SNP Special Needs Plan
& Medi Medi – Cal Medi Connect
Medicare MAPD Special Needs #SNP
& Chronic Condition – C-SNP Plan?
Definition:
To enroll in a Medicare SNPs you must have one of these specific diseases or characteristics. Medicare SNPs tailor their benefits, provider choices, and drug formularies to best meet your specific needs. Medicare.gov
There are three different types of SNPs:
- Chronic Condition SNP (C-SNP)
- Dual Eligible SNP (D-SNP) Medicare & Medi Cal
- Institutional SNP (I-SNP) cms.govSpecialNeedsPlans *
Medicare SNPs CMS.gov also see Special Needs Plans are subtype of Medicare Advantage Plan.
- Can I get my health care from any doctor, other health care provider, or hospital?
- You generally must get your care and services from doctors, other health care providers, or hospitals in the plan’s network (except emergency care, out-of-area urgent care, or out-of-area dialysis).
- Prescription drugs
- Yes. All SNPs must provide Medicare prescription drug coverage (Part D).
- Do I need to choose a primary care doctor?
- Generally, yes.
- Do I have to get a referral to see a specialist?
- In most cases, yes. Certain services, like yearly screening mammograms, don’t require a referral.
- What else do I need to know about this type of plan?
- A plan must limit membership to these groups:
- 1) people who live in certain institutions (like nursing homes) or who require nursing care at home, or
- 2) people who are eligible for both Medicare and Medicaid, or
- 3) people who have specific chronic or disabling conditions (like diabetes, End-Stage Renal Disease, HIV/AIDS, chronic heart failure, or dementia).
- Check with us, there might be additional rules [email protected]
- A plan must limit membership to these groups:
- Plans will coordinate the services and providers you need to help you stay healthy and follow doctors’ or other health care providers’ orders.
- Scan Foundation Summary on Chronic Care Act
- Forbes *
- Social Services
- SNP plans may also offer home-delivered meals, transportation for nonmedical needs, pest control, indoor air quality equipment (e.g., air conditioner for someone with asthma), and minor home modifications (e.g., permanent ramps, widening of hallways or doorways to accommodate wheelchairs).
- Learn More
- Health IT.gov *
- Model of Care - HRA - Blue Shield Promise
- Telehealth *
- Modern Health Care *
- Oscar TeleHealth
- Medicare Managed Care Manual Chapter 16-B: Special Needs Plans
- cms.gov/Special-Need-Plans-SNP-Frequently-Asked-Questions-FAQ
- Taking Stock of Medicare Advantage: Special Needs Plans Commonwealth Fund
- Our webpage on
- Proposed Rule 2023 to lower out of pocket Medicare Part D prescription drug costs and improve consumer protections, reduce disparities, and improve health equity in Medicare Advantage (MA) and Part D. CMS.Gov Fact Sheet *
-
SNP enrollment is year around.
- Learn More

- Instant quotes & #Enrollment for Individual & Family
- Get the latest and most updated information.
- Medicare information contact us [email protected]
- Employer Small Group Health Proposals - Quotes
- We’re here to help you with any enrollment, selection and service questions you might have. Anthem pays us to help you at no extra charge! Check out the brochures below and on either side.
Diabetes C SNP
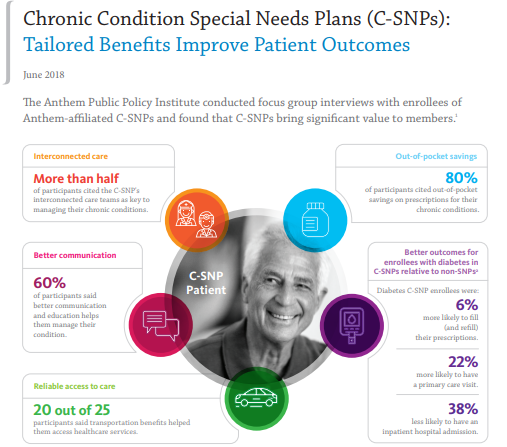
If you have Medicare and diabetes you can enroll in chronic condition special needs plans (C-SNPs). Surveys show members experience better outcomes than you would in regular Medicare Advantage (MA) plan. The survey used a claims-based approach to compare member outcomes on five clinical and utilization measures, Avalere found that enrollees in a diabetes-focused C-SNP were:
• 22 percent more likely to have a primary care visit,
• 10 percent more likely to receive appropriate diabetes testing,
• 38 percent less likely to have an inpatient hospital admission,
• 32 percent less likely to have a readmission, and
• 6 percent more likely to fill (and refill) a prescription for an antidiabetic medication.
These findings held true when controlling for expected differences in enrollees’ demographics and health status. The analysis suggests that C-SNPs can improve outcomes for beneficiaries with diabetes compared to non-SNPs. AnthemInc.com * Avalere.com *
Los Angeles & Orange County
Email us [email protected] for the most current documents or visit Blue Cross’s affiliate website.
No extra charge for our services & expertise.
- Summary of Benefits –
- Evidence of Coverage
- See page 7 of the EOC Special eligibility requirements for our plan Our plan is designed to meet the specialized needs of people who have certain medical conditions. To be eligible for our plan, you must have diabetes mellitus. NIH.Gov *
- To determine eligibility for a special needs individual to enroll in a C-SNP, CMS requires that the C-SNP contact the applicant’s existing provider – doctor to verify that the enrollee has the qualifying conditions. C-SNPs must reconfirm a beneficiary’s eligibility at least annually. CMS.gov *
- Sample Pre Enrollment Qualification Assessment
- Wellcare
- Health Net
- Sample Pre Enrollment Qualification Assessment
- To determine eligibility for a special needs individual to enroll in a C-SNP, CMS requires that the C-SNP contact the applicant’s existing provider – doctor to verify that the enrollee has the qualifying conditions. C-SNPs must reconfirm a beneficiary’s eligibility at least annually. CMS.gov *
- The Coverage chart is on page 50 of the EOC. If it changes with annual revisions, just use the table of contents or search feature.
- SNP FAQ’s from CMS Site
- See page 7 of the EOC Special eligibility requirements for our plan Our plan is designed to meet the specialized needs of people who have certain medical conditions. To be eligible for our plan, you must have diabetes mellitus. NIH.Gov *
- Our webpage on Diabetes – Prevention & Coverage under Medicare & ACA
Try turning your phone sideways to see the graphs & pdf's?
Special Needs Plans * #11302 Outdated 11.2011 *
- Our webpage on Special Needs Plans
- 10 Things to Know About Medicare Advantage Dual-Eligible Special Needs Plans (D-SNPs) KFF.org
- Taking Stock of Medicare Advantage: Special Needs Plans Commonwealth Fund
- Medicare Special Needs Plans CMS.gov
- What is a Special Needs Plan? CMS.gov
- Special Needs Plans Medicare.Gov
- Congress Considers Strategies To Improve Medicare And Medicaid Integration For Dual-Eligible Individuals Medicare & Medi Cal

- Instant quotes & #Enrollment for Individual & Family
- Get the latest and most updated information.
- Medicare information contact us [email protected]
- Employer Small Group Health Proposals - Quotes
- We’re here to help you with any enrollment, selection and service questions you might have. Anthem pays us to help you at no extra charge! Check out the brochures below and on either side.
Medicare Coverage for Diabetes # 11022
VIDEO's
- Diabetes Official Medicare VIDEO
- Max Insulin Co Pay $35
- Sugary Drinks - No Good VIDEO
- HBO Weight of the Nation VIDEO
- Fed UP – Official Trailer VIDEO
- Beat Diabetes – VIDEO You Tube - A trip to the grocery store
- Trump – Lower Cost of Insulin 5.26.2020 VIDEO
- How to use Medicare Part D Rx Plan Finder VIDEO
- Our main webpage on diabetes
- Rated – Surcharged Policies Pre Existing Conditions
Medicare Coverage of Kidney Dialysis and Transplants # 10128
- Average Billed Charges – 2017 Transplant Kidney - $414k
- Transplant Costs & Insurance - Kidney.org
- Medicare and People with Disabilities: An Overview–Hi Cap
- Medicare and People with End Stage Renal Disease (ESRD) Hi Cap
- No Cash, No Heart. Transplant Centers Require Proof Of Payment. CA Health Line
- Rated – Surcharged Policies Pre Existing Conditions
#My Medi-Cal
How to get the Health Care
You Need
24 pages
Smart Phones - try turning sideways to view pdf better
-
- More explanation

- Enroll with Benefits Cal
- What is Medi Cal - VIDEO
-
How to VIDEO
-
Medi-Cal Managed Care HMO – Health Care Options
- Benefits Cal is a one-stop-shop to apply for...
- Cal Fresh
- Ages 26 through 49 Adult Full Scope Medi-Cal Expansion regardless of immigration status
- Cal WORKs
- Medi-Cal
- CMSP (County Medical Services Program)
- Disaster Cal Fresh
- GA/GR (General Assistance and General Relief )
- Briefing — Medi-Cal Explained: An Overview of Program Basics
- chcf.org/medi-cal-explained/
- #BenefitsCal is a one-stop-shop to apply for...
- Medi-Cal
- County Medical Services Program (CMSP),
- Food Assistance - Cal Fresh (formerly known as Food Stamps)
- How to use Eat Fresh.org VIDEO
- Cooking & Nutrition
- California Work Opportunity and Responsibility to Kids (CalWORKs) or check their other website
- Medi-Cal
-
Here you can review and choose the HMO that you want to deliver your Medi-Cal health Care.
-
BIC Benefits Identification Card
InsuBuy International Medical Coverage –
Instant Quotes & Enrollment
Coverage for Travel - $50k Emergency under Medicare Medi Gap or MAPD Advantage may not be enough!
Chronic Conditions #List
- Chronic alcohol and other dependence
- Autoimmune disorders
- Cancer (excluding pre-cancer conditions)
- Cardiovascular disorders
- Chronic heart failure
- Dementia
- Diabetes mellitus
- End-stage liver disease
- End-Stage Renal Disease (ESRD) requiring dialysis (any mode of dialysis)
- Severe hematologic disorders
- HIV/AIDS
- Chronic lung disorders
- Chronic and disabling mental health conditions
- Neurologic disorders
- Stroke cms.gov/C-SNPs * Medicare.gov * cms.gov/Special-Need-Plans-SNP-Frequently-Asked-Questions-FAQ *CMS – Medicare – List of conditions for Special Needs Plans
Chronic care management services
- If you have 2 or more serious, chronic conditions (like arthritis, asthma, diabetes, hypertension, heart disease, osteoporosis, and other conditions) that are expected to last at least a year, Medicare may pay for a health care provider’s help to manage those conditions.
- This includes a comprehensive care plan that lists your health problems and goals,
- other health care providers, medications, community services you have and need, and
- other information about your health.
- It also explains the care you need and how your care will be coordinated.
- Your health care provider will ask you to sign an agreement to provide this service. If you agree, he or she will prepare the care plan,
- help you with medication management,
- provide 24/7 access for urgent care needs,
- give you support when you go from one health care setting to another,
- review your medicines and how you take them, and
- help you with other chronic care needs. You pay a monthly fee, and the Part B deductible and coinsurance apply. medicare.gov/10050-Medicare-and-You
Links & Resources on Chronic Care
- Blue Cross Explanation
- Nolo.Com
- CA Health Advocates.org
- CA Dept of Aging – HICAP (Local SHIP) – Center for Health Care Rights – 1-800-434-0222
- Medicare Managed Care Manual – SNP Chapter 16 B
- Wikipedia
- Management Services
- Aetna.com Model of Care
- The MOC provides the basic framework under which the SNP will meet the needs of each of its enrollees. The MOC is a vital quality improvement tool and integral component for ensuring that the unique needs of each enrollee are identified by the SNP and addressed through the plan’s care management practices. The MOC provides the foundation for promoting SNP quality, care management, and care coordination processes CMS.Gov *
- Vantage Health Plan Annual Training
- Cal Broker Magazine
FAQ’s ESRD – Special Needs Plan for Kidney Failure ”
- if one gets a transplant and no longer requires dialysis, can they stay on a ESRD SNP Plan?
- Let’s check the Evidence of Coverage – almost 300 pages of plain English to explain just about everything
- The only time we are allowed to cancel you, is if you no longer have the medical condition required for enrollment in Anthem MediBlue ESRD (HMO C-SNP). Page 238 of EOC
- Special eligibility requirements for our plan Our plan is designed to meet the specialized needs of people who have certain medical conditions. To be eligible for our plan, you must have end-stage renal disease requiring dialysis (any mode of dialysis).
- So, hopefully when you no longer require dialysis you’ll have a special enrollment period to pick another Medicare Advantage Plan. Page 7 of eoc
- Source medicareinteractive.org/SEP-Chart
- Here’s a definition of how bad ESRD must be to qualify.
- We can help you enroll in a MAPD plan with Blue Cross, Blue Shield & UHC, no additional charge.
- There might – it’s a long shot be a way to enroll in Medi Gap – under one of the guaranteed issue provisions?
- How old are you?
- Let’s check the Evidence of Coverage – almost 300 pages of plain English to explain just about everything
- Might you lose Medicare, and need an under 65 plan if you no longer qualify as ESRD?
- Nope, you won’t lose Medicare per page 6 of the Medicare Booklet on Kidney Dialysis & Transplant services
I live in Los Angeles and I’m on a transplant waiting list in Washington State. Will a Medicare Advantage Plan pay my expenses out of state
- Nope, you won’t lose Medicare per page 6 of the Medicare Booklet on Kidney Dialysis & Transplant services
- National Kidney registration? kidney.org/transplant-waitlist
The United Network for Organ Sharing (UNOS) manages the list of all the people across the US waiting for an organ transplant. UNOS ensures that deceased donor organs are distributed fairly using a transparent system - transplant living.org/how-could-i-get-a-transplant-sooner/
There are different kinds of donated kidneys – some with shorter wait times. It will be your job to choose which of these kidneys you’re willing to take – being open to more than 1 kind may make your wait shorter. - On the other hand:
- organjet.com OrganJet provides an information service, as well as options for timely and affordable air transport, for patients who are multi-listed or distant listed for organ transplants in the U.S.
- (Did you know that 500+ kidneys are wasted every year while 90000+ people wait on the list? We believe that we can improve the system and are working towards it.)
- In the meantime, you can likely get a transplant earlier by listing smartly.
- What are network providers?
- Network providers are the doctors and other health care professionals, medical groups, durable medical equipment suppliers, hospitals and other health care facilities that have an agreement with us to accept our payment, and any plan cost sharing, as payment in full. We have arranged for these providers to deliver covered services to members in our plan. The most recent list of providers and suppliers is available on our website at https://shop.anthem.com/medicare/ca.
- Why do you need to know which providers are part of our network?
- It is important to know which providers are part of our network because, with limited exceptions, while you are a member of our plan, you must use network providers to get your medical care and services.
- The only exceptions are emergencies, urgently needed services when the network is not available (generally, when you are out of the area), out-of-area dialysis services and cases in which the plan authorizes use of out-of-network providers. See Chapter 3 (Using the plan’s coverage for your medical and other covered services) for more specific information about emergency, out-of-network and out-of-area coverage.
- If you don’t have your copy of the Provider/Pharmacy Directory, you can request a copy from Customer Service (phone numbers are printed on the back cover of this booklet). You may ask Customer Service for more information about our network providers, including their qualifications. You can also see the Provider/Pharmacy Directory at https://shop.anthem.com/medicare/ca or download it from this website. Both Customer Service and the website can give you the most up-to-date information about changes in our network providers.
- Getting an exception is pushing the limits of our pay grade. See also our webpages on medical necessity and appeals.
- I checked with “my people” at Caremore and they advise that you NOT change plans as it may put in at the bottom of the waiting list!
- Thus, I think your “battle” would be with Medi Cal to pay the 20% that Medicare doesn’t pay.
- Medi-Cal pays out of state when:
540-1 (a) (5) When an out-of-state treatment plan has been proposed by the beneficiary’s attending physician and the proposed plan has been received, reviewed and authorized by the Department before the services are provided; and the proposed treatment is not available from resources and facilities within the State. - https://www.law.cornell.edu/cfr/text/42/431.10
- Medi Cal Treatment Authorization Request
#Understanding Medicare Advantage Plans (PDF) #12026
- MAPD Plans look like a great deal, as the "premium" is paid by fee from the Federal Government, on average $2k/year.Kff * MAPD Plans must cover all A & B services Medicare.Gov * generally they also cover Part D Rx.
- That's why the premium is very low or ZERO!
- Set a Zoom Meeting
- We can now do SOC Scope of Appointment, before the Meeting via a 3 minute recorded meeting 2 days before. AHIP Training Module 4 Page 14 *
- #Intake Form Berwick Needs Assessment Form - We can better prepare for the meeting
- Medicare Advantage (Medicare Part C): An Overview Hi Cap
- HMO - Narrow Networks?
- HI Cap CA Health Care Advocates Fact Sheet
- Do I just sign up with a Medicare Advantage Company and automatically get * Parts A & B or do I have to get those from Medicare.Gov * VIDEO
- Get Quotes, Full Information and Enroll
- MANDATED wording!: Think Advisor * ‘‘We do not offer every plan available in your area. Any information we provide is limited to those plans we do offer in your area. Please contact Medicare.gov or 1–800–MEDICARE to get information on all of your options.’’
- We disagree with the above wording, as we can use the same tools on Medicare.gov as they do!
- FYI a 4.27.2022 HHS Office of the Inspector General report found that MAPD plans denied 13% of prior authorizations that would have been covered under original Medicare (Conversely, Medi Gap, just follows what Medicare pays.)
- 88% of MAPD enrollees are happy
-
MAPD plans often include Dental & Part D - Rx Prescriptions and often have NO premiums!
-
How is that possible?
-
The Federal Government pays them around $700/month to handle your medical care. You must continue to pay your Medicare Part B premium of about $170/month. It's best to apply when you turn 65 for the supplement plans or advantage plans, as that's the main "Open Enrollment" period, guaranteed issue for any plan.
-
-
-
Medicare Advantage Plans also have an annual open enrollment now known as AEP Annual Election Period October 7 to December 15th.
-
Additional Coverage is important as Medical Bills are increasing Seniors Credit Card Debt or leading to possible bankruptcy?
- If You Have Problems with Your Medicare Advantage Plan
- forbes.com/how-insurers-can-navigate-the-costs-of-medicare-advantage-benefits
- politico.com/medicare-advantage-plans-congress
- Uncle Sam wants you to help stop insurers' bogus Medicare Advantage sales tactics
- ca health advocates/using-ai-to-deny-care
- Dodging the Medicare Enrollment Deadline Can Be Costly
- Medicare Advantage Increasingly Popular With Seniors — But Not Hospitals and Doctors
- Medicare Advantage is bad for patients and bad for investors
- When Medicare Advantage Plans Terminate Coverage
- Medi-Cal D-SNP Feasibility Study
Brother - Sister - Sibling Side Pages Subpages
View our website with your Desktop or Tablet for the most information