How to get Medicare Coverage if you have End Stage Renal Disease? (ESRD)
Chronic Kidney Disease?
Need Dialysis
How to get Medicare Coverage if you have End-Stage Renal Disease (ESRD)
You can get premium-free Part A Hospital if you get regular dialysis treatments or need a kidney transplant, have filed an application for Medicare, and meet 1 of the following conditions:
- Have worked the required amount of time under Social Security, the Railroad Retirement Board (RRB), or as a government employee; or
- Are getting or are eligible for Social Security or RRB benefits; or
- Are the spouse or dependent child of a person who has worked the required amount of time under Social Security, the RRB, or as a government employee; or are getting Social Security or RRB benefits.
Part A Hospital coverage begins:
- The 3rd month after the month in which a regular course of dialysis begins;
- See FAQ for more detail, or
- The first month a regular course of dialysis begins if the individual engages in self-dialysis training; or
- The month of kidney transplant;
- FAQ for more detail,
- Transplant Costs & Insurance -Kidney.org or
- Two months prior to the month of transplant if the individual was hospitalized during those months in preparation for the transplant. Citations – (CMS) * Publication 10128 Page 6 *
- FAQ about full recovery after transplant and special enrollment to get new coverage
- Part A & B Enrollment – Sign Up?
Resources & Links
Medicare Coverage of Kidney Dialysis and Transplants # 10128
- Average Billed Charges – 2017 Transplant Kidney - $414k
- Transplant Costs & Insurance - Kidney.org
- Medicare and People with Disabilities: An Overview–Hi Cap
- Medicare and People with End Stage Renal Disease (ESRD) Hi Cap
- No Cash, No Heart. Transplant Centers Require Proof Of Payment. CA Health Line
- Rated – Surcharged Policies Pre Existing Conditions
Jump to section on
|
How much does kidney dialysis cost?
How is it covered under the various options for Medicare Coverage?
How costly is kidney failure treatment?
Kidney failure treatment—hemodialysis, peritoneal dialysis, and kidney transplantation—is costly, and most people need financial help. The average cost to Medicare per person in 2011 was1
- almost $88,000 for hemodialysis, a treatment for kidney failure that filters blood outside the body
- more than $71,000 for peritoneal dialysis, a treatment for kidney failure that uses the lining of a person’s abdominal cavity as a filter
- almost $33,000 for a transplant, surgery to place a healthy kidney from someone who has just died or a living donor, usually a family member, into a person’s body nih.gov *
**********
Dialysis is used during end-stage kidney failure to replace the functions of the kidneys — including waste removal and regulation of blood levels of potassium and sodium.
Typical costs:
- Dialysis is covered by health insurance.
- For patients covered by health insurance, out-of-pocket costs typically include the deductible, and coinsurance for the treatment cost.
- For example, with Medicare, a patient, once the deductible of about $150 is met, typically would pay coinsurance of 20%; but many Medicare patients also have secondary insurance to cover all or part of that cost.
- A study published in Health Affairs[1] showed that the average U.S. patient pays $114 for dialysis-related drug costs and about $10 in dialysis costs per month. health.costhelper.com/dialysis.html *
New Rule to promote at-home dialysis services
- kidney.org/home hemo
- fresenius kidney care.com/home-hemodialysis
- home dialysis.org/home-dialysis-basics
- davita.com/can-anyone-do-dialysis-at-home
and transplant care for people from underserved communities —- decisive step to ensure people with Medicare with chronic kidney disease have easy access to quality care and convenient treatment options 42 CFR Parts 412, 413 and 512 Final Rule Modern Health Care *
New rule to promote at-home dialysis services and transplant care for people from underserved communities, which marks the agency’s first effort to tackle health disparities for Medicare enrollees with kidney failure in the decade since Congress established the prospective payment system for ESRD providers. CMS published the proposed rule for ESRD payments in July. .modernhealthcare.com/payment/medicare-drops-changes-esrd-payment-health-equity-mind
- See our page on what Medi Gap and Medicare Pay.
- View Typical Summary of Benefits for MAPD
- latimes.com/dialysis-industry-political-spending
- kevin md.com/involuntary-discharge-dialysis
- Dialysis Management Solutions (DMS) provides services to help self-funded employers and brokers manage the impact of dialysis claims and ease the stop-loss renewal process.
FAQ’s
- What about staying with under an under 65 plan? Covered CA?
- Covered CA – Co-Ordination with Medicare?
- Who gets on the list for a kidney?
- Are patients being forced into Medicare – Insurers making Dialysis clinics out of Network?
- Supreme Court sides with insurer in dialysis coverage case
- Supreme Court rules in favor of insurance plan that pushed kidney failure patient to Medicare
- The Supreme Court’s Dialysis Ruling Reinforces Self-funding as the Only Affordable Option
- Medicare expenditures could be reduced by increased peritoneal dialysis use
-
Medi-Gap policy?
Can you get or keep one?- If you have a Medi Gap plan before you are diagnosed with ESRD, you can keep it.
- There is also a guaranteed issue opportunity when you turn 65, Medicare Publication Kidney Dialysis & Transplant Services # 10128. page 42.
- If you get a Medicare Advantage plan, you could then change to Medi Gap under the 1 year free trial rule MAYBE!!!
- If this is your situation, ask us and we will double check. One must read the law 3 times and then when you think you understand it, read it again.
- One could also hope for a “Underwriting Holiday.”
- Anthem MediBlue Plus & SNP
- Blue Shield 65 Plus – Inspire HMO 2024
- Scan
- SNP Special Needs Plans Medicare Advantage
- United Health Care
- If you are not in a guaranteed issue period, here’s the underwriting questions, so forget it.
#Medicare10050 and You 2025
Spanish
Everything you want to know
- Steve's Video Seminar Introduction to Medicare & You
- 2025 Changes & Updates CA Health Care Advocates 78 page slide show pdf
- Clear View to Medicare Patient Advocate.org - 36 pages
***********
- Your Medicare #Benefits # 10116
- Inpatient ONLY - How Medicare Pays for your Surgery Part A vs Part B Very Well Health.com
- medicare.gov/coverage
- What's Covered App for Smartphones
- Medicare Coverage Database Search
- medicare.gov/procedure-price-lookup
- MLN Items & Services Not Covered Under Medicare
- An Overview-05-19-23 CA Health Care Advocates Hi Cap
- Original Medicare: An Overview CA Health Care Advocates Hi Cap
- 2024 Premiums, Coinsurance & Deductibles – 10-19-23 CA Health Care Advocates Hi Cap
- Supplementing Medicare: An Overview 10-30-20 CA Health Care Advocates Hi Cap
- Enroll in Blue Cross
- Learn about UHC United Health Care
- Enroll in Blue Shield
- SCAN
- Use our scheduler to Set a phone, Skype or Face to Face meeting
- #Intake Form - We can better prepare for the meeting (National Contracting Center)
- TITLE XVIII—HEALTH INSURANCE FOR THE AGED - Medicare AND DISABLE
-
- Welcome to Medicare 2022 Publication # 11095
- Our webpage on Enrolling ONLINE for Medicare Part A Hospital & B Doctor Visits
- Part A Hospital rules for zero premium
- Part B – Doctors – How to sign up – Benefits
- How to apply for Part B when you lose employer coverage - during your special enrollment period # 10012
- Fact Sheet Deciding Whether to Enroll in Medicare Part A and Part B When You Turn 65 CMS.gov 15 pages
- Medicare & You: Deciding to Sign Up for Medicare Part B VIDEO
- CMS form to fill out L 564 E to prove you had Employer Coverage and get a special enrollment period, when you retire. VIDEO
- HI CAP CA Health Care Advocates Medicare Enrollment Periods
FAQ's from Medicare.Gov
#Should I get Parts A & B?
Most people should enroll in Medicare Part A (Hospital Insurance) when they're first eligible, but certain people may choose to delay Medicare Part B (Medical Insurance). In most cases, #How
It depends on the type of health coverage you may have.
- Deciding to Sign Up for Medicare Part B VIDEO
- You must pay your Part B premium every month for as long as you have Part B (even if you don’t use it).
- If I'm low income - are there any breaks?
- Interactive Q & A from IRS on when to sign up for Medicare
- I have coverage through my spouse who is currently working.
- I have retiree coverage (from my former employer or my spouse’s former employer) or COBRA coverage.
- I have TRICARE, and I'm a retired service member.
- I have TRICARE, and I'm an active-duty service member.
- I have CHAMPVA.
- I have End-Stage Renal Disease (ESRD).
- I have Marketplace Covered CA or other private insurance.
- I don't have any of these.
- medicare.gov/should-i-get-parts-a-b
- How to apply for Part B during your special enrollment period # 10012
- Fact Sheet Deciding Whether to Enroll in Medicare Part A and Part B When You Turn 65 15 pages
- FAQ's that we did
Medicare Advantage Plans
Guaranteed Acceptance!
All Medicare Advantage plans will accept customers with ESRD! AHIP * Modern Health Care * 21st Century Cures Act
- Anthem MediBlue Plus
- United Health Care
- Blue Shield 65 Plus – Inspire HMO 2022
- SCAN
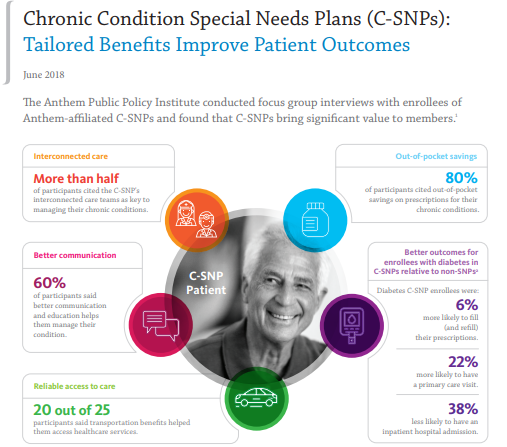
Medicare MAPD Special Needs #SNP
& Chronic Condition – C-SNP Plan?
Definition:
To enroll in a Medicare SNPs you must have one of these specific diseases or characteristics. Medicare SNPs tailor their benefits, provider choices, and drug formularies to best meet your specific needs. Medicare.gov
There are three different types of SNPs:
- Chronic Condition SNP (C-SNP)
- Dual Eligible SNP (D-SNP) Medicare & Medi Cal
- Institutional SNP (I-SNP) cms.govSpecialNeedsPlans *
Medicare SNPs CMS.gov also see Special Needs Plans are subtype of Medicare Advantage Plan.
- Can I get my health care from any doctor, other health care provider, or hospital?
- You generally must get your care and services from doctors, other health care providers, or hospitals in the plan’s network (except emergency care, out-of-area urgent care, or out-of-area dialysis).
- Prescription drugs
- Yes. All SNPs must provide Medicare prescription drug coverage (Part D).
- Do I need to choose a primary care doctor?
- Generally, yes.
- Do I have to get a referral to see a specialist?
- In most cases, yes. Certain services, like yearly screening mammograms, don’t require a referral.
- What else do I need to know about this type of plan?
- A plan must limit membership to these groups:
- 1) people who live in certain institutions (like nursing homes) or who require nursing care at home, or
- 2) people who are eligible for both Medicare and Medicaid, or
- 3) people who have specific chronic or disabling conditions (like diabetes, End-Stage Renal Disease, HIV/AIDS, chronic heart failure, or dementia).
- Check with us, there might be additional rules [email protected]
- A plan must limit membership to these groups:
- Plans will coordinate the services and providers you need to help you stay healthy and follow doctors’ or other health care providers’ orders.
- Scan Foundation Summary on Chronic Care Act
- Forbes *
- Social Services
- SNP plans may also offer home-delivered meals, transportation for nonmedical needs, pest control, indoor air quality equipment (e.g., air conditioner for someone with asthma), and minor home modifications (e.g., permanent ramps, widening of hallways or doorways to accommodate wheelchairs).
- Learn More
- Health IT.gov *
- Model of Care - HRA - Blue Shield Promise
- Telehealth *
- Modern Health Care *
- Oscar TeleHealth
- Medicare Managed Care Manual Chapter 16-B: Special Needs Plans
- cms.gov/Special-Need-Plans-SNP-Frequently-Asked-Questions-FAQ
- Taking Stock of Medicare Advantage: Special Needs Plans Commonwealth Fund
- Our webpage on
- Proposed Rule 2023 to lower out of pocket Medicare Part D prescription drug costs and improve consumer protections, reduce disparities, and improve health equity in Medicare Advantage (MA) and Part D. CMS.Gov Fact Sheet *
-
SNP enrollment is year around.
- Learn More
#Understanding Medicare Advantage Plans (PDF) #12026
- MAPD Plans look like a great deal, as the "premium" is paid by fee from the Federal Government, on average $2k/year.Kff * MAPD Plans must cover all A & B services Medicare.Gov * generally they also cover Part D Rx.
- That's why the premium is very low or ZERO!
- Set a Zoom Meeting
- We can now do SOC Scope of Appointment, before the Meeting via a 3 minute recorded meeting 2 days before. AHIP Training Module 4 Page 14 *
- #Intake Form Berwick Needs Assessment Form - We can better prepare for the meeting
- Medicare Advantage (Medicare Part C): An Overview Hi Cap
- HMO - Narrow Networks?
- HI Cap CA Health Care Advocates Fact Sheet
- Do I just sign up with a Medicare Advantage Company and automatically get * Parts A & B or do I have to get those from Medicare.Gov * VIDEO
- Get Quotes, Full Information and Enroll
- MANDATED wording!: Think Advisor * ‘‘We do not offer every plan available in your area. Any information we provide is limited to those plans we do offer in your area. Please contact Medicare.gov or 1–800–MEDICARE to get information on all of your options.’’
- We disagree with the above wording, as we can use the same tools on Medicare.gov as they do!
- FYI a 4.27.2022 HHS Office of the Inspector General report found that MAPD plans denied 13% of prior authorizations that would have been covered under original Medicare (Conversely, Medi Gap, just follows what Medicare pays.)
- 88% of MAPD enrollees are happy
-
MAPD plans often include Dental & Part D - Rx Prescriptions and often have NO premiums!
-
How is that possible?
-
The Federal Government pays them around $700/month to handle your medical care. You must continue to pay your Medicare Part B premium of about $170/month. It's best to apply when you turn 65 for the supplement plans or advantage plans, as that's the main "Open Enrollment" period, guaranteed issue for any plan.
-
-
-
Medicare Advantage Plans also have an annual open enrollment now known as AEP Annual Election Period October 7 to December 15th.
-
Additional Coverage is important as Medical Bills are increasing Seniors Credit Card Debt or leading to possible bankruptcy?
- If You Have Problems with Your Medicare Advantage Plan
- forbes.com/how-insurers-can-navigate-the-costs-of-medicare-advantage-benefits
- politico.com/medicare-advantage-plans-congress
- Uncle Sam wants you to help stop insurers' bogus Medicare Advantage sales tactics
- ca health advocates/using-ai-to-deny-care
- Dodging the Medicare Enrollment Deadline Can Be Costly
- Medicare Advantage Increasingly Popular With Seniors — But Not Hospitals and Doctors
- Medicare Advantage is bad for patients and bad for investors
- When Medicare Advantage Plans Terminate Coverage
- Medi-Cal D-SNP Feasibility Study
Medicare Advantage
Special Needs Plans
LIPITOR can cause serious side effects
These side effects have happened only to a small number of people. Your doctor can monitor you for them. These side effects usually go away if your dose is lowered or if LIPITOR is stopped. These serious side effects include:
- Muscle problems. LIPITOR can cause serious muscle problems that can lead to kidney problems, including kidney failure. You have a higher chance for muscle problems if you are taking certain other medicines with LIPITOR.
- Liver problems. Your doctor should do blood tests to check your liver before you start taking LIPITOR and if you have symptoms of liver problems while you take LIPITOR. Call your doctor right away if you have the following symptoms of liver problems:
-
- Feel tired or weak
- Loss of appetite
- Upper belly pain
- Dark, amber-colored urine
- Yellowing of your skin or the whites of your eyes
- Learn More===> lipitor.com/side-effects
People who take high doses of popular cholesterol-lowering drugs called statins may be more likely to develop kidney problems, a new study suggests.
“If you are concerned about your statin then go talk to your doctor,” he said. “Do not panic. There are both urine and blood tests your doctor can use to monitor your kidneys.”
Signs of kidney injury could include dark urine, difficulty urinating or less frequent urination. “If you are on a higher dose of a statin and there is any issue with urination, call your doctor,” Steinbaum said. “Instead of a high-dose statin, we can use a lower-dose statin along with another type of cholesterol-lowering medication.”
Whatever you do, Mehta added, “do not stop taking statins abruptly. Have a conversation with your doctor to discuss your benefits and risks, and ask if your kidney function has been tested.” Read the whole article==> Web MD
You cannot buy additional coverage through #Covered California
if you have premium-free Medicare Part A Hospital
Medicare complies with Health Care Reform, so you do NOT need to get a an Individual policy or a subsidized one from Covered CA. It fact, it's illegal for anyone to sell you a policy! Kaiser Health News * Covered CA Medicare Fact Sheet * Medicare.Gov Medicare & Market Place #11694 * CMS.Gov FAQ Medicare & Marketplace * HealthCare.Gov when - how to change from Covered CA to Medicare * Social Security §1882 * Health Care.Gov
NOTE: This information also applies to people younger than 65 whose benefits begin the first month they receive disability benefits because they have Amyotrophic Lateral Sclerosis (ALS), better known as Lou Gehrig’s Disease, and to people younger than 65 who have Medicare because of a disability and are receiving SSDI Social Security Disability Insurance.
There are a lot of ands, if or buts in this complex issue. Please refer to the source material below. There are some exceptions, but they are very complex. Don't even think of getting a 1/2 correct answer over the phone. If you have to pay for Part A Hospital, then are options, like subsided Covered CA Plans. Email us [email protected] or ask a question below.
Video about Covered CA – if no Premium Free Part A – jump to 2:30 Medicare & the Marketplace (Covered CA
Medicare vs Covered CA - Publication 11694
Links & Resources
- Medicare Publication # 11694 Medicare & Covered CA
- Covered CA Medicare Fact Sheet
- InsureMeKevin.com
(3)(A)
(i) It is unlawful for a person to sell or issue to an individual entitled [no premium] to benefits under part A or enrolled under part B of this title (including an individual electing a Medicare+Choice plan [MAPD] under section 1851)—
(I) a health insurance policy with knowledge that the policy duplicates health benefits to which the individual is otherwise entitled under this title or title XIX,
(II) in the case of an individual not electing a Medicare+Choice plan, [aka MAPD Medicare Advantage] a medicare supplemental policy with knowledge that the individual is entitled to benefits under another medicare supplemental policy or in the case of an individual electing a Medicare+Choice plan, a medicare supplemental policy with knowledge that the policy duplicates health benefits to which the individual is otherwise entitled under the Medicare+Choice plan or under another medicare supplemental policy, or
(III) a health insurance policy (other than a medicare supplemental policy) with knowledge that the policy duplicates health benefits to which the individual is otherwise entitled, other than benefits to which the individual is entitled under a requirement of State or Federal law.
(ii) Whoever violates clause (i) shall be fined under title 18, United States Code, or imprisoned not more than 5 years, or both, and, in addition to or in lieu of such a criminal penalty, is subject to a civil money penalty of not to exceed $25,000 (or $15,000 in the case of a person other than the issuer of the policy) for each such prohibited act. Sec. 1882. [42 U.S.C. 1395ss]
Our webpages that touch on this Issue:
Rx costs under Medicare?
Renal & Transplants
Part D Rx – Shop Plans Immunosuppressant Rx can run $5 to 13k You Tube *
LIS Extra Help
Rx coverage under Part B Medicare?
Oral End-Stage Renal Disease (ESRD) drugs: Medicare helps pay for some oral ESRD drugs if the same drug is available in injectable form and the drug is covered under the Part B ESRD benefit.
Transplant / immunosuppressive drugs. Medicare covers transplant drug therapy if Medicare helped pay for your organ transplant. Medicare won’t pay for any services or items, including transplant drugs, for patients who aren’t entitled to Medicare.
Part D may cover other transplant drugs that Part B doesn’t cover, even if Medicare didn’t pay for the transplant. If you have ESRD and Original Medicare, you may join a Medicare drug plan.
If you’re entitled to Medicare only because of ESRD, your Medicare coverage ends 36 months after the month of the transplant.
Medicare will pay for your transplant drugs with no time limit if you were already entitled to Medicare because of age or disability before you got ESRD or you became entitled to Medicare because of your age or disability after getting a transplant that was paid for by Medicare or private insurance that paid primary to your Medicare Part A (Hospital Insurance) coverage, in a Medicare-certified facility.
Your costs in Original Medicare
You pay 20% of the Medicare-approved amount for covered Part B prescription drugs that you get in a doctor’s office or pharmacy, and the Part B deductible applies. In a hospital outpatient setting, you pay a copayment of 20%. If your hospital is participating in a certain outpatient drug discount program (called “340B”), your copayment will be 20% of the lower price, with some exceptions. Doctors and pharmacies must accept assignment for Part B drugs, so you should never be asked to pay more than the coinsurance or copayment for the Part B drug itself.
If you get drugs that Part B doesn’t cover in a hospital outpatient setting, you pay 100% for the drugs, unless you have Part D or other prescription drug coverage. In that case, what you pay depends on whether your drug plan covers the drug, and whether the hospital is in your drug plan’s network. Contact your prescription drug plan to find out what you pay for drugs you get in a hospital outpatient setting that Part B doesn’t cover. Medicare.Gov * Provider Tips to get paid CMS.gov *
- ESRD – General Information
- Clinical Performance Measures (CPM) Project
- End-Stage Renal Disease (ESRD) Quality Improvement Initiative
- ESRD Network Organizations
- cms.gov/ESRD-Center
-
ESRD Info on Medicare Website
-
Medicare Info for Children with End Stage Renal Disease (ESRD) From CMS.Gov
From KidneyFund.org
- What causes kidney failure?
- Symptoms
- Treatment of kidney failure
- New to dialysis
- Adjusting to kidney failure
- Complications of kidney failure
- Disaster preparedness
- Kidney failure/ESRD diet
- california health line.org/dialysis-patients-panic-as-kidney fund no longer pays premium for private health plan
- Kidney fund may give wrong advise on Insurance Coverage for their benefit, not the consumers… LA Times
More Links
- Medicare Advantage
- Medi-Gap (Supplements) ♦
- davita.com Kidney Care Resource Web MD on Chronic Kidney Disease
- 42 U.S. Code § 1395rr – End stage renal disease program
- Medical Necessity
- Clinical Guidelines for transplant
- Kidney.org – Travel ♦
- Pre-X for International Travel Plans ♦
- Medicare Outside of USA Insbuy
- Get the FULL policy – evidence of coverage
- Federal Register Final Rule 1.1.2020



https://www.aarp.org/health/medicare-qa-tool/does-medicare-cover-nutrition-counseling.html
https://www.amwins.com/solutions/group-benefits/self-funded/dialysis-management-solutions
https://www.medicarerights.org/medicare-watch/2024/12/12/incremental-expansion-of-dental-coverage-in-medicare-continues-under-biden-administration
https://www.npr.org/sections/shots-health-news/2024/12/17/nx-s1-5203056/pig-kidney-transplant-gene-edited
https://healthjournalism.org/blog/2025/01/medicare-is-experimenting-with-how-it-pays-for-kidney-transplants/
If I have 12 to 15% kidney function when does ESRD start?
I haven’t started dialysis.
End-Stage Renal Disease (ESRD)—Permanent kidney failure that requires a regular course of dialysis or a kidney transplant.
You can get Medicare no matter how old you are if your kidneys no longer work, you need regular dialysis or have had a kidney transplant,
medicare.gov/Medicare-Coverage-ESRD
Having kidney failure means that:
85-90% of your kidney function is gone
your kidneys don’t work well enough to keep you alive
https://www.kidney.org/atoz/content/KidneyFailure
When the beneficiary first enrolls in Medicare based on ESRD, Medicare coverage usually starts:
1. On the fourth month of dialysis when the beneficiary participates in dialysis treatment in a dialysis facility.
2. Medicare coverage can start as early as the first month of dialysis if:
The beneficiary takes part in a home dialysis training program in a Medicare-approved training facility to learn how to do self-dialysis treatment at home;
The beneficiary begins home dialysis training before the third month of dialysis; and
The beneficiary expects to finish home dialysis training and give self-dialysis treatments.
Example: If the beneficiary starts home dialysis training in a Medicare approved facility, or if a course of home self-dialysis training is begun before the third month of dialysis, or if the beneficiary is expected to finish home dialysis training and perform self-dialysis on July 17th, the Medicare entitlement date would be July 1st.
3. Medicare coverage can start the month the beneficiary is admitted to a Medicare-approved hospital for kidney transplant or for health care services that are needed before the transplant if the transplant takes place in the same month or within the two following months.
Example: If the beneficiary has a kidney transplant on July 17th, the Medicare entitlement date would be July 1st.
4. Medicare coverage can start two months before the month of the transplant if the transplant is delayed more than two months after the beneficiary is admitted to the hospital for that transplant or for health care services that are needed before the transplant.
Example: If on July 17th the beneficiary starts pre-surgical health care services that are needed prior to a kidney transplant and the transplant is performed on September 4th, the Medicare eligibility date would be July 1st, since the transplant was performed within two months of the pre-surgical services.
5. Medicare coverage can start two months before the month of the transplant if the transplant is delayed more than two months after the beneficiary is admitted to the hospital for that transplant or for health care services that are needed before the transplant.
Example: The beneficiary was admitted to the hospital on May 25th for some tests that are needed before a kidney transplant. The transplant was to be on June 15th; however, the transplant was delayed until September 15th. Therefore, the beneficiary’s Medicare coverage will start on July 1st, two months before the month of transplant. cms.gov/End-Stage-Renal-Disease-ESRD
kidney.org/esrd_medicare_guidelines
Kidney failure refers to temporary or permanent damage to the kidneys that results in loss of normal kidney function. End-stage renal disease (ESRD) is when the kidneys permanently fail to work. stanford health care.org/medical-conditions/kidney-failure
Please contact an agent is your state ASAP!!! There are more options before you have ESRD!
If I have a transplant and I get better, do I lose my Medicare?
If so, can I get a “Special Enrollment” back into an ACA/Obamacare plan?
If you have Medicare only because of permanent kidney failure, Medicare coverage will end:
12 months after the month you stop dialysis treatments.
36 months after the month you have a kidney transplant.
Your Medicare coverage will resume if:
You start dialysis again, or you get a kidney transplant within 12 months after the month you stopped getting dialysis.
You start dialysis or get another kidney transplant within 36 months after the month you get a kidney transplant. medicare.gov/end-stage-renal-disease-esrd
If you lose Medicare, that would give you a special enrollment as it’s loss of MEC – Minimum Essential Coverage https://individuals.healthreformquotes.com/aca/enrollment/special/
Moral Issues on kidney transplant donors?
usa today.com/china-genocide-organ-trafficking
I’m getting a Kidney transplant. When does Medicare start?
If you’re getting a kidney transplant
Medicare coverage can begin the month you’re admitted to a Medicare-certified hospital for a kidney transplant (or for health care services that you need before your transplant) if your transplant takes place in that same month or within the next 2 months.
Example: Mr. Green will be admitted to the hospital on March 11 for his kidney transplant. His Medicare coverage will begin in March. If his transplant is delayed until April or May, his Medicare coverage will still begin in March.
If your transplant is delayed more than 2 months after you’re admitted to the hospital (for the transplant or for health care services you need before your transplant), Medicare coverage can begin 2 months before your transplant.
Example: Mrs. Perkins was admitted to the hospital on May 25 for some tests she needed before her kidney transplant. She was supposed to get her transplant on June 15. However, her transplant was delayed until September 17. Therefore, Mrs. Perkins’ Medicare coverage will start in July—2 months before the month of her transplant. medicare.gov/Medicare-Coverage-ESRD page 10
See page 9 if you want to qualify based on getting dialysis
Can a Marketplace plan [Covered CA] coordinate benefits with Medicare if the services rendered are dialysis when the member becomes eligible for Medicare because of their ESRD status?
If one were to already have a Covered CA plan, I guess it would be OK to keep it. There would NOT be any subsidies though. Learn More ===> HealthCare.Gov
If you don’t already have a Covered CA plan, then it’s illegal for anyone to sell you one. Citations: Khn.org Health Care.Gov
View Medicare Publication 2179 for details of how Medicare co-ordinates with other health insurance.
See our webpage on getting ACA under 65 plan vs Medicare