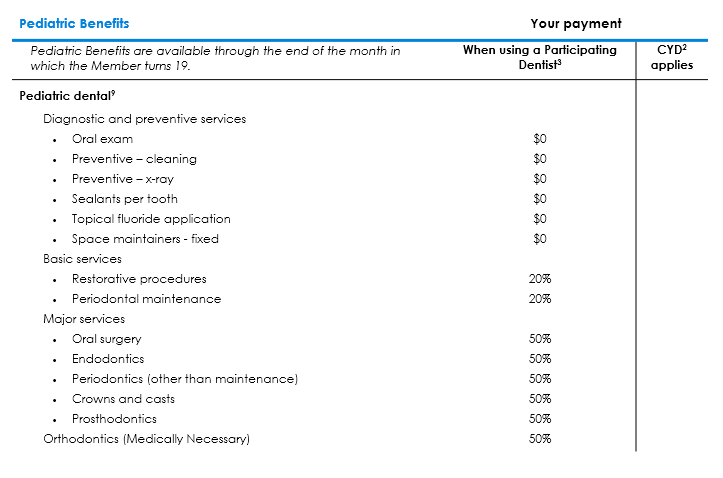
#Pediatric Dental and Vision
Pediatric Dental and Vision are Mandatory essential benefits under Section “J” 42 USC 18022 SB 951, even if there are no children on the policy. If there are no children, you are not getting charged see FAQ below for more detail.
- Resources & Links
- Blue Shield Trio HMO EOC Evidence of Coverage 2019 Page 50 for Dental & 112 for Vision
- Blue Shield Graphic on Pediatric Dental & Vision
- Covered CA – Ask us [email protected] or log into your account and click on Select Dental Plan in right hand side under Actions
- Delta Dental VIDEO Changes with Health Care Reform Pediatric Dental
- Children’s Vision Problems Often Go Undetected, Despite Calls for Regular Screening
Pediatric Dental from Summary of Benefits
Oral Health for #Seniors
Justice in Aging - Advocates Guide
- Denti-Cal under Medi Cal
- National Institute for Dental Research - Caregiver information
- Health.Gov tips for older adults
- nia.nih.gov/taking-care-your-teeth-and-mouth
- Dental Care - Medicare
Dental - Glossary – #Dictionary
- Golden West
- Sealants Fact Sheet
- Dental Site – Dr. Dorfman DDS Excellent Site for Dental Information
- Deep Cleaning explanation & coverage
- Dental Implants
- Sacramento Truck driver sudden dealth from tooth infection Sacramento Bee 1.31.2017
Dental FAQ’s
- Question What is Coordination of benefits – two or more policies in force?
. - Answer Basic and general rules on Coordination of Benefits
- .
- Question Is it worth it and safe to have dental coverage, during the pandemic as people are postponing routine cleaning, etc, during the pandemic?
. - Answer Blue Cross has already announced lower rates and that they are paying extra to the dentists for COVID 19 extra costs to prevent transmission.
- If no one goes to the dentist, under the Medical Loss Ratio rule, Insurance Companies will have to give rebates, so that they pay out 85 cents on every dollar they take in .
- Anthem issues premium credits to employer groups
- We continue to look for ways to provide support and financial relief to our employers and members during the COVID-19 emergency.
- Shelter-in-place orders across the country have caused significant disruption to traditional patterns of care. As a response to these challenges, we are supporting our customers by issuing premium credits to our Fully Insured employer groups based on their April 2020 invoices.
- The credits will appear on employers’ August 2020 invoices (issued in July 2020):
- • 15% of the April premium for Anthem Small Group medical plans
- • 50% of the April premium for Anthem Dental plans – Source – Broker Email 6.5.2020PPE reimbursement protects members and supports dentistsCOVID-19 requires that dentists take extra precautions to protect both themselves and their patients. These added steps can add to the cost of a dental visit.
- To protect the health of our members while minimizing unexpected fees, we are paying dentists an extra reimbursement from June 15 through August 31, 2020.
- Anthem will pay $10 per dental patient, per visit, on dental PPO network claims for personal protective equipment (PPE).
- Supporting the dentists in our networks can help preserve employee access to providers in their plans. Broker email dates 6.22.2020
.
- Question is it safe to go to the dentist?
. - Answer COVID-19 spreads primarily through respiratory droplets that often make their way into your mouth, nose, or even eyes, you may be putting yourself in danger while sitting in the dentist chair (remember: dental hygienists and dentists are all up in your mouth during cleanings and procedures—and you wearing a mask is basically impossible).
- Viral transmission can happen if someone isn’t showing symptoms yet, so even if a dental office is making staff who are showing symptoms stay home, that won’t be helpful if a staffer is asymptomatic. That said, “as long as the dentist and assistants wear masks and get tested,” a dental procedure can be perfectly safe if you’re experiencing any type of dental emergency—swelling, uncontrolled bleeding, pain, trauma from an accident, or if you have a dental concern related to an underlying condition (chemotherapy, uncontrolled diabetes, etc.)—it’s important to see your dentist as soon as possible since, again, many offices are still open for emergency procedures and visits.
- In the meantime, and again, as long as you’re not currently facing a dental emergency, remember to keep your teeth and mouth healthy by brushing your teeth and flossing twice a day (yes, even in quarantine). Learn more NPR.org 6.3.2020 Is it safe?
.
- questions to ask medical and dental staff when scheduling an appointment:
. - Answer
- Do the staff and patients wear masks at all times?
- Do the staff have enough masks and protective equipment?
- Will there be a limit on how many people can be in a waiting room?
- Are the staff being tested for COVID-19?
- How often are staff cleaning the waiting rooms and offices?
- If you don’t drive, can you take public transit while keeping your distance from other people and washing your hands before and afterward?Evidence of Coverage for Delta Dental PPOTimely Access to CarePPO and Premier Providers have agreed waiting times to Enrollees for appointments for care which will never be greater than the following timeframes:
- for emergency care, 24 hours a day, 7 day days a week;
- for any urgent care, 72 hours for appointments consistent with the Enrollee’s individual needs;
- for any non-urgent care, 36 business days; and
- for any preventative services, 40 business days.
- During non-business hours, the Enrollee will have access to his or her Provider’s answering machine, answering service, cell phone or pager for guidance on what to do and whom to contact if he or she is experiencing an Emergency Dental Condition.
- If the Enrollee calls our Customer Service Center, a representative will answer their call within 10 minutes during normal business hours.
- Should the Enrollee need interpretation services when scheduling an appointment with any of our PPO or Premier Providers, he or she may call our Customer Service Center at 800-471-0287 for assistance.
Technical & Research Resources
- webb dental.com/
- TMJ society.org/
- tmj.org/
- AB 2994, TMJ mandated if medically-necessary
Our other pages on
Dental Coverage
We don't put a lot of effort into selling dental coverage. Generally it's a wash on paying premiums vs getting back claims payments. Unless it's employer group. Then the premiums are tax deductible under IRS Section 106.
Here's more information on how we feel about dental. Here's our page on implants, where we get lots of inquires, but few sales. Most people only seem to want dental coverage, after they've been told they need a lot of dental work. Not profitable for Insurance Companies. See our other pages for details & explanations. See our page on Medical Loss Ratio. Insurance Companies need to take in $1 to pay 80c in claims.
Medicare Plans
- Anthem Blue Cross
- Blue Shield – Medi-Gap – Any Medicare Provider
- Health Net Medi Gap
- UHC AARP Medi Gap
- Scan
Individual & Family Plans
Dental For Everyone,
has an excellent website with full brochures, Instant online quoting and enrollment
One of our colleagues on how Dental for Everyone Works..
Employer Group Plans
- Medi-Cal





I have an employer group dental plan with Walmart that only coordinates with other group plans.
I’m interested in a Individual Delta Dental PPO.
What does their co-ordination of benefits say?
We’ve answered your question on our dual coverage page – Co-ordination of benefits.
Dr Brent Matza called in this prescription for me last week because I have a tooth that was growing under another and couldn’t be removed at that time .
I have a terrible infection or abscess in my jaw where tooth is infected under the gums.
I really need to get another presc of amoxicillin to finish clearing up the swelling and infection.
I can’t lay on that side of my cheek, right side jaw bone hurts bad.
I’ll be trying to find a dentist next week.
My prescriptions go in to Walgreens on Ming Ave in bakersfield CA 93309
Thanks for the compliment, asking us complex claims problems….
However, we are not the official claims site for Health Net or any dental insurer.
Please try the number on the back of your ID card.
If you have questions like, what gets covered by Health Insurance or what gets covered by dental, we can probably look that up, if you let us know exactly what policies you have. Here’s an example EOC Evidence of Coverage
If we don’t have access to your EOC Evidence of Coverage, then you’ll need to send them to us.
I am a 60 yr. old mother of adult children, no minors are covered under my individual policy, so how on earth can Pediatric Dental be “mandatory”,
Reply
That’s the law. Everyone has to have it. It’s an essential benefit. You are also required to have maternity. There is no charge for the dental though.
Next Question
It is a question of principle, not $6.89 additional monthly fee!
How come this fee is being padded after the contract was signed last year?
There is not a single thing, in my opinion, that has gone right with the roll out of Health Care Reform.
Our Reply
See my SNAFU page I’m doing twice or more work with less than ½ the pay. I especially resent that Covered CA (CC) advertising does not mention that one can buy from an agent. Worse, so many people think they can only buy from CC and only CC provides guaranteed issue. So, I’m certainly not making it up on volume. The policy is effective Jan 1, 2014.
Next Question
No one mentioned this earlier. It was the law though. For some reason, CC policies do not currently include pediatric dental, nor do I believe it’s available! After months of repeated requests and no resolution to auto payment, now someone decides to add mandatory fee retroactively and initiate auto payment. This is not right! It is unfair and a dishonest act. If the fee became mandatory after the policy was issued, wait till the renewal date of the policy at the end of 2014 and then add this fee.
What dental plan provides the most comprehensive coverage for “deep cleaning?”
Deep dental cleaning is also called periodontal scaling and root planning, or SRP. It’s similar to how a hygienist typically cleans your teeth but focuses on the outer surface of the roots and below your gum line. This special cleaning is needed when tartar buildup has caused infection of the gums. Pockets form, a widening of the gumline that has pulled away from the tooth. Loss of this connective tissue can lead to bone loss and, eventually, tooth loss. Learn More
The Difference: Deep Dental Cleaning vs Regular Cleaning
You Tube VIDEO on deep cleaning
Better VIDEO on deep cleaning
If you’re a dentist check out Spear Education.com
If you have recently sat in your dentist’s chair for a routine exam, or you plan to in the near future, you are already ahead of the 34% of Americans who skip their checkup.
Let’s set the record straight: if your dentist has suggested a deep cleaning, it is important that you get one scheduled right away. my ideal dental.com
Here’s how to avoid the need for a deep dental cleaning
You can prevent gingivitis and periodontal disease and avoid the need for a deep dental cleaning. “Probably 95 to 98% of dental disease, and periodontal disease in particular, is preventable,” Dr. Crum says.
Key to prevention is better home care. You’ve had the recommendations drilled into your head since you were a kid—brush twice a day and floss once a day. If traditional brushing and flossing aren’t cutting it for you, there are different home care tools you can try.
considerable.com
We have individual family Delta Dental HMO which is due for renewal at just $250/yr total premium
I need crown work so looking for best plan to move into that will offer the deepest discounts for crown, post, and root canal. My estimate for work is over $5,000
Please, when asking us to compare or advise on plans, let us know the exact plan you have, ages and how many people are covered.
Are you talking about the DeltaCare® USA CAA54 Individual/Family Dental Program Disclosure Contract
This plan does NOT have waiting periods and no annual maximums!
Are you happy with the dentists on the provider list?
How about appointing us as your agent on this plan?
One problem with dental, is that the premiums and thus the commissions are so low, we don’t really have time to shop and compare for you.
Thus, we suggest you use the shop & compare tools on our website like:
Dental for Everyone Which shops maybe 50 plans and allows side by side comparisons.
Scroll back up and visit our pages and compare benefits for Blue Cross, Blue Shield and Health Net
It’s also difficult for us as agents, as most people that ask about dental coverage, are in need of MAJOR services and facing huge bills. That’s not really something Insurance Companies are looking to pay immediate claims for.
Note also, that employer group plans often offer richer benefits, shorter waiting periods and higher maximums as there they are getting people that don’t need MAJOR services right away to make up or help pay for ones with immediate claims.