Introduction
Medicare & Employer Health Plans?
If you are covered by an Employer Group Health Plan Health Care Advocates Definition, then when you or your spouse turn 65 and become eligible for Medicare Part A Hospital and Part B Dr. Visits, there are several things to look into, check out and make decisions on:
- Does your employer’s health insurance plan have more or less than 20 employees?
- If fewer than 20, you MUST sign up for Medicare A & B as Medicare is Primary which means Medicare pays any bills first and if they don’t pay in full, then other coverage you might have, like your Employers Group health plan would pay. This may also mean, if you don’t have Medicare, you don’t get your bills paid! You must enroll in Medicare when you are supposed to, if not, there are penalties!
- Medicare rights.org/Medicare-and-Current-Employer-Insurance-Scenario
- Supplementing Medicare: Retiree Plans 04-06-21 Hi Cap
- Coverage While You and Your Spouse Work 04-06-21 Hi Cap
- Don’t just take our summary. Medicare’s rules are very complex and confusing. The rules are not ours, they are Medicare’s, CA State, Insurance Company etc.
- Follow the links, official brochures and footnotes below for the exact forms and citations you need. There are penalties if things are done even just a tiny bit wrong.
Try turning your phone sideways to see the graphs & pdf's?
Health Insurance unfortunately is very complicated
President Trump February 27, 2017
- Thus, if we haven't simplified and explained in PLAIN ENGLISH what you are looking for:
Does your employer have more or less than 20 Employees?
If your Employer Group Insurance has
#Fewer than 20 employees
.
If you work for an employer who has fewer than 20 employees, Medicare will be primary and pays before your other coverage. You MUST sign up for Part A and Part B * when you’re first eligible.
- There may also be Part A penalties if you have to pay a premium because you don’t qualify for Premium Free Part A along with having to wait to get your coverage.
- For more information see the Special Enrollment Periods) for when you lose Group Coverage!
- FAQ’s on should you enroll from Medicare.gov
- medicare.gov/working-past-65
- Medicare-Eligible Employees Pose HR Challenges SHRM
- Branden Benefits.com
-
We have seen a situation where the employee did not enroll in Medicare Part B thinking he had coverage through his company’s health insurance. A major medical event occurred and the health insurance company did not cover medical expenses that should have been covered by Medicare Part A & B. This left the employee with a large financial exposure.
The employer had been misinformed by the group health insurance agent who was not aware of the Medicare Part B requirement for companies with less than 20 employees.
-
- ca health advocates.org/other-health-insurance/employer-coverage
- medicare rights.org/Medicare-and-Current-Employer-Insurance-Scenario
- SCROLL DOWN for more information and details!
Just Turning 65? Less than 20 Employees
Enroll 1st in Medicare Parts A Hospital and B Dr. Visits
Then we can help you with Medi Gap, Part D Rx or Medicare Advantage
FAQ
Staying on Employer Plan
- I turned 65 a few months ago, I’m still working and I’ve stayed on my employers group plan.
- 1. If I cancel my current medical insurance, with my employer, then I guess I would need to sign up for Medicare part “B”, right?
- 2. My income probably falls into the first tier so there would be a premium of $134 +/-
- 3. Then I would need a Medicare Supplemental plan like my High Deductible F so another premium of $75 or so, right?
- 4. Then another supplemental Prescription Plan Part D with a premium of around $40
- 5. Also, my Granddaughter, whom I have legal custody of is on my group plan, so I would need to get individual coverage for her, right?
- 6. I believe that was around $350 for a plan I liked.
- 7. So I would end up with an estimated monthly expense of: Part B Medicare $134 Plan Hi F Medi Gap $75 Part D Rx $40 Individual Plan for Grand daughter $350 For a total of $599
- 8. On Medicare Part “B” how would she pay that premium? A. Monthly bank withdrawal?
- Answer
- 1. Yes
- 2. Correct. Here’s our page for Part B Premiums and the Surcharge on Part D
- Medi-Gap High F with Blue Shield is explained on our webpage here. Here’s the Plan Details and comparison of what Medicare Pays, what you pay and what the Insurance Company pays.
- Part D is explained in general on this page. Right now, AARP has the lowest premiums for Part D of the companies that we represent. However, AARP wants to control the Internet and doesn’t allow agents to post anything meaningful, as I hear everytime I go to a Web Design Meetup or anything, CONTENT IS KING! So, you have to email us to get AARP details. [email protected]
- 5 & 6. Coverage for dependents. You can get quotes here. We need to clarify on a case by case basis as to if an employer plan will cover dependents when the employee is covered by Medicare. In general, they will.
- 7 Yes, your calculations are correct. $350 for a young child gets you a platinum plan with Blue Shield.
- 8. Ways to pay Part B Medicare Dr. Visits are in the Medicare & You manual page 27 & 28
Medicare vs employer group when there are
#more than 20 employees
- If you have group health coverage based on your current employment (does NOT include COBRA!) you may be able to delay Part A and Part B and won’t have to pay a lifetime late enrollment penalty if you enroll later.
- Verify with your HR or benefits manager that you have minimum essential group health plan coverage as defined under 26 U.S. Code § 5000
- See Our webpage on the Employer Tax Deduction Section 106 for the premiums paid into a Group Health Plan.
- When you retire and decide to go on Medicare, Medi Gap, Part D Rx, etc., will your employer be able to certify on form L564 E OMB No. 0938-0787 that you had qualifying Group Health Coverage. If your employer won’t or can’t fill out this form, what about your 1095 B Conformation of Employer Minimum Essential Coverage?
- Insurance ID Cards? Pay Stubs?
How you delay your Medicare coverage depends on your situation:
- If you’ll be getting benefits from Social Security or the Railroad Retirement Board (RRB) at least 4 months before you turn 65, you’ll automatically get Part A and Part B. You’ll get your red, white, and blue Medicare card in the mail 3 months before your 65th birthday.
- If you don’t want Part B, follow the instructions that came with the card. If you keep the card, you keep Part B and will pay Part B premiums.
- If you won’t be getting benefits from Social Security or the Railroad Retirement Board (RRB) at least 4 months before you turn 65, you don’t need to do anything when you turn 65.
- It’s illegal for an employer to offer any incentives to encourage you to take Medicare and drop the employer plan! Coremarkins * The Age Discrimination in Employment Act (ADEA) prohibits employers with 20 or more employees from cancelling group health coverage for current employees due to age, even when such employees become eligible for Medicare. SHRM *
Links, Resources & Bibliography
- Interactive Q & A from IRS on when to sign up for Medicare
- Centers for Medicare & Medicaid Services employer web page
- Fact Sheet: Medicare decisions for someone nearing age 65
- Fact Sheet: Deciding whether to enroll in Medicare Part A or Part B when you turn 65
- Fact Sheet: Medicare Decisions for Those Over 65 and Planning to Retire in the Next 6 Months
- See our module in the upper right on Should I get A & B?
FAQ’s
#Important
Let your Employer know you’re eligible for Medicare A & B
You must tell your employer if you are enrolled, or eligible to enroll, in Medicare (Part A and/or Part B coverage). Your boss is mandated to tell Medicare who is working there and is eligible for Medicare.
- cms.gov/Mandatory-Insurer-Reporting-For-Group-Health-Plans
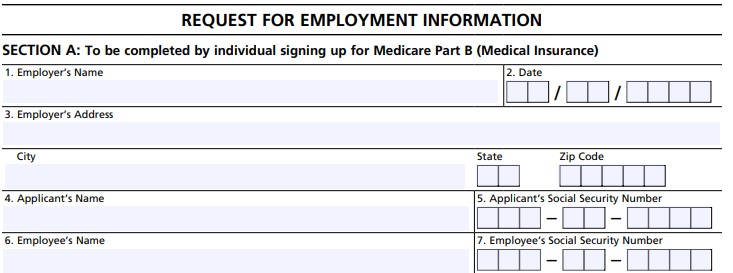
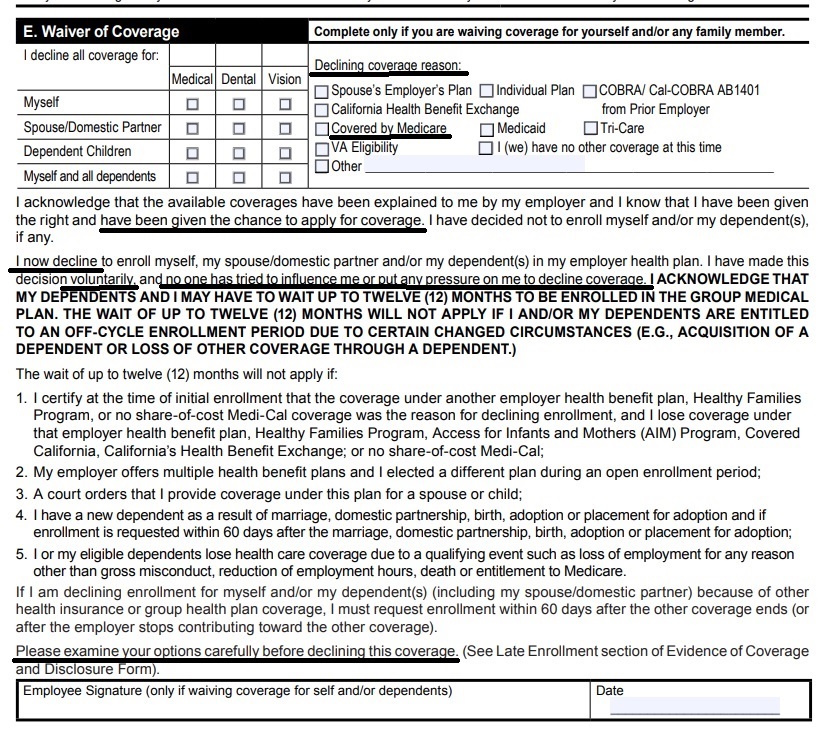
- Employee Enrollment Application – waiver form
FAQ
- If an employee goes onto Medicare, can his #dependents stay on the group Plan?
- Yes, for dependent to be covered, the term is ELIGIBLE employee, not enrolled employee
- I got a client an $18k REFUND by doing this!
- Employer Dependent Definition
- Blue Cross Group Administrator Manual
- See waiver of coverage above, just decline for the employee due to Medicare. Don’t decline for the dependents!
- Yes, for dependent to be covered, the term is ELIGIBLE employee, not enrolled employee
General Information on
- Medicare A Hospital
- Medicare B Dr. Visits
#Medicare10050 and You 2025
Spanish
Everything you want to know
- Steve's Video Seminar Introduction to Medicare & You
- 2025 Changes & Updates CA Health Care Advocates 78 page slide show pdf
- Clear View to Medicare Patient Advocate.org - 36 pages
***********
- Your Medicare #Benefits # 10116
- Inpatient ONLY - How Medicare Pays for your Surgery Part A vs Part B Very Well Health.com
- medicare.gov/coverage
- What's Covered App for Smartphones
- Medicare Coverage Database Search
- medicare.gov/procedure-price-lookup
- MLN Items & Services Not Covered Under Medicare
- An Overview-05-19-23 CA Health Care Advocates Hi Cap
- Original Medicare: An Overview CA Health Care Advocates Hi Cap
- 2024 Premiums, Coinsurance & Deductibles – 10-19-23 CA Health Care Advocates Hi Cap
- Supplementing Medicare: An Overview 10-30-20 CA Health Care Advocates Hi Cap
- Enroll in Blue Cross
- Learn about UHC United Health Care
- Enroll in Blue Shield
- SCAN
- Use our scheduler to Set a phone, Skype or Face to Face meeting
- #Intake Form - We can better prepare for the meeting (National Contracting Center)
- TITLE XVIII—HEALTH INSURANCE FOR THE AGED - Medicare AND DISABLE
-
- Welcome to Medicare 2022 Publication # 11095
- Our webpage on Enrolling ONLINE for Medicare Part A Hospital & B Doctor Visits
- Part A Hospital rules for zero premium
- Part B – Doctors – How to sign up – Benefits
- How to apply for Part B when you lose employer coverage - during your special enrollment period # 10012
- Fact Sheet Deciding Whether to Enroll in Medicare Part A and Part B When You Turn 65 CMS.gov 15 pages
- Medicare & You: Deciding to Sign Up for Medicare Part B VIDEO
- CMS form to fill out L 564 E to prove you had Employer Coverage and get a special enrollment period, when you retire. VIDEO
- HI CAP CA Health Care Advocates Medicare Enrollment Periods
FAQ's from Medicare.Gov
#Should I get Parts A & B?
Most people should enroll in Medicare Part A (Hospital Insurance) when they're first eligible, but certain people may choose to delay Medicare Part B (Medical Insurance). In most cases, #How
It depends on the type of health coverage you may have.
- Deciding to Sign Up for Medicare Part B VIDEO
- You must pay your Part B premium every month for as long as you have Part B (even if you don’t use it).
- If I'm low income - are there any breaks?
- Interactive Q & A from IRS on when to sign up for Medicare
- I have coverage through my spouse who is currently working.
- I have retiree coverage (from my former employer or my spouse’s former employer) or COBRA coverage.
- I have TRICARE, and I'm a retired service member.
- I have TRICARE, and I'm an active-duty service member.
- I have CHAMPVA.
- I have End-Stage Renal Disease (ESRD).
- I have Marketplace Covered CA or other private insurance.
- I don't have any of these.
- medicare.gov/should-i-get-parts-a-b
- How to apply for Part B during your special enrollment period # 10012
- Fact Sheet Deciding Whether to Enroll in Medicare Part A and Part B When You Turn 65 15 pages
- FAQ's that we did
Medicare #DualCoverage
Publication - 02179
-
VIDEO how two plans coordinate and pay your claim.
- Medicare.Gov on how Medicare works with other insurance.
- Employer obligation to report # of employees to Medicare
- Explanation from Cal Broker Magazine Sept 2019
- Sample Small Employer Group Health Plan
#Subrogation
Medicare's Right to collect from other Coverage
- You're Medicare Advantage plan has the right and responsibility to collect - subrogate for covered Medicare services for which Medicare is not the primary payer.
- According to CMS regulations at 42 CFR sections 422.108 and 423.462, Anthem MediBlue Access (PPO), as a Medicare Advantage organization, will exercise the same rights of recovery that the Secretary exercises under CMS regulations in subparts B through D of part 411 of 42 CFR and the rules established in this section supersede any state laws. Anthem MediBlue Access (PPO) Evidence of Coverage
- Medi-Cal (for People with Medicare) – 04-19-23 Hi Cap CA Health Care Advocates
Medicare Part A
(#Hospital Insurance)
Medicare Part A Hospital coverage helps pay for care in hospitals as an inpatient,... skilled nursing facilities, hospice care, and some home health care (see publication # 10969) but not Long Term Care.
Most people get Part A automatically when they turn age 65 at no charge, since they or a spouse paid Medicare taxes while they were working. You need to sign up close to your 65th birthday, even if you will not be retired by that time. (If you are getting Social Security benefits when you turn 65, your Medicare Hospital Benefits - Part A - start automatically.)
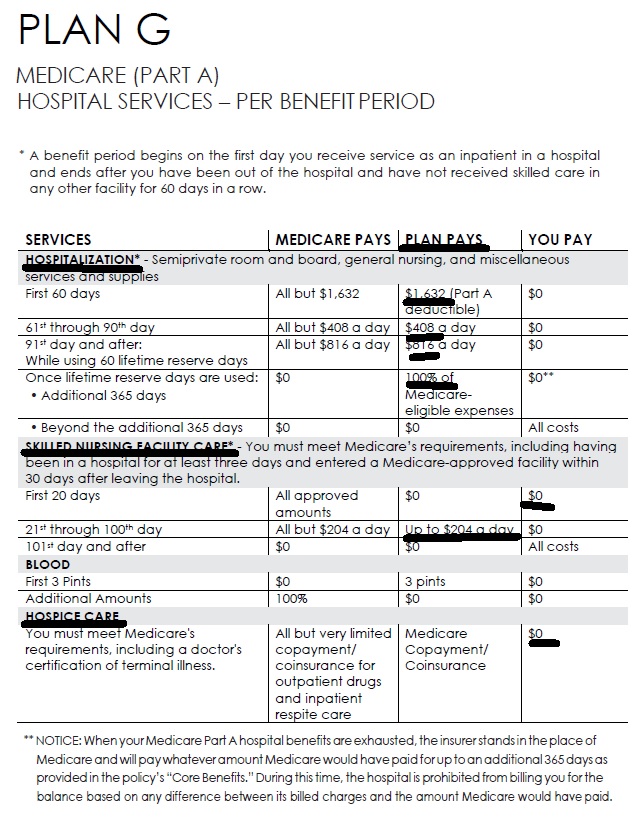
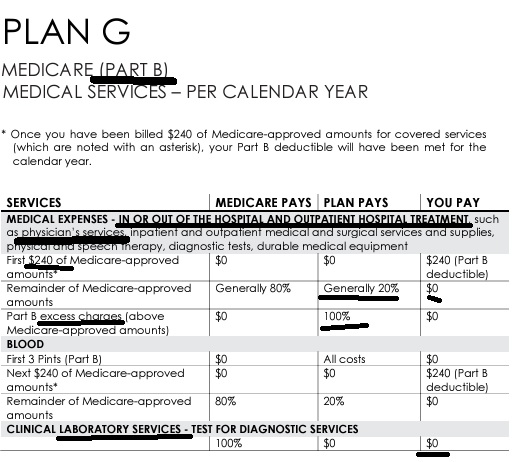
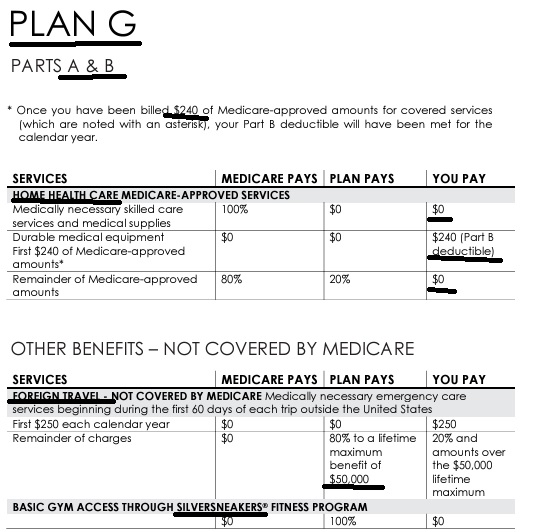
Here's a chart it's just a illustration and is NOT official that shows what Medicare pays, the gaps in Medicare and what you may get when you add a Medi Gap Plan or Medicare Advantage to cover those gaps
.Steve's VIDEO Explanation Comparing what Medicare pays and what you get extra with MAPD or Medi Gap
-
See full brochure I cut and pasted this from
-
Pays on top of Medicare Parts A & B – Any Medicare Provider
Part B - Outpatient helps Pay For Doctors' services, outpatient hospital care, and some other medical services that Part A does not cover, such as the services of physical and occupational therapists, and some home health care see publication 10969, but not Long Term Care. Part B helps pay for these covered services and supplies when they are medically necessary.
The chart below is a very brief summary. Check the actual Evidence of Coverage for the plan you want to enroll in, Medicare & You or actual Medicare documents.
2024 Fact Sheet Medicare Costs
Our Webpages with more detail:
- Coverage in Part A Hospital & B Doctor Visits? Part D Rx
- Chiropractic – Medicare A & B – MAPD
- Diabetes – Prevention & Coverage under Medicare & ACA
- Durable Medical Equipment
- End Stage Renal – Kidney Failure
- Hearing Aids
- Physical therapy – occupational speech
- Skilled Nursing SNF & Home Health What Medicare Pays
- Togetherness – Loneliness Social Determinants of Health
- Mental Health
- How to sign up for Medicare?
- FAQ Medical Necessity our Medical Necessity Webpage
- Original Medicare & Medi-Gap – Supplement vs Medicare Advantage MAPD
- Medicare Beneficiaries’ Out-of-Pocket Spending for Health Care AARP
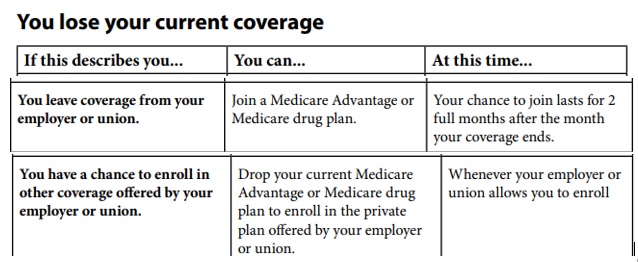
Special Enrollment Periods SEP
When you lose Employer Coverage
Special Enrollment Period SEP for Medicare Parts A & B
When you #lose or give up Group Health Coverage
Watch for the Deadlines!
When you retire, decide you don’t want or lose your employer coverage (COBRA doesn’t count! CA Health Care Advocates) you may then have an SEP Special Enrollment Period to enroll in Part B Doctor visits, without penalty.
- Special enrollment period Social Security Publication # 10012
- You can use an SEP to enroll in Medicare Part B while you’re still in a group health plan based on current employment. Also, if your employment ends or employer-provided medical coverage ends
- If you already have Part A Hospital, you can enroll online, or fill out the
- #application for Part B OMB No. 0938-1230 ! and the
- Certification from your Employer that you had Group Coverage OMB No. 0938-0787 – L564 E
- If the employer can’t fill it out, complete Section B of the form as best you can, but don’t sign it.
- You’ll need to submit proof of job-based health insurance.
- What forms of proof can I send?
- Income tax form that shows health insurance premiums paid
- W-2s showing pre-tax medical contributions
- Pay stubs showing health insurance premium deductions
- Health insurance cards with a policy effective date
- Explanations of benefits paid by the employer group health plan
- Statements or receipts that show payment of health insurance premiums
- You can apply online (at Social Security) – select “Already Enrolled in Medicare” from the menu.
- Or, fax or mail your forms to your local Social Security office. Medicare.gov *
- If the employer can’t fill it out, complete Section B of the form as best you can, but don’t sign it.
- This Special Enrollment Period also doesn’t apply if you have one of these:
- ■ End-Stage Renal Disease (ESRD)
- ■ Veterans Affairs and
- Individual Health Insurance Marketplace – Covered CA 11036-Enrolling-Medicare-Part-A-Part-B.pdf page 13
Introduction to #MediGap
Our video explaining the Governments brochure on choosing a Medi Gap Policy. Click the little square on the right, to enlarge the video.
- 2025 Official Medicare Guide to choosing a Medi Gap Policy # 02110
- Spanish
- Get Quotes for Medi Gap Quotit
- Medicare Supplement Policies CA Insurance Code §§10192.1 - 10192.24
- CA Health Care Advocates HI CAP Fact Sheet
- If you have a Medigap policy and get care, Medicare will pay its share of the Medicare-approved amount for covered health care costs. In most Medigap policies, you agree to have the Medigap insurance company get your Part B claim information directly from Medicare. Then, your Medigap policy will pay your doctor whatever amount you owe under your policy and you’re responsible for any costs that are left. Learn More >>> Medicare.Gov
- Prior Authorization NOT Required! Askchapter.org *
- Supplementing Medicare: An Overview 10-30-20 Hi Cap
- Supplementing Medicare: Medigap Plans 12-14-23 Hi Cap
- Your Rights to Purchase a Medigap 12-14-23 HI Cap
- Search for Participating Doctors & Hospitals - Just about ALL of them!
- Anthem Blue Cross Information & Enrollment
- United Health Care
- Blue Shield – Medi-Gap Information & Enrollment
- Health Net
-
Medi Gap pays the medical expenses that Original Medicare Part A (Hospital) and Part B (Doctor) doesn't. Check out the chart on this page to see what Medicare Pays, what you pay and what a Medi Gap plan pays.
- If you have a Medigap policy and get care, Medicare will pay its share of the Medicare-approved amount for covered health care costs. Then, your Medi-gap policy will pay its share. You’re responsible for any costs that are left. Medicare.Gov *
- More than half of all fee-for-service Medicare enrollees without any additional coverage chose a Medicare Supplement plan in 2021 Health Care Finance *
-
Original Medicare, Medicare Advantage nor Medi Gap pay for long term care either in a nursing home or at home care. Get more information on Long Term Care here.
-
Even if you think you can't afford any extra premiums, there's a lot of valuable information to help with planning.
-
When you enroll in Medi Gap beyond age 65 for Part B as you had
Qualifying #Employer Coverage
Termination of Employment or Retirement Plan
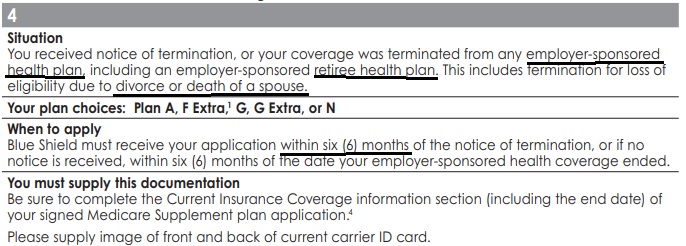
You have the right to purchase a Medi-gap policy for 6 months if your, your spouse’s or a family member’s current employment or retirement plan coverage terminates, or you lose your eligibility due to divorce or death of a spouse or family member.
The 6-month period to apply for a Medigap policy starts on the date you receive notice that your health benefits will end. If you do not receive advance notice, the 6-month period starts the date the benefits end or the date of your first denied claim. This protection of California law applies whether your group health benefits were primary or secondary to Medicare.
Our webpage on the pros & cons of Employer Coverage vs Medicare
Loss of COBRA or Cal Cobra
You are also entitled to this protection when you become eligible for COBRA (Our webpage on COBRA) or have used up all your COBRA benefits. It does not apply if you stop paying COBRA premiums before you use all your benefits. COBRA benefits are always secondary to Medicare benefits unless you have ESRD Renal Kidney Failure and are in a 30-month coordination period. For more information on COBRA, see Medicare & Other Health Insurance. CA HealthCare Advocates *
COBRA and Medicare are VERY VERY confusing. Double check with us [email protected] on your specific situation!!!
Situation 4 From Medi Gap Guaranteed Issue Guide
You received notice of termination, or your coverage was terminated from any employer-sponsored health plan, including an employer-sponsored retiree health plan. This includes termination for loss of eligibility due to divorce or death of a spouse.
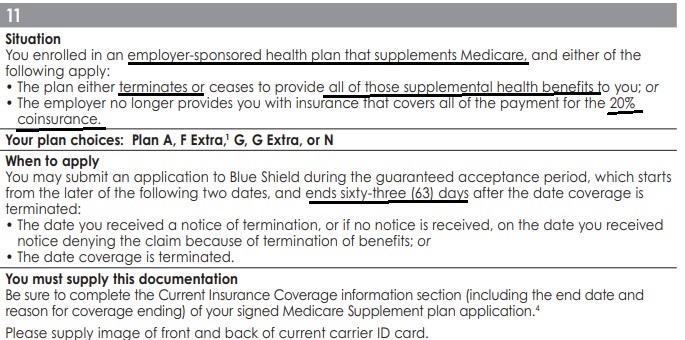
Situation 11 from Medi Gap Guaranteed Issue Guide
- You enrolled in an employer-sponsored health plan that supplements Medicare, §419 (e) Welfare Benefit Plans and either of the following apply:
- The plan either terminates or ceases to provide all of those supplemental health benefits to you; or
- The employer no longer provides you with insurance that covers all of the payment for the 20% coinsurance.
- Why is there Both situation 4 and 11?
- I asked and was told # 11 applies to §419 (e) Welfare Benefit Plans
- Learn More about not enrolling in Part B if you have employer coverage
- See our main page on loss of employer coverage
MAPD Medicare Advantage &
Part D Rx
#Understanding Medicare Advantage Plans (PDF) #12026
- MAPD Plans look like a great deal, as the "premium" is paid by fee from the Federal Government, on average $2k/year.Kff * MAPD Plans must cover all A & B services Medicare.Gov * generally they also cover Part D Rx.
- That's why the premium is very low or ZERO!
- Set a Zoom Meeting
- We can now do SOC Scope of Appointment, before the Meeting via a 3 minute recorded meeting 2 days before. AHIP Training Module 4 Page 14 *
- #Intake Form Berwick Needs Assessment Form - We can better prepare for the meeting
- Medicare Advantage (Medicare Part C): An Overview Hi Cap
- HMO - Narrow Networks?
- HI Cap CA Health Care Advocates Fact Sheet
- Do I just sign up with a Medicare Advantage Company and automatically get * Parts A & B or do I have to get those from Medicare.Gov * VIDEO
- Get Quotes, Full Information and Enroll
- MANDATED wording!: Think Advisor * ‘‘We do not offer every plan available in your area. Any information we provide is limited to those plans we do offer in your area. Please contact Medicare.gov or 1–800–MEDICARE to get information on all of your options.’’
- We disagree with the above wording, as we can use the same tools on Medicare.gov as they do!
- FYI a 4.27.2022 HHS Office of the Inspector General report found that MAPD plans denied 13% of prior authorizations that would have been covered under original Medicare (Conversely, Medi Gap, just follows what Medicare pays.)
- 88% of MAPD enrollees are happy
-
MAPD plans often include Dental & Part D - Rx Prescriptions and often have NO premiums!
-
How is that possible?
-
The Federal Government pays them around $700/month to handle your medical care. You must continue to pay your Medicare Part B premium of about $170/month. It's best to apply when you turn 65 for the supplement plans or advantage plans, as that's the main "Open Enrollment" period, guaranteed issue for any plan.
-
-
-
Medicare Advantage Plans also have an annual open enrollment now known as AEP Annual Election Period October 7 to December 15th.
-
Additional Coverage is important as Medical Bills are increasing Seniors Credit Card Debt or leading to possible bankruptcy?
- If You Have Problems with Your Medicare Advantage Plan
- forbes.com/how-insurers-can-navigate-the-costs-of-medicare-advantage-benefits
- politico.com/medicare-advantage-plans-congress
- Uncle Sam wants you to help stop insurers' bogus Medicare Advantage sales tactics
- ca health advocates/using-ai-to-deny-care
- Dodging the Medicare Enrollment Deadline Can Be Costly
- Medicare Advantage Increasingly Popular With Seniors — But Not Hospitals and Doctors
- Medicare Advantage is bad for patients and bad for investors
- When Medicare Advantage Plans Terminate Coverage
- Medi-Cal D-SNP Feasibility Study
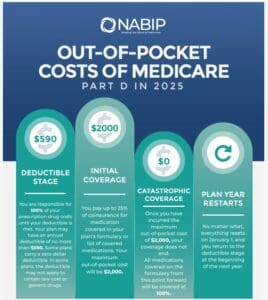
Prescription Drug 2025 #RxGuide
PDF # 11109
*****************
Coverage Gap - Donut Hole $2,000 Cap
******************
- Medicare Part D Rx generally runs say $30 to $100. See link below for how to shop premiums.
- Scope of appointment - permission to discuss Rx and MAPD Plans
- Our Webpage Premiums for those with High Income Parts D Rx & B Doctor Visits
- Medicare Rules for High Income People Medicare Costs # 11579
- Our #High Income Surcharge Video Explanation
- Ways to pay your premium - See brochure above.
- Kaiser Foundation Introduction - Overview
- Fact Sheet Medicare Part D CA Health Care Advocates Hi Cap
-
. Prescription Drugs Hi Cap
- Medicare Part D: An Overview – 10-31-23
- Prescription Drug Resources – 11-07-22
- When Your Part D Prescription is Denied– 11-22-22
- Medicare Rx Benefit Manual Rev 1.2016 83 pages
- Resources: Medicare Drug Coverage (Part D) Mini-Course & Podcast Series CMS
- Network Pharmacies, Formularies & Common Coverage Rules # 11136
- Insulin Maximum Co Pay $35
- Graphic on Part D Premium Increases & Why?
- Maximus Appeals LEP Late Enrollment Penalty
- Shop & Compare Tools Part D Rx
- Get Instant Quotes, Information & Enroll online
- MANDATED wording!: ‘‘We do not offer every plan available in your area. Any information we provide is limited to those plans we do offer in your area. Please contact Medicare.gov or 1–800–MEDICARE to get information on all of your options.’’ § 422.2267(e)(41).
- We disagree with the above wording, as we can use the same tools on Medicare.gov as they do!
Medicare Advantage Guaranteed Issue
When you lose Employer Coverage
Our webpage on Guaranteed Issue & Enrollment Periods for MAPD Medicare Advantage & Part D Rx
Just Enter your census or securely send us an excel spreadsheet or a list of employees and get instant proposals for California
FAQ’s
- I’ve retired early, I’m not 65 yet What do I do for Health – Medical Insurance?
- ***There are plenty of Health Plans in the Individual Market. Get quotes here. If your MAGI income is below 400% of Federal Poverty Level you may even qualify for subsidies – tax credits. Get a complementary quote, benefits, rates & subsidy calculation for California here. If you are 62+ and getting Social Security some of your Social Security is taxable and counts towards MAGI income for subsidies. If you are disabled, you get Medicare after two years of SSDI. If you can really live on a budget or are unfortunately forced to, there is Medi-Cal if you are under 138% of Federal Poverty Level. We don’t get paid to help you with that, so just contact Medi-Cal directly. Check out the Retirement Section of our website.
- I retired from North Carolina State University july 2018. They told me that they would supplement my medicare to the same level of medical insurance I had before, but when I asked them how to enroll for that they were less than helpful. I have social security and they pay a monthly premium I don’t know whether I am enrolled or what to do to enroll or what exactly I am covered for or what to do.
- Check out these websites to learn more about what your employer offers:
- Are Medigap policies written during the 8-month Special Enrollment Period issued subject to the same terms as terms, with regard to pre-existing conditions, as those written during the Initial Enrollment Period?
- ***We will answer your question on our Medi Gap Guaranteed Issue page.
- How do I show Medicare that I had qualifying employer coverage?
- See above under SEP Special Enrollment when you lose Group Coverage
- What Happens If I Don’t Take Part B as Soon as I’m Eligible?
- ***If you do not enroll in Medicare Part B during your initial enrollment period, you must wait for the general enrollment period (January 1- March 31 of each year) to enroll, and Part B coverage will begin the following July 1 of that year. If you wait 12 months or more, after first becoming eligible, your Part B premium will go up 10 percent for each 12 months that you could have had Part B but didn’t take it. You will pay the extra 10 percent for as long as you have Part B.
- If you didn’t take Part B at age 65 because you were covered under as an active employee (or you were covered under your spouse’s group health insurance plan and he/she was an active employee), you may sign up for Part B (generally without an increased premium) within 8 months from the time you or your spouse stop working or are no longer covered by the group plan. You also can sign up at any time while you are covered by the group plan. opm.gov/medicare-part-b-coverage/
- This is a wonderful service you’re providing and I will be sure to refer my friends to you for their insurance needs.
- ***Thank you
- I’m disabled and covered under my Dad’s retirement plan. I just qualified for Medicare. Must I enroll in Part B or can that be postponed as I have employer coverage?
- What about? Medi Cal? Aged & Disabled Program? Are there programs to pay the Part B Doctor Visits and Part D Rx.
- Yes, disabled people can be covered under their parents coverage
- Check these links:
- Medicare Part B Forgiveness
- ca.db101.org/medicare/program
- Aged and Disabled Federal Poverty Level Program
- Dual Coverage? Medi Cal, Employer Group, Individual, Cal Medi Connect & Medicare.
- FAQ on Medicare.gov
Anthem Medicare Supplement - Get Quotes, Information and ONLINE Enrollment - No extra charge for our help
Links, References & Resources
official Medicare link to enroll in Medicare Part A Hospitalization and Part B Doctor Visits.
Learn More ===>
- Medicare.gov – should I get part B?
- Publication 11036 Enrolling in Parts A & B and
- Medicare & You #10050
- Can you postpone Part A enrollment if you are covered under a Employer Group Plan?
- Early Retirement – What Health Insurance?
- Transitioning from Employer Group Coverage to Medicare
- Dual Coverage?
- the horses mouth on if you should get Part B Doctor Visits, how to enroll, COBRA Traps, etc.
- Medicare Eligibility & Premium Calculator Tool
- Part B Late Enrollment Penalty
- PBS News Hour FAQ’s Employer vs Medicare







I misunderstood and did not file for Medicare part B in time when I retired in June.
Now Kaiser has terminated my health care retirement benefit. I am enrolling now. [In Part B]
What options do I have or have I lost retirement health care through Kaiser forever?
If you lost Employer coverage in June you’re GOOD!
You have eight months to enroll in Part B! Medicare Publication 10012
If you have Part A Hospital then you need to use form OMB # 0938-1230 to enroll.
I presume your Kaiser is through your former employer. Check their website and rules. For example, here’s our webpage on LAUSD retirement…
As soon as you are approved for Part B, you should be able to get your Kaiser Medicare Advantage back. If you have problems, let us know. We can get you enrolled in:
Medi Gap or Medicare Advantage with:
Blue Cross
United Health Care &
Blue Shield
Can I keep my group plan with over 20 employees and get an MAPD plan. I want the hearing aid benefits.
Good Question – Let’s set up a Zoom meeting to discuss it.