Find a therapist, psychologist who accepts Medicare & ACA Obamacare
Ways to #Find a Therapist
- Find Therapists that accept Medicare
- All Insurance Companies – Mental Health Provider Finder
- Psychology Today - Find a Provider
- More Americans Are Seeking Mental Health Care In A ‘Therapy Boom Read More Kff News
- One estimate suggests 42% of therapists in California don’t accept insurance at all. Without the financial help of insurance, clients pay an average of $130 out of pocket per session. It can be much higher in major cities. Read more: What's stopping therapists from providing affordable Mental Health Care?
- Helping employees find support for their mental health A quick view of Anthem’s behavioral health programs
- npr.org/mental-health-care-shortage-medicare-medicaid
Google Search for ONLINE Therapists
Here’s what I googled for online therapists. Check with them and ask what Insurance Plans they take. Then double check on the official Insurance Company provider list.
- A step-by-step guide to finding a therapist NPR
- 988 mental health hotline is live. Here's what to know NPR
- apa.org/online-therapy
- talk space
- amwell.com/online-therapy/
- break through.com/
- live health online.com/psychology
- psychologytoday.com/depression/ca/torrance
- meetup.com
- nami south bay.com/support-groups
- Anxiety & Depression Assoc of America Support Groups
- Patients Seek Mental Health Care From Their Doctor But Find Health Plans Standing in the Way
- Mental health patient directories rife with ‘phantom’ providers almost six out of 10 in-network providers listed under Oregon Medicaid provider directories are not actually available to see patients
How much does a therapist get to see you?
-
- Physician Fee Schedule CMS.gov
- Medicare Provider Finder
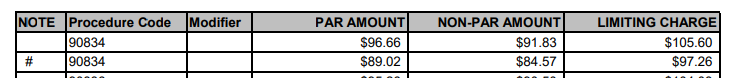
- 45-minute psychotherapy session (the most common mental health service) Medicare pays just $84.74 psychologists are leaving Medicare, reducing their Medicare patient loads, and stop taking new Medicare patients. APA Services.org
- Medicare Physician Fee Schedule 1.1.2019 Los Angeles Are 18
- 90834 Individual psychotherapy, 45 minutes
- # -These amounts apply when service is performed in a facility setting

- Question I am a provider and I can’t seem to find out rates Medi-Cal will pay for Behavioral Health codes. Client has primary and this would be for their secondary. Here is one of the codes- H2019. Can you help?
- Answer The Medi-Cal rates do not contain these codes so I called Medi-Cal where they told me they have the description of each code but not the rates and for me to call Medicare (Noridian Health Care Solutions) where they said Medicare does not cover these codes.
- I know that Medi-Cal covers but I can’t see to find rates for the codes we use. It’s for Behavioral health-ABA.
- CPT codes and maximum allowances for psychological services
- § 51505.3. Psychology Services. H2019 is a valid 2019 HCPCS code for Therapeutic behavioral services, per 15 minutes or just “Ther behav svc, per 15 min” for short, used in Other medical items or services. https://hcpcs.codes/h-codes/H2019/
- Therapists Flee Kaiser as Mental Health Patients Languish
- Why mental health providers say Medi-Cal’s latest reform may force them to cut services
To hear the sound, click on the sound button

in the video below.
@infantryguru Are you Ready to Be All You Can Be? This motivated me #military #army #miltok #motivational #beallyoucanbe #mind #powerfultool #rightnow #enhancethecorps ♬ Military – Florews
- Jump to section on:
Find Medicare Doctors who accept assignment #MD
- Medicare Video - Physician Compare
- Blue Shield Statement Medi Gap uses ANY Medicare MD!
- Care Compare Video
- Video on how to use Medicare Provider Finder VIDEO
- Our Webpage on Medicare Assignment – Doctor Participating or Not?
- Compare Hospitals - Search Medicare.gov
- Medicare Guide to Choosing a Hospital Publication # 10181
- Hospital Readmission Penalty Look Up
- Long-Term Acute Care Hospital (LTACH) Clinical Guidelines - Oscar
- US News & World Report America's Best Hospitals
- UCLA #3
- Cedar's Sinai # 6
- UCSF San Francisco #9
- Stanford #12
Mental Health ACA/Obamacare under 65
Read it directly in the Sample EOC Evidence of Coverage – Use Ctrl F search feature
#Individual Therapy
There are a lot of people suffering from a mental health condition who need therapy. And there are a lot of therapists who want to help them. But both sides believe the insurance companies that are supposed to bring them together are actually keeping them apart. Nearly half of therapists in California don’t take insurance as reimbursement rates don’t provide a living wage,
Most insurance companies pay therapists in their networks between $60 and $80 per session. In the San Francisco area and Los Angeles, therapists say the market rate for therapy is more like $150 to $200 a session.
“The second thing is the paperwork. For an hour of psychotherapy you spend a half-hour on paperwork, CA Health
Find a Support Group
Links & Resources
- psychology today.com/groups
- meet up.com/depression-support-group
- nami south bay.com/support groups
- d b s a south bay.org/ DEPRESSION AND BIPOLAR SUPPORT ALLIANCE – SOUTH BAY, TORRANCE
- Introduction to Therapy – Los Angeles Times 12,23.2020
- Low cost alternatives to therapy 9.22.2021
- FAQ on if Mental Health Therapist Benefits vary by Metal Level
- chabad.org/Ten-Hacks-for-Mental-Control-That-Every-Human-Being-Should-Know
- 10 Delusional Beliefs Held by Chronic Worriers Psychology Today
- Americans can wait many weeks to see a therapist. California law aims to fix that NPR 11.18.2021
- Senate Bill 221
- New California Law Makes It Easier to Get Care for Mental Health and Substance Abuse CA Health Line
- More than half of private practice therapists worry about economy, plan to raise rates in 2023, survey finds
- St. Dymphna, patron saint of mental health LA Times May 14, 2022
- it is essential that the healthcare industry reduce stigma, enhance affordability, and improve patient education surrounding mental health Athena Health
- Autism Resource Center – Magellan
Medicare Part B Outpatient Mental Health
- Medicare Part B (Medical Insurance) covers mental health services and visits with:
- Psychiatrist or other doctor
- Clinical psychologist
- Clinical social worker
- Clinical nurse specialist
- Nurse practitioner
- Physician assistant
- NAMI’s List of Mental Health Professionals
- Mental Health America’s list
- Your therapist must accept Medicare Assignment
- Part B covers outpatient mental health services, including services that are usually provided outside a hospital, like in these settings:
- A doctor’s or other health care provider’s office
- A hospital outpatient department
- A community mental health center
- Part B also covers outpatient mental health services for treatment of inappropriate alcohol and drug use.
- Part B helps pay for these covered outpatient services:
- One depression screening per year. The screening must be done in a primary care doctor’s office or primary care clinic that can provide follow-up treatment and referrals.
- Individual and group psychotherapy with doctors or certain other licensed professionals allowed by the state where you get the services.
- Family counseling, if the main purpose is to help with your treatment.
- Testing to find out if you’re getting the services you need and if your current treatment is helping you.
- Psychiatric evaluation.
- Medication management.
- Certain prescription drugs that aren’t usually “self administered”(drugs you would normally take on your own), like some injections.
- Diagnostic tests.
- Partial hospitalization.
- A one-time “Welcome to Medicare” preventive visit. This visit includes a review of your potential risk factors for depression.
- A yearly “Wellness” visit. This is a good time to talk to your doctor or other health care provider about changes in your mental health so they can evaluate your changes year to year.
- Who’s eligible?
- All people with Part B are covered.
- Your costs in Original Medicare
- You pay nothing for your yearly depression screening if your doctor or health care provider accepts assignment.
- 20% of the In Original Medicare, this is the amount a doctor or supplier that accepts assignment can be paid. It may be less than the actual amount a doctor or supplier charges. Medicare pays part of this amount and you’re responsible for the difference.
- Medicare-approved amount for visits to a doctor or other
- The Part B The amount you must pay for health care or prescriptions before Original Medicare, your prescription drug plan, or your other insurance begins to pay.
- If you get your services in a hospital outpatient clinic or hospital outpatient department, you may have to pay an additional An amount you may be required to pay as your share of the cost for a medical service or supply, like a doctor’s visit, hospital outpatient visit, or prescription drug. A copayment is usually a set amount, rather than a percentage. For example, you might pay $10 or $20 for a doctor’s visit or prescription drug. See Medicare Mental Health Booklet * Medicare.Gov
- If you have a Medicare Advantage Plan – Check the Summary or EOC Evidence of Coverage for more benefits.
- Medicare Advantage Plans – Part C
- Anthem MediBlue Plus
- Blue Shield 65 Plus – Inspire HMO 2022
- SNP Special Needs Plans
- United Health Care
- Sample EOC – Use Ctrl – F & Search for Mental Health MAPD plans must give at least the benefit you would get under Original Medicare
- See our webpages on
- Mental Health – ACA/Health Reform Mandated Essential Benefit
- Mental Health – Outpatient – Therapist – Medicare
- Resources – Mental Health – Conservatorship – FSP
- Organizing, Hoarding, & Cluttering
- Pre-Existing Conditions – ACA No more!
- Preventative Care – Wellness Visit – Medicare
- Corona Virus – How does Insurance Cover it? – Relief Programs
- Social Determinants of Health Togetherness – Loneliness
- Medicare Advantage
- SNP Special Needs Plans
- Medicare Advantage Plans – Part C
#Medicare & You - Mental Health

- Medicare & Mental Illness Publication # 10184
- Find therapists who accept Medicare Assignment
- Medicare Billing Etc Guidelines for Professionals
- Our Webpage on Medicare & Mental Health
- Mental Health
- Medicare.Gov on Mental Health
- EOC Evidence of Coverage - Plain English,
- Los Angeles Consumer Resources #Directory
- Los Angeles Times on low cost & free therapy alternatives
- NPR Mental Health & COVID
- Guide to Mental Health Benefits (The Mighty)
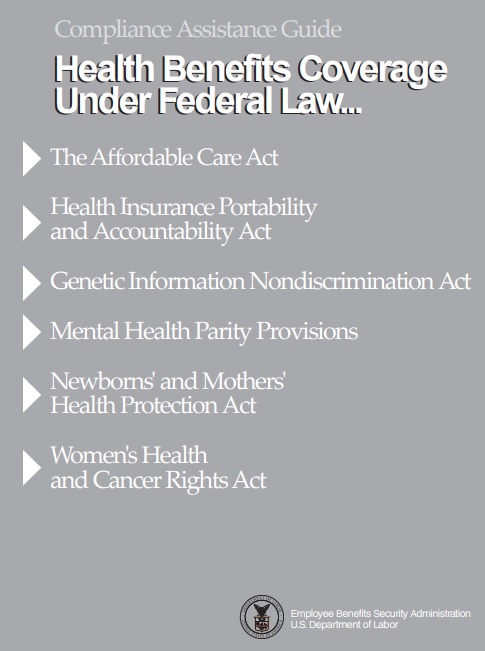
 Compliance Assistance Guide from DOL.Gov Health Benefits under Federal Law
Compliance Assistance Guide from DOL.Gov Health Benefits under Federal Law
- Mental Health Videos
- Veteran's Mental Health
- CMS Learning Aid for Mental Health Professionals
Behavioral health integration services
If you have a behavioral health condition (like depression, anxiety, or another behavioral health condition), Medicare may pay for a health care provider’s help to manage that condition if your provider offers the Psychiatric Collaborative Care Model.
The
Psychiatric Collaborative Care Model
is a set of integrated behavioral health services that includes care management support if you have a behavioral health condition. This care management support may include care planning for
- behavioral health conditions,
- ongoing assessment of your condition,
- medication support,
- counseling,
- or other treatments that your provider recommends.
Your health care provider will ask you to sign an agreement for you to get this set of services on a monthly basis. You pay a monthly fee, and the Part B deductible and coinsurance apply.
More Details & Limitations on Coverage
This article is intended for physicians, providers and suppliers submitting claims to Medicare contractors (carriers and/or Part A/B Medicare Administrative Contractors (A/B MACs) for mental health services provided to Medicare beneficiaries.
The Social Security Act (Section 1862(a)(1)(A)) excludes from coverage services that are not “reasonable and necessary for the diagnosis or treatment of an illness or injury or to improve the functioning of a malformed body member.”
This booklet gives the following Medicare mental health services information:
Covered and non-covered mental health services
- Eligible professionals
- Eligible professionals commonly used Current Procedural Terminology (CPT) codes
- National Correct Coding Initiative (NCCI)
- Provider charts
- Assignment
- Outpatient psychiatric hospital services
- Family psychotherapy (with the patient present and their treatment is the primary purpose) or (without the patient present, is medically reasonable and necessary, and their treatment is the primary purpose)
- Individual and group psychotherapy (individual therapy with one or more therapists and more than one individual in a therapy session with one or more therapists)
- Psychoanalysis (therapy that treats mental disorders by investigating the interaction of conscious and unconscious elements)
- Partial Hospitalization Program (PHP)
- Community Mental Health Centers (CMHC)
- Behavioral Health Integration (BHI) services
- Inpatient Psychiatric Facility (IPF) services
- Medical records requirements
- Coverage period
- Same day billing guidelines
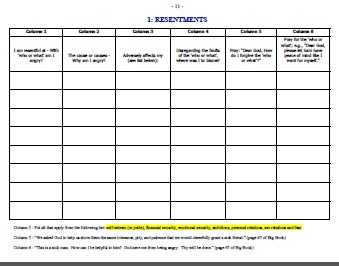
12 #Step Meetings & Therapist Confidentiality
The Twelve Traditions encourage members to practice the spiritual principle of anonymity in the public media and members are also asked to respect each other’s confidentiality.[42] This is a group norm,[42] however, and not legally mandated; there are no legal consequences to discourage those attending twelve-step groups from revealing information disclosed during meetings.[43] Statutes on group therapy do not encompass those associations that lack a professional therapist or clergyman to whom confidentiality and privilege might apply. Professionals and paraprofessionals who refer patients to these groups, to avoid both civil liability and licensure problems, have been advised that they should alert their patients that, at any time, their statements made in meetings may be disclosed.[43] wikipedia.org
Links & Resources
- Shouse Law – Therapist-Patient Privilege Evidence Code 1014
- CA Evidence Code Section 1014
- CA MFT.org
- Legislative Counsel Explanation
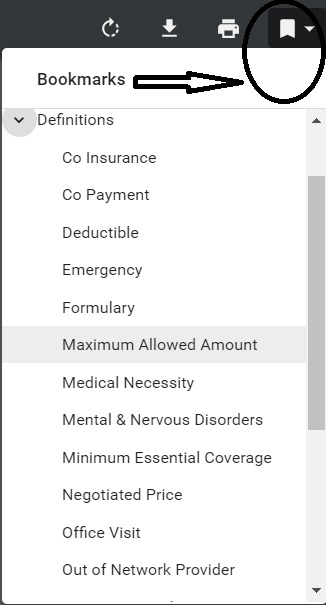
Specimen Individual Policy #EOC with Definitions
Employer Group Sample Policy
It's often so much easier and simpler to just read your Evidence of Coverage EOC-policy, then look all over for the codes, laws, regulations etc! Plus, EOC's are mandated to be written in PLAIN ENGLISH!
- Find your own Individual EOC Evidence of Coverage
- It' important to use YOUR EOC not just stuff in general!
- Obligation to READ your EOC
- Plain Meaning Rule - Plain Writing Act
- Our Webpage on Evidence of Coverage
- OOP Out of Pocket Maximum - Many definitions are explained there.







https://www.npr.org/sections/shots-health-news/2024/08/24/nx-s1-5028551/insurance-therapy-therapist-mental-health-coverage
https://www.axios.com/2024/12/18/psychologists-accept-health-insurance-survey
https://www.apa.org/news/press/releases/2024/12/insurance-challenges-limit-psychologists
https://news.blueshieldca.com/notice-of-data-breach