Continuity of Care Law California
Keep same doctors even if you change Insurance Plans or Networks…
Continuity of care
Continuity of care definition means that you may be able to use a Non-Participating Provider if your provider leaves your insurance companies network, or if you are a newly-covered Member whose previous health plan was withdrawn from the market. (Please follow the links and requests for care, it may be that any prior plan counts)
You can request to continue treatment with your Non-Participating Provider in the situations described above if you are currently receiving the following care:
Ongoing treatment for an acute or serious chronic condition;
Pregnancy care, including care immediately after giving birth;
Treatment for a terminal illness; FYI see also Hospice
Other services authorized by a now-terminated provider as part of a documented course of treatment; or
Care for a child up to 36 months old.
To request continuity of care, fill out your Insurance Companies Continuity of Care Application. and show Medical Necessity.
The Non-Participating Provider Finder must agree to accept your Insurance Companies Allowed Charges as payment in full for your ongoing care. If the provider agrees and your request is authorized, you may continue to see the Non-Participating Provider at the Participating Provider Cost Share for:
Up to 12 months; or
If you have a terminal illness, for the duration of the terminal illness. * Sample Group Health Plan * Excerpt from Blue Shield Trio Silver HMO EOC
See the Your payment information section for more information about the Allowed Charges.
- Health Net Continuity of Care Assistance Request Forms
- Policy Details
- Blue Shield FAQ 2.2022 5 pages
- Blue Shield explanation 9 pages
- Request for Continuity of Care
- LA Care Explanation
- Sample Group Health Plan *
- dmhc.ca.gov/continuity of care
- See the Advocates Guide to Surprise Medical Bills
- Medi Cal – Continuity of Care dhcs.ca.gov
- Anthem Info & Link to request for Continuity of Care
Jump to section on:
Medi-Cal Managed Care HMO – Health Care Options
Here you can review and choose the HMO that you want to deliver your Medi-Cal health Care.
Learn more:
- Disability Rights.org –
- What are Medi Cal Managed Care Plans? What do I need to know?
- Medi-Cal Managed Care Health Plan Directory
- Medi-Cal Listing of HMO plans by county *
- Medi-Cal Managed Care Provider Search
- Medi Cal HMO – Managed Care Providers by County
- health care options.dhcs.ca.gov/tips-help-you-choose-medical-plan
- health care options.dhcs.ca.gov/frequently-asked-questions-faqs
- California’s County-Based Health Plans 2022 CHCF
- Medi-Cal’s Fragmented System Can Make Moving a Nightmare Read More CA Health Line *
- Poor Care Co-Ordination? New contracting process Deficient Oversight CA Health Line *
- Disability Rights – Medi Cal provider HMO’s, what are they? What do I need to know about them?
- Medi-Cal Managed Care – Health Care Options
- EOC’s, Forms & Income Charts from Insure Me Kevin.com
- Sacramento? dhcs.ca.gov//mmcd health plan dir
- Battle Lines Are Drawn Over California Deal With Kaiser Permanente
- Exemption from enrolling in a Health Care Plan
- health care options.dhcs.ca.gov - Download Forms
- You May Get A Medical Exemption If:
- You have a complex medical condition; AND
- The care you get from your Regular Medi-Cal doctor for the complex medical condition cannot be changed, because your condition could get worse; AND
- Your Regular Medi-Cal doctor is NOT part of a plan in your county. You may see more than one Regular Medi-Cal doctor. If you do, have the form filled out by the doctor who sees you most often. Ask your Regular Medi-Cal doctor if he or she is part of a Plan in your county. This should be done before you submit this form.
- You have a complex medical condition; AND
- Provider Search – Statewide Fee for Service
- See our webpage on IMR Independent Medical Review
Technical Legal Information
#Continuity of Care
California Senate Bill SB 133
If you buy your own coverage and your current plan leaves the market your new plan must cover treatment by the same physicians, even if they are not in the new insurer’s network.
The provision would apply for enrollees under treatment for a chronic, acute or terminal illness, and in cases of pregnancy. The coverage would be contingent on the doctor accepting the payment offered by the new health plan, and the insurer would have to continue covering the services of that provider for up to one year. The coverage could extend beyond a year if the patient were terminally ill.
Similar protections already exist for people with job-based insurance policies that are under the purview of state regulators. CA Healthline
LEGISLATIVE COUNSEL’S DIGEST
… Existing law requires a health care service plan and a health insurer that provides services at alternative rates of payment, at the request of an enrollee or insured, to provide the completion of services by a terminated provider if the enrollee or insured is undergoing a course of treatment for one of any specified conditions, including a serious chronic condition… Existing law also requires a health care service plan to provide for the completion of covered services by a nonparticipating provider to a newly covered enrollee who, at the time his or her coverage became effective, was receiving services from that provider for one of any specified conditions. Existing law prohibits completion of covered services for a serious chronic condition from exceeding 12 months from the contract termination date or 12 months from the effective date of coverage for a newly covered enrollee or insured. Existing law requires a health care service plan to provide a disclosure form regarding the benefits, services, and terms of a plan contract and requires the disclosure form to include a description of how an enrollee can request continuity of care under the provisions described above.
This bill would provide that an enrollee or insured who has a condition that will require a transplant is not limited by the 12-month period described above and would require the completion of covered services to be provided for the duration of the condition and until the time he or she undergoes the transplant surgery and receives the necessary followup care that is consistent with good professional practice.
***
Continuity of Care?
California Assembly Bill AB 369
California Bill AB 369 requires a health plan, at the request of a newly covered enrollee under an individual contract, or a health insurer at the request of a new covered insured under an individual insurance policy, to arrange for the completion of covered services by a non-participating provider for one of the conditions specified in existing law, if the new covered enrollee or insure meets both of the following:
- Had coverage that was terminated between December 1, 2013 and March 31, 2014, inclusive because the plan or insurer ceased to provide or arrange health benefits or the plan or insurer withdrew from the market; and,
- At the time coverage became effective, the newly covered enrollee or insured was receiving services from that provider for one of the specified condition. healthnet pulse.com
- special-enrollment-triggering-events/md-network/
- Blue Shield 1 page summary
- dmhc.ca.gov/continuity of care
- California Code of Regulations 22, § 53286 – Continuity of Care
- AB 1286 Frommer 2004
- AB 369 2014
- Commonwealth Fund explanation of ACA/Obamacare and it’s effect on State Law 4.13.2016
- Blue Shield Flyer on Continuity of care
- SB 133 fact sheet
#Transfer Rights for Continuity of Care with the Same Doctor
.
10133.56. (a) A health insurer that enters into a contract with a professional or institutional provider to provide services at alternative rates of payment pursuant to Section 10133 shall, at the request of an insured, arrange for the completion of covered services by a terminated provider, if the insured is undergoing a course of treatment for any of the following conditions:
(1) An acute condition. An acute condition is a medical condition that involves a sudden onset of symptoms due to an illness, injury, or other medical problem that requires prompt medical attention and that has a limited duration. Completion of covered services shall be provided for the duration of the acute condition.
.
(2) A serious chronic condition. A serious chronic condition is a medical condition due to a disease, illness, or other medical problem or medical disorder that is serious in nature and that persists without full cure or worsens over an extended period of time or requires ongoing treatment to maintain remission or prevent deterioration. Completion of covered services shall be provided for a period of time necessary to complete a course of treatment and to arrange for a safe transfer to another provider, as determined by the health insurer in consultation with the insured and the terminated provider and consistent with good professional practice. Completion of covered services under this paragraph shall not exceed 12 months from the contract termination date.
.
(3) A pregnancy. A pregnancy is the three trimesters of pregnancy and the immediate postpartum period. Completion of covered services shall be provided for the duration of the pregnancy.
.
(4) A terminal illness. A terminal illness is an incurable or irreversible condition that has a high probability of causing death within one year or less. Completion of covered services shall be provided for the duration of a terminal illness, which may exceed 12 months from the contract termination date.
.
(5) The care of a newborn child between birth and age 36 months. Completion of covered services under this paragraph shall not exceed 12 months from the contract termination date.
.
(6) Performance of a surgery or other procedure that has been recommended and documented by the provider to occur within 180 days of the contract’s termination date.
- Laws may change FASTER than we can keep up. Be sure to visit the State of CA website on Insurance Law, before using anything in a citation.
- AB 369 HN Bulletin Continuity of Care health net pulse.com
- Medicare Advantage Plans in 2015 will allow you to opt out if the MD Network is significantly changed.
- medicare-advantage-plans/#comment-11065 carriers have been notifying clients if during the year a provider chooses to cancel their HMO contract since those folks have to pick a new PCP
All our plans are Guaranteed Issue with No Pre X Clause
Quote & Subsidy #Calculation
There is No charge for our complementary services
Watch our 10 minute VIDEO
that explains everything about getting a quote
- Our Quote Engine Takes all the complexity out of using pencil and paper to figure out the premiums per the Obamacare/ACA rules under CFR §1.36B-3 *
- Get more detail on the Individual & Family Carriers available in CA
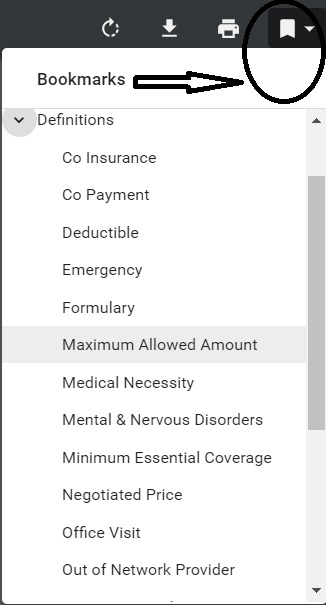
Specimen Individual Policy #EOC with Definitions
Employer Group Sample Policy
It's often so much easier and simpler to just read your Evidence of Coverage EOC-policy, then look all over for the codes, laws, regulations etc! Plus, EOC's are mandated to be written in PLAIN ENGLISH!
- Find your own Individual EOC Evidence of Coverage
- It' important to use YOUR EOC not just stuff in general!
- Obligation to READ your EOC
- Plain Meaning Rule - Plain Writing Act
- Our Webpage on Evidence of Coverage
- OOP Out of Pocket Maximum - Many definitions are explained there.
VIDEO Steve Explains how to read EOC
#Covered CA Certified Agent
No extra charge for complementary assistance
- Get Instant Health Quotes, Subsidy Calculation & Enroll
- Appoint us as your broker
- Get Instant Health Quotes, Subsidy Calculation & Enroll
- Videos on how great agents are








I might be losing Medi-Cal as I’ll be making too much money.
I have chronic pain, and am prescribed an opioid to control it.
Because it’s a controlled substance, I can get only a 30 day supply of pain meds at a time.
However, if I were to transition out of Medi-Cal and go with a new health care provider, it could take 90+ days to see a new specialist who could prescribe pain meds
So there would be a 60+ day gap of no pain meds, not good.
Would “continuity of care” apply to me?
Looks to me like it would. Ask your current MD if he would accept payment from the new Insurance Company. Here’s where to get quotes and subsidy calculation.
When you decide what company you want, then we can get you the proper forms. You can also check the new companies provider finder by clicking on the link in the quote in the lower right, just above where it says “add to cart”
You can get more detailed information on all companies here.
My son was diagnosed with Hodkins Lymphoma in June 2018 and he will turn 26 in April 2020. He is on my UHC health care plan through my employer. He is in remission currently but will need maintenance treatment that goes beyond his birthday next year.
1) Can he get a waiver from UHC to continue the treatment just to complete this maintenance treatment, several months after his birthday, say to the middle or end of 2020?
Please read this page carefully, 3 times and then when you think you understand it, read it again. Justice Felix Frankfurter.
Continuity of care and I’ve only read this page ONE time, seems to only apply to a new company taking over care, nothing to force a current company to continue coverage.
Check out COBRA, Disabled Children and of course an individual plan under ACA/Obamacare would be guaranteed issue, no pre x and when you lose coverage, you have a special enrollment. Get quotes here.