Blue Shield – Blue Cross Medicare Trial Rights, Birthday Rules to get
Medi Gap – Supplemental plans Plans – California
Introduction
Medi Gap Guaranteed Issue
There are only certain times (Special & Open Enrollment) when you can enroll in a Medi-Gap – Supplemental plans without Medical Health Underwriting questions. These times are called Guaranteed Acceptance – Issue.
Medi Gap is not like Medicare Advantage, where if you enroll when you turn 65 or at AEP Annual Open Enrollment, there are no health questions asked, or ACA under 65 Health Care Reform, where no questions are asked if you enroll at Open Enrollment (Age 65) or a Special Enrollment, See below.
The basic most common time, is when you turn 65.
See below of a summary of the times, then check with us [email protected] or the actual documents we’ve linked to for the exact rules.
- What is a better choice for Me?
- What's on this page?
- You Just turned 65
- MAPD Plan lowers benefits or raised premium
- If you are Under 65
- Birthday Rule
- On year Trial test of MAPD Plan
- Underwriting Holiday rules waived if you want to transfer from one Medi Gap plan to another
- Your Employer Coverage is ending
- Health Questions if you don't qualify for guaranteed issue
- You have a Change in Medi Cal Benefits
#Guaranteed Acceptance Guides Medi Gap
- Blue Shield
- Health Net
- Blue Cross Guaranteed Guide CA
- United Health Care - AARP - Email us [email protected]
- Get more detail compare contract explanation at:
Introduction to #MediGap
Our video explaining the Governments brochure on choosing a Medi Gap Policy. Click the little square on the right, to enlarge the video.
- 2023 Official Medicare Guide to choosing a Medi Gap Policy # 02110
- Get Quotes for Medi Gap Quotit
- Medicare Supplement Policies CA Insurance Code §§10192.1 - 10192.24
- CA Health Care Advocates HI CAP Fact Sheet
- Supplementing Medicare: An Overview 10-30-20 Hi Cap
- Supplementing Medicare: Medigap Plans 12-14-23 Hi Cap
- Your Rights to Purchase a Medigap 12-14-23 HI Cap
- Search for Participating Doctors & Hospitals - Just about ALL of them!
- Anthem Blue Cross Information & Enrollment
- United Health Care
- Blue Shield – Medi-Gap Information & Enrollment
- Health Net
-
Medi Gap pays the medical expenses that Original Medicare Part A (Hospital) and Part B (Doctor) doesn't. Check out the chart on this page to see what Medicare Pays, what you pay and what a Medi Gap plan pays.
- If you have a Medigap policy and get care, Medicare will pay its share of the Medicare-approved amount for covered health care costs. Then, your Medi-gap policy will pay its share. You’re responsible for any costs that are left. Medicare.Gov *
-
Original Medicare, Medicare Advantage nor Medi Gap pay for long term care either in a nursing home or at home care. Get more information on Long Term Care here. Even if you think you can't afford any extra premiums, there's a lot of valuable information to help with planning.
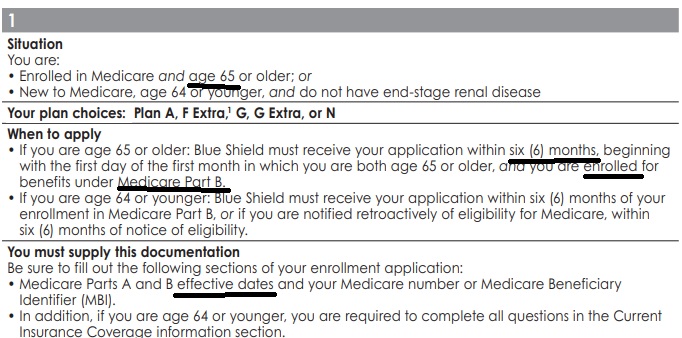
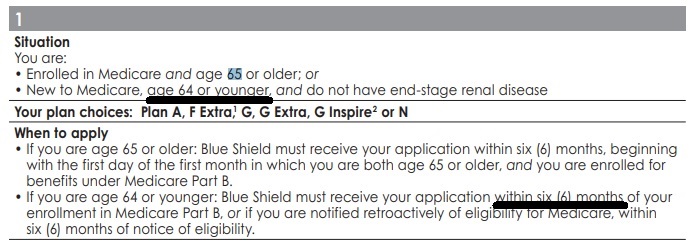
Medi Gap Guaranteed Issue Rules when you have #turned 65?
Or just enrolled in Part B?
Here’s Blue Shield rule from their Guaranteed Issue Guide:
When’s the best time to buy a Medi Gap policy?
The best time to buy a Medigap policy is during your Medigap Guaranteed Issue Open Enrollment Period. This period lasts for 6 months and begins on the first day of the month in which you’re both 65 or older and enrolled in Medicare Part B. Publication 02110 Page 14 & 45
FAQ’s just turned Age 65 or newly enrolled in Part B”
- Hello – I just signed up for Medicare Part B using the current GEP General Enrollment Period Timetable and Guaranteed Issue Availability Since I relied on Cobra coverage, which isn’t considered Employer Coverage, I will be subject to a penalty Am I entitled to a guaranteed issue Medigap policy, and how soon before July do I have to obtain the policy?
- Yes, under situation # 1 above, you are entitled to guaranteed issue Medi Gap as it says 65 and enrolled in Part B!
- I grant you, I don’t like the wording… but I’ve checked with the carriers and have actually had coverage issued.
- I suggest you enroll, as soon as you get confirmation that Part B has been approved!
- See our Medi Gap Pages for Blue Cross , UHC United Health and Blue Shield,
- There is no extra charge for our expertise. You can enroll online or we can help you in a Zoom meeting.
- From what I understand, the door is closing on signing up for Plan F
- If you mean the new rules under MACRA that starts in 2020 for those who are newly eligible. You would be OK as long as you were first eligible prior to January 2020. Otherwise, go for Plan G, the only difference is the $233 * Out of Hospital Medical Deductible
- 1 Is it true that one has to sign up for a Medigap plan within 6 months of starting Medicare?
2 I will be starting in June, [that’s when I turn 65] so can I wait until November to sign up for a Medi-gap plan ? (to save money?)- 1 Yes, see above for details
2 Yes, if I’m counting on my fingers correctly. Your six months would start in June.- I do not recommend that you wait. If this is your plan, you might be better off finding another agent to help you. Purposely waiting can only lead to a malpractice claim and a major hurt to your pocket book. If one knew when they were going to have a claim or be in an accident, they just wouldn’t leave the house that day.
- Will your next question be, how long can you wait to sign up for Part B?
- 3 months after the month you turn 65. That would save you $134/month.
- If you are on a budget, how about Hi F? You pay the first 2k of bills, not paid by Medicare A or B and you save around $100/month on premium. Get quotes and enroll online.
- 1 Yes, see above for details
#Guaranteed Acceptance Guides Medi Gap
- Blue Shield
- Health Net
- Blue Cross Guaranteed Guide CA
- United Health Care - AARP - Email us [email protected]
- Get more detail compare contract explanation at:
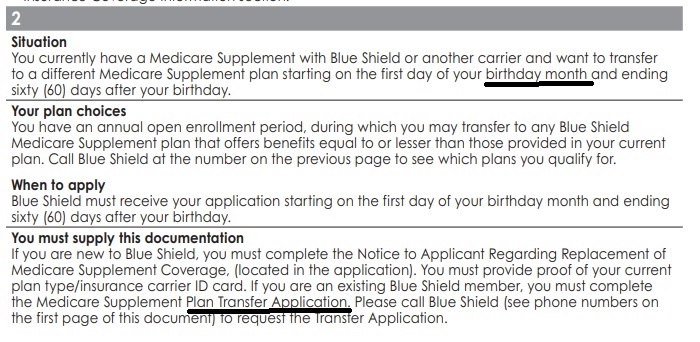
#Birthday Rule Medicare Guaranteed Issue rules
to change to plan A, F, G or N.
An individual shall be entitled to an annual open enrollment period lasting 60 days or more, commencing with the individual’s birthday, during which time that person may purchase any Medicare supplement coverage that offers benefits equal to or lesser than those provided by the previous coverage. 1358.11. (h) (1) * SB 407 Effective 7.1.2020?
Blue Cross Innovative F or G or Blue Shield Plan F or G Extra, count the same as F or G and don’t require underwriting. CA Health Care Advocates *
The application may be submitted 90 days in advance, for Blue Cross, but the effective date would be for the month after the clients birthday unless their birth date was on the 1st. CA Health Care Advocates * excerpt of email from BC 6.2.2020
- nor discriminate in the pricing of coverage, because of health status,
- claims experience,
- receipt of health care, or
- medical condition of the individual
Blue Shield – Birthday Rule – Chart
Typical Guidelines for all Insurance Companies
Guaranteed Issue Chart – Guide
California Birthday Rule FAQ’s
Don’t wait to wait for your birthday? Try Blue Shields and other companies Underwriting Holiday and/or Just go ahead & Answer Health Questions
Do NOT confuse the birthday rule with Medicare Advantage * AEP Annual Election Period October 15th to December 7th for the next January 1st. They are two totally separate things!!!
FAQ’s on “Birthday Rule”
- California’s birthday rule DOES NOT APPLY for Plan C Medicare Advantage
- MAPD Changes can be made only during end-of-year period AEP October 15 through December 7th or a special enrollment MAPD Open & Special Enrollments
- When is an application submitted?
- Received?
- By agent?
- Wrong Department of the Insurance Company?
- § 70.305 Timely mailing treated as timely filing.
- (a) General rule. Title 26 U.S.C. 7502 provides that, if the requirements of such section are met, a document shall be deemed to be filed on the date of the postmark stamped on the cover in which such document was mailed.
- (iii) (A) If the postmark on the envelope or wrapper is made by the U.S. Postal Service, such postmark must bear a date on or before the last date, or the last day of the period, prescribed for filing the document. https://www.law.cornell.edu/cfr/text/27/70.305
- From agent contract
- ***to present or propose to another for review, consideration, or decision merriam-webster.com/submit
- ***arstechnica.com/
- Date Calculator time and date.com/
- I’m transferring from Plan F to Plan G under the birthday rule to save premium. How come the Insurance Company called and asked about tobacco usage? It’s guaranteed issue isn’t it?
- CA Insurance Code 10192.11. (h) (1) … annual open enrollment period … During this open enrollment period, no issuer that falls under this provision shall deny or condition the issuance or effectiveness of Medicare supplement coverage, nor discriminate in the pricing of coverage, because of health status, claims experience, receipt of health care, or medical condition of the individual if, at the time of the open enrollment period, the individual is covered under another Medicare supplement policy or contract.
- So, is tobacco usage protected under health status?
- Resource Brokerage.com Central States Indemnity agent underwriting guide – CA requires Tobacco usage question even in Open Enrollment or Guaranteed Issue
- Alisprotect.com says tobacco rates don’t apply
- (24)(36) “Health status” means the determination bya carrier ofthe past, present, or expected risk of an individual or the employer due to the health conditions of THE INDIVIDUAL OR the employees of the employer.
(24.5) (37) “Health-status-related factor” means any of the following factors:- (a) Health status;
(b) Medical condition, including both physical and mental illnesses;
(c) Claims experience;
(d) Receipt of health care; Ch. 217 Insurance 913
(e) Medical history;
(f) Genetic information;
(g) Evidence of insurability, including conditions arising out of acts of domestic violence; and
(h) Disability. Colorado.Gov
- (a) Health status;
- One might also check with https://cahealthadvocates.org/ for their research, which isn’t answered on their website
- d. Tobacco Use – If a carrier reflects tobacco usage in the calculation of rates, then it shall do so according to the following requirements:
- (3) Any rate adjustment attributable to an individual (and all similarly situated individuals) based upon tobacco usage shall be applied to that individual (and all similarly situated individuals), and shall not be distributed to the entire group; and,
- h. Health status and claims experience may not be used as case characteristics. A health questionnaire, requesting reasonable information, may be used to obtain information about the health status of group enrollees. However, the health questionnaire may not be used in any way to determine the premium rate or any rating factor that is used in the determination of the premium rate that is charged to the group, except as provided in Subparagraph (d) of this paragraph. Colorado Secretary of State
- Confidential Agent Manual 2017
- Members who have smoked tobacco cigarettes or used any tobacco product at any time within the past 12 months will pay the tobacco rate. Non-tobacco rates apply to all applicants who meet open enrollment or guaranteed issue requirements.
- Obamacare/ACA doesn’t allow health questions, but it does allow tobacco usage to be surcharged 50%. CA though doesn’t allow the surcharge.
- If I sign up for Plan G, Hi-F Medicare Supplement plan now, can I easily switch to a regular Plan F or something higher later?
- The birthday rule above used to only allow you to change from one plan to another of the same or lesser value on your birthday. See the Medi Gap Plans A – N Chart.
- Underwriting Holiday or Freedom to Switch may allow you to do that.
- If you are healthy when you want to make a change, you can do that anytime. Here’s typical underwriting questions.
Steve talks about the Birthday Rule
Right to change to equal or lessor plan – 60 days – Innovative & Extra don’t count for making you do underwriting – answering health questions.
- Enroll in Blue Cross
- United Health Care email us [email protected] information
- Enroll in Blue Shield
- GET INSTANT Medi Gap QUOTES
- What's on this page?
- You Just turned 65
- MAPD Plan lowers benefits or raised premium
- If you are Under 65
- Birthday Rule
- On year Trial test of MAPD Plan
- Underwriting Holiday rules waived if you want to transfer from one Medi Gap plan to another
- Your Employer Coverage is ending
- Health Questions if you don't qualify for guaranteed issue
- You have a Change in Medi Cal Benefits
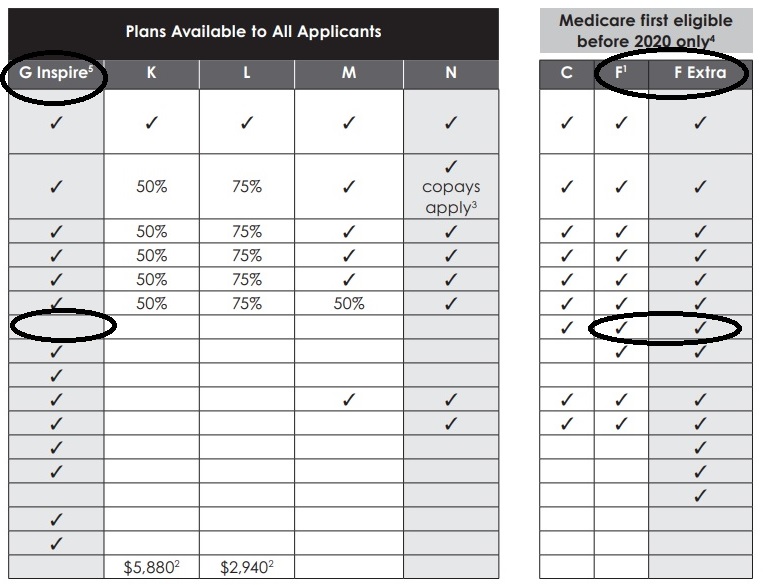
Transfer Application
No need to fill out Health Questions
When you fill out the transfer application under the birthday rule, whether ONLINE or Paper, check off the equal or lesser plan that you want.
![]()
Then put down the rule – situation # for the Insurance Company that you are using.
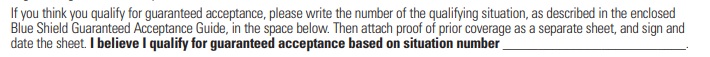
When you get to the Statement of Health, you don’t have to fill out any questions.
While these pictures are from the Blue Shield application, the general principles apply to all Insurance Companies.
Blue Shield of California Authorized Agent - Broker
![]()
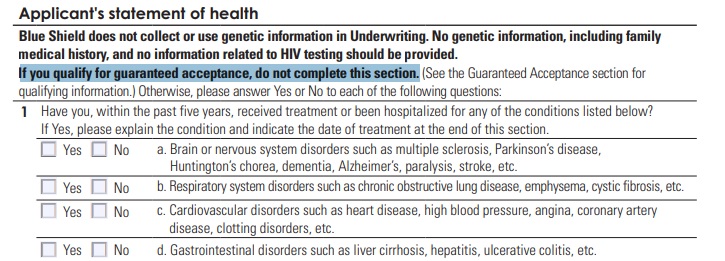
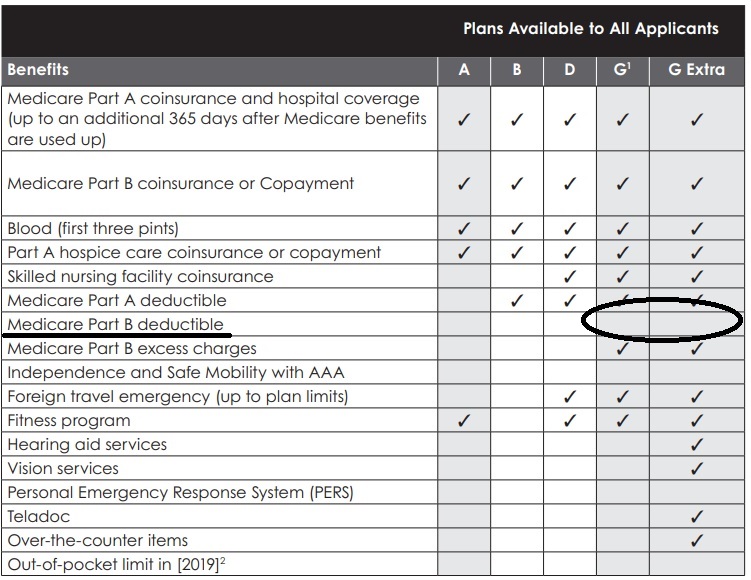
Medi Gap A - N #Chart
From Blue Shield Enrollment Guide
Click link or image to enlarge
 |
 |
- Our webpage on F vs G
- 2024 Fact Sheet Medicare Costs
- Fact Sheet Innovative Benefits Hi Cap
When you enroll beyond age 65 for Part B as you had
Qualifying #Employer Coverage
Termination of Employment or Retirement Plan
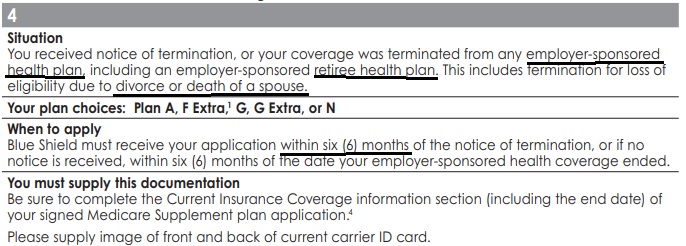
You have the right to purchase a Medi-gap policy for 6 months if your, your spouse’s or a family member’s current employment or retirement plan coverage terminates, or you lose your eligibility due to divorce or death of a spouse or family member. The 6-month period to apply for a Medigap policy starts on the date you receive notice that your health benefits will end. If you do not receive advance notice, the 6-month period starts the date the benefits end or the date of your first denied claim. This protection of California law applies whether your group health benefits were primary or secondary to Medicare.
Our webpage on the pros & cons of Employer Coverage vs Medicare
Loss of COBRA or Cal Cobra
You are also entitled to this protection when you become eligible for COBRA (Our webpage on COBRA) or have used up all your COBRA benefits. It does not apply if you stop paying COBRA premiums before you use all your benefits. COBRA benefits are always secondary to Medicare benefits unless you have ESRD and are in a 30-month coordination period. For more information on COBRA, see Medicare & Other Health Insurance. CA HealthCare Advocates *
COBRA and Medicare are VERY VERY confusing. Double check with us [email protected] on your specific situation!!!
You received notice of termination, or your coverage was terminated from any employer-sponsored health plan, including an employer-sponsored retiree health plan. This includes termination for loss of eligibility due to divorce or death of a spouse.
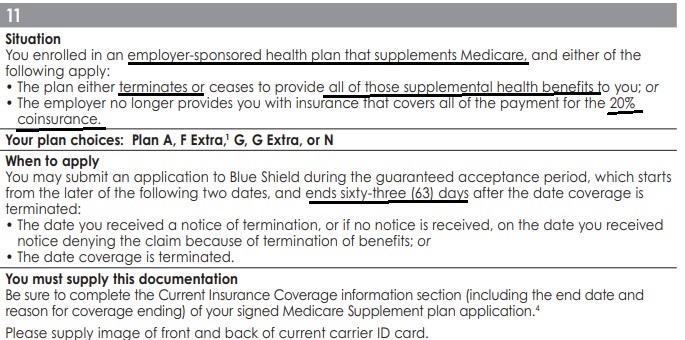
Situation 11
- You enrolled in an employer-sponsored health plan that supplements Medicare, §419 (e) Welfare Benefit Plans and either of the following apply:
- The plan either terminates or ceases to provide all of those supplemental health benefits to you; or
- The employer no longer provides you with insurance that covers all of the payment for the 20% coinsurance.
- Why is there Both situation 4 and 11?
- I asked and was told # 11 applies to §419 (e) Welfare Benefit Plans
- Learn More about not enrolling in Part B if you have employer coverage
- See our main page on loss of employer coverage
FAQ’s
Loss of Employer Coverage
- Where can one find the Official list for Medicare Advantage Plans, being as they differ from Medi Gap Plans?
- Are Medigap policies written during the 8-month Special Enrollment Period issued subject to the same terms as terms, with regard to pre-existing conditions, as those written during the Initial Enrollment Period?
- The waiver of Pre X would be the same. Situation # 4 above says the enrollment period is 6 months. It gets QUITE confusing with different rules for different enrollments… Part B Outpatient, Part D Rx, Medicare Advantage, etc. One has to check each option with a fine tooth comb!
- See links above to enroll online with Blue Cross and Blue Shield, email us for UHC United Health Care
- Here’s our scheduler to set a zoom meeting with screen sharing. set-a-meeting/
- See links above to enroll online with Blue Cross and Blue Shield, email us for UHC United Health Care
- The waiver of Pre X would be the same. Situation # 4 above says the enrollment period is 6 months. It gets QUITE confusing with different rules for different enrollments… Part B Outpatient, Part D Rx, Medicare Advantage, etc. One has to check each option with a fine tooth comb!
- I already have Medicare A and want part B. I am covered by a federal employee health plan (FEHB). Medicare (SSA) says I need to have a form filled out by my company president to verify employment- my W2 and tax form indicating coverage is not enough. Online it says my Medicare part B won’t start until July.
- We will answer that question on our page about if you have employer coverage – do you have to enroll in parts A, B & D?
- If you want more information and details – Please send a copy of your termination notice and if at all possible, all documents from your Employer’s Health Plan. Don’t hold back. We need to see if your under situation 4 or 11.
- Did the employer plan supplement Medicare or not?
- If one gets terminated from their spouses retiree benefits plan when the spouse passes away is there a guaranteed enrollment period into Medi Gap and how does it work?
- Yes. See situation # 4 above.
- If you cancel your Part B, then you to reinstate Part B later will you have guaranteed issue rights for Medi Gap?
- Excerpt from Medicare Medi Gap Guide # 02110 * Medicare.Gov *
- It’s also important to understand that your Medi gap rights may depend on when you choose to enroll in Medicare Part B. If you’re 65 or older, your Medigap Open Enrollment Period begins when you enroll in Part B and it can’t be changed or repeated.In most cases, it makes sense to enroll in Part B and purchase a Medi gap policy when you’re first eligible for Medicare, because you might otherwise have to pay a Part B late enrollment penalty and you might miss your Medi gap Open Enrollment Period. However, there are exceptions if you have employer coverage.
- From prior conversations and emails, you’ve stated that you have an application pending for Part B, but have not been enrolled. I’d check and see if you can get the application cancelled, as if you never asked to be enrolled in Part B.
- Either you or I can write to HICAP – CA Advocates and see what light they can put on the subject.
- This may be a question to learn when you got Part B and if you can get guaranteed issue at a later date…
- Excerpt from Medicare Medi Gap Guide # 02110 * Medicare.Gov *
Employer loss of Coverage Guaranteed Issue
CA Insurance Code §10192.11
(e) (1) An individual enrolled in Medicare Part B is entitled to open enrollment described in this section for six months following:
(A) Receipt of a notice of termination or, if no notice is received, the effective date of termination from any employer-sponsored health plan including an employer-sponsored retiree health plan.
(B) Receipt of a notice of loss of eligibility due to the divorce or death of a spouse or, if no notice is received, the effective date of loss of eligibility due to the divorce or death of a spouse, from any employer-sponsored health plan including an employer-sponsored retiree health plan.
(C) Termination of health care services for a military retiree or the retiree’s Medicare eligible spouse or dependent as a result of a military base closure or loss of access to health care services because the base no longer offers services or because the individual relocates.
(2) For purposes of this subdivision, “employer-sponsored retiree health plan” includes any coverage for medical expenses, including, but not limited to, coverage under the Consolidated Omnibus Budget Reconciliation Act of 1985 (COBRA) and the California Continuation Benefits Replacement Act (Cal-COBRA), that is directly or indirectly sponsored or established by an employer for employees or retirees, their spouses, dependents, or other included insureds.
Be careful and double check – COBRA might not get you out of the Part B Late Enrollment Penalty!
- Interaction between COBRA and Medigap Guaranteed Issue Requirements in Situations Involving Termination of Employer Group Coverage
#Understanding Medicare Advantage Plans (PDF) #12026
Insurance Companies get a fee from the Federal Government, when you enroll in an MAPD plan. MAPD Plans must cover all A & B services Medicare.Gov *
That's why the premium is very low or ZERO!
- Set a phone or Skype Meeting
- We can now do SOC Scope of Appointment, before the Meeting via a 3 minute recorded meeting 2 days before. AHIP Training Module 4 Page 14 *
- #Intake Form - We can better prepare for the meeting
- Medicare Advantage (Medicare Part C): An Overview Hi Cap
- HMO - Narrow Networks?
- HI Cap CA Health Care Advocates Fact Sheet
- Do I just sign up with a Medicare Advantage Company and automatically get * Parts A & B or do I have to get those from Medicare.Gov * VIDEO
- Get Quotes, Full Information and Enroll
- MANDATED wording!: Think Advisor * ‘‘We do not offer every plan available in your area. Any information we provide is limited to those plans we do offer in your area. Please contact Medicare.gov or 1–800–MEDICARE to get information on all of your options.’’
- We disagree with the above wording, as we can use the same tools on Medicare.gov as they do!
- FYI a 4.27.2022 HHS Office of the Inspector General report found that MAPD plans denied 13% of prior authorizations that would have been covered under original Medicare (Conversely, Medi Gap, just follows what Medicare pays.)
- 88% of MAPD enrollees are happy
-
MAPD plans often include Dental & Part D - Rx Prescriptions and often have NO premiums!
-
How is that possible?
-
The Federal Government pays them around $700/month to handle your medical care. You must continue to pay your Medicare Part B premium of about $170/month. It's best to apply when you turn 65 for the supplement plans or advantage plans, as that's the main "Open Enrollment" period, guaranteed issue for any plan.
-
-
-
Medicare Advantage Plans also have an annual open enrollment now known as AEP Annual Election Period October 7 to December 15th.
-
Additional Coverage is important as Medical Bills are increasing Seniors Credit Card Debt or leading to possible bankruptcy?
- If You Have Problems with Your Medicare Advantage Plan
- When Medicare Advantage Plans Terminate Coverage
- Medi-Cal D-SNP Feasibility Study
Medicare #Trial Period rules & guarantees about if you get a
Medicare Advantage Plan MAPD and
then you would rather switch to Originial Medicare A-Hospital & B- Doctor Visits and a Medi-Gap plan?
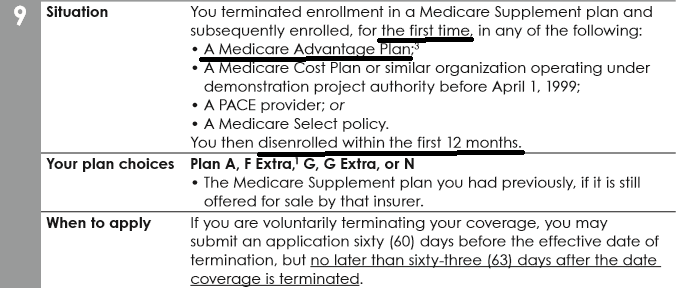
There is a Medicare Advantage 12 month trial period (free-look) in which you can get an MAPD and come back to Medi Gap. This trial period can be either when you first turn 65, or you drop a Medi-Gap plan to enroll in a MAPD Plan.
FAQ’s
MAPD Trial Period – Come back to Medicare and Medi-Gap”
- Question I enrolled in a Medi-Gap plan, last year when I turned 65. If I enroll in a Medicare Advantage plan, can we go back to our Medi Gap plan anytime or do we have to wait for Open Enrollment, 10.15 to 12.7 annually?
. - Answer If you cancel the MAPD plan within 12 months, you can go back to your Medi Gap plan.
- If you stay in the MAPD plan longer than a year, you would have to meet underwriting – health questions to get a Medi Gap policy. There might be some Insurance Companies more liberal, but the law doesn’t require it.
- Check with us when you’re ready to change. Sometimes there are “limited time” special offers, underwriting holidays – freedom to switch
- The Open Enrollment Period is only for MAPD and Part D Rx guaranteed sign up, switching plans or going back to original medicare, Parts A & B.
- Again, if you are in a MAPD plan longer than a year, it’s not guaranteed issue to get your Medi Gap plan back
- The Trial right is only for the first time you drop Medi Gap to try MAPD
.
- Question If I understand it, this benefit – Right to get a Medi Gap Plan occurs because there is a “trial” period for MA in certain cases. However, those cases don’t seem to include the case in which MA was obtained upon returning from overseas. What am I missing?
.- Answer Federal Guaranteed Rights to get Medi Gap is shown in Publication 02110 above
- You are right, in your case, as you are not currently living in the USA you wouldn’t be joining at age 65, since you are not resident in any MAPD Service area.
- Check the other guaranteed issue rights, like if there is a change in premium or benefits.
- Blue Shield is liberal… Plus CA has or may have more liberal rights for guaranteed issue into Medi Gap Check out situation 14 Check out Situation # 17 if you get another company who changes benefits or premium 15% or more…
- One must read all these rules at least 3 times and then when you think you understand it, read it again. Justice Felix Frankfurter
.
- Question Do I understand correctly that a MAPD plan that was guaranteed issued, as I was living overseas and returned to USA as we discussed in this can be reverted to original Medicare + Medigap also on a guaranteed issue basis after a year?
- Answer Yes. That’s what this whole section is about. See above for details and explanation. If you have further questions, email us
Medi Gap Plans from Anthem Blue Cross –
Click for Information and ONLINE enrollment
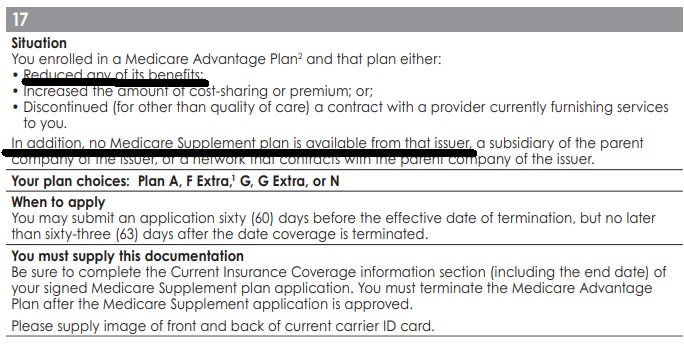
Renewal Medicare Advantage Plan offers #less benefits or raises premium
Excerpt from Blue Shield
Situation # 17
CA Insurance Code §10192.12 (D) (i) The Medicare Advantage plan in which the individual is enrolled reduces any of its benefits or increases the amount of cost sharing or premium or discontinues for other than good cause relating to quality of care its relationship or contract under the plan with a provider who is currently furnishing services to the individual.
An individual shall be eligible under this subparagraph for a Medicare supplement policy issued by the same issuer through which the individual was enrolled at the time the reduction, increase, or discontinuance described above occurs or, commencing January 1, 2007, for one issued by a subsidiary of the parent company of that issuer or by a network that contracts with the parent company of that issuer.
If no Medicare supplement policy is available to the individual from the same issuer, a subsidiary of the parent company of the issuer, or a network that contracts with the parent company of the issuer, the individual shall be eligible for a Medicare supplement policy pursuant to paragraph (1) of subdivision (e) issued by any issuer, if the Medicare Advantage plan in which the individual is enrolled does any of the following:
(I) Increases the premium by 15 percent or more.
(II) Increases physician, hospital, or drug copayments by 15 percent or more.
(III) Reduces any benefits under the plan.
(IV) Discontinues, for other than good cause relating to quality of care, its relationship or contract under the plan with a provider who is currently furnishing services to the individual.
(ii) Enrollment in a Medicare supplement policy from an issuer unaffiliated with the issuer of the Medicare Advantage plan in which the individual is enrolled shall be permitted only during the annual election period for a Medicare Advantage plan, except where the Medicare Advantage plan has discontinued its relationship with a provider currently furnishing services to the individual. Nothing in this section shall be construed to authorize an individual to enroll in a group Medicare supplement policy if the individual does not meet the eligibility requirements for the group.
- I don’t see that the Federal Law per the Medi Gap Guide has this rule.
- AARP – Have us or your agent review bullet points 7 & 8 in confidential agent manual.
I have Medicare and I’m #under 65,
What Medi Gap or Medicare Advantage Plans can I get?
If you are under 65 and have Medicare due to a disability, SSDI, SSI? you can get Part D Rx, Medicare Advantage and Medi Gap plans, guaranteed issue, no medical questions asked, in California by enrolling when you are first eligible or in the case of Part D & Medicare Advantage, at Open Enrollment 10.15 to 12.7 each year. Other states may differ, learn more CA Healthline 1.4.2016.
When you turn 65, that gives you an additional time to enroll in a Medicare Supplement plan at LOWER rates.
See Medicare and You # 10050 and each Insurance Companies Web Page (see menu above) for details, brochures, enrollment forms and rates.
Please email us, [email protected] if you want more personalized attention.
FAQ’s, Resources & Links
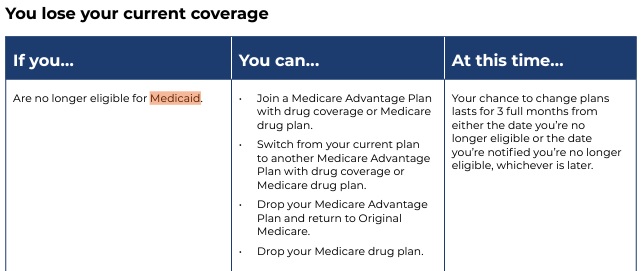
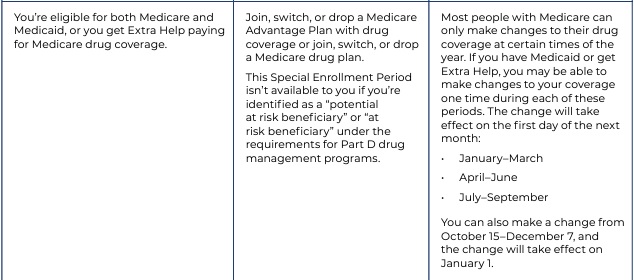
Special Enrollment times for Medicare Advantage
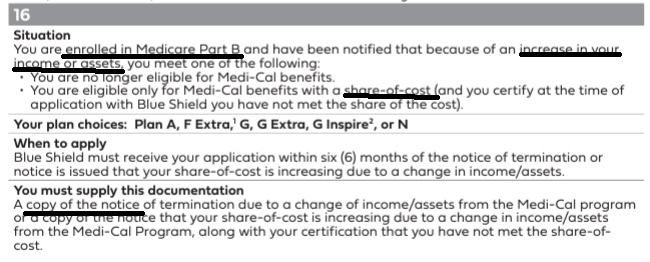
Guaranteed Right to get Medi Gap if your #Medi-Cal benefits change...
- You can deduct the cost of that policy or product and that may help them get under the strict income limit in the Aged & Disabled Federal Poverty Level FPL and Blind FPL programs. See above, you must have original Medicare, A & B not Medicare Advantage. Learn More Medicare.gov
- You may be able to drop Medicare Advantage - but that is up to YOU! We are not telling you to do it!
- If your purchase private health insurance with coverage that duplicates Medi-Cal coverage, the private health coverage would be billed first and then Medi–Cal would pay for the services it covers after the private health carrier pays or denies a claim. Our webpage on Dual Coverage * Western Center Law & Poverty Guide for Low Income Americans * CA Code of Regulations 22 § 50555.2 * Health Care Rights.org *
Guaranteed Issue Rules to Get Medi Gap
- Here’s a video explanation of our research on how one might get Medi Gap even if they are not healthy. If you have a Medicare Advantage plan, see also Situation # 17
- Visit our Medi Gap Guaranteed Issue Page
- Problems getting Medi Gap if you have full benefits Medi Cal?
Right to Opt out of Medicare Advantage
FAQ’s “Under 65 disabled & Medicare Qualified”
- I have been trying to get a Medicare supplement for two years. NO one will give me one. I get denied for anything, for an H. Pylori infection. Every company I apply with denies me. I was born in 1957 and have Medicare but no company will give me a supplement. They all want to give me prescription drug plan while denying the medical plan. I live in California.
- How about Medicare Advantage at the next Open Enrollment? Medicare Advantage is guaranteed issue, while Medicare Supplements where you can go to any doctor or hospital that accepts Medicare is not. Check out our page on when Supplements are guaranteed issue. See also the subpage where if you take a Medicare Advantage Plan and don’t like it, you can then get a supplement. Let’s talk privately about some companies that have an unofficial practice of being more liberal…
- Please note that Medicare Supplements are not like Obama Care, there is no right to guaranteed issue, any time. Even Obama Care has certain open enrollment periods. See our page on Medical Loss Ratio, the Insurance Companies take in a small premium…from lots of people, but have to be able to pay all claims from all policy holders. See also the new page – under construction we are building on Donald Care. It appears that many of our leaders don’t understand medical underwriting and the law of large numbers.
- Hi. I’m looking for the best price on a Pre-65 Plan N supplement. We have Anthem at $249/month. My wife is on Social Security Disability. Birthdate: 10/25/1954. The price for Anthem started at $174 and after six months they raised it to $249. Any possibilities we should look into?
- I’ve responded to you privately. Use the menu above to check out other companies for Medi-Gap… but there may be a problem with Guaranteed Issue. In October there is Medicare Advantage.
Steve talks about Plan G & Extra - Innovative VIDEO
What Plan G pays in addition to Medicare Parts A & B
- Check our Carrier Pages for the latest Info
- Anthem Blue Cross
- Blue Shield – Medi-Gap
- Email us [email protected] for UHC United Health Care information
What are the Medical #Underwriting Questions for a Medi-Gap policy
if I’m not in a guaranteed issue period, like just turning 65?
Check the paper applications below and review the questions:
- Blue Cross Application – Section 2A
- Blue Shield Application Page 121 of Enrollment Kit – Page 6 Application
- We have other companies that don’t allow agents to post information…. email us [email protected]
- Possible Pre X period if you don’t have prior creditable coverage
- Email us to discuss [email protected]
“Medical Questions – Underwriting – If not in Guaranteed Issue Period?”
- CANCER
- I have Plan F Medi Gap and applied for Plan G to save premium. So what if the Part B Deductible is higher. It wasn’t my birthday. What RIGHT does the Insurance Company have to deny the transfer because I had an alleged pre-existing condition a nothing squamous cell skin cancer. It’s hard to find someone who has not had a skin cancer
- 1st off, when I ask my higher ups at any of the Medi Gap Insurance Carriers about health underwriting, I get a blank stare, as most everyone gets a Medi Gap policy or change at a Guaranteed Issue date – period.
- Thus, I can’t get underwriting guidelines from anyone. Here’s an excerpt from a well known carrier, prior to ACA/Obamacare when asking health questions and pre X clauses where outlawed for under 65. Conversely, there is a mandate and only certain times one can enroll.
- There are exclusions for tons of stuff. Insurance Companies need to collect $1 to pay claims of 80 cents. It’s called MRL Medical Loss Ratio and is written into ACA/Obamcare. It was pretty much the way it was before.
- Insurance underwriters evaluate the risk and exposures of potential clients. They decide how much coverage the client should receive, how much they should pay for it, or whether even to accept the risk and insure them. Underwriting involves measuring risk exposure and determining the premium that needs to be charged to insure that risk. The function of the underwriter is to protect the company’s book of business from risks that they feel will make a loss and issue insurance policies at a premium that is commensurate with the exposure presented by a risk.
- Each insurance company has its own set of underwriting guidelines to help the underwriter determine whether or not the company should accept the risk. The information used to evaluate the risk of an applicant for insurance will depend on the type of coverage involved. For example, in underwriting automobile coverage, an individual’s driving record is critical. However, the type of automobile is actually far more critical. As part of the underwriting process for life or health insurance, medical underwriting may be used to examine the applicant’s health status (other factors may be considered as well, such as age & occupation). The factors that insurers use to classify risks are generally objective, clearly related to the likely cost of providing coverage, practical to administer, consistent with applicable law, and designed to protect the long-term viability of the insurance program.[3]
- The underwriters may decline the risk or may provide a quotation in which the premiums have been loaded (including the amount needed to generate a profit, in addition to covering expenses[4]) or in which various exclusions have been stipulated, which restrict the circumstances under which a claim would be paid. Depending on the type of insurance product (line of business), insurance companies use automated underwriting systems to encode these rules, and reduce the amount of manual work in processing quotations and policy issuance. This is especially the case for certain simpler life or personal lines (auto, homeowners) insurance. Some insurance companies, however, rely on agents to underwrite for them. This arrangement allows an insurer to operate in a market closer to its clients without having to establish a physical presence.
- Two major categories of exclusion in insurance underwriting are moral hazard and correlated losses.[5] With a moral hazard, the consequences of the customer’s actions are insured, making the customer more likely to take costly actions. For example, bedbugs are typically excluded from homeowners’ insurance to avoid paying for the consequence of recklessly bringing in a used mattress.[5] Insured events are generally those outside the control of the customer, for example (typical in life insurance) death by automobile accident, contrasted with death by suicide. Correlated losses are those that can affect a large number of customers at the same time, thus potentially bankrupting the insurance company. This is why typical homeowner’s policies cover damage from fire or falling trees (usually affecting an individual house), but not floods or earthquakes (which affect many houses at the same time).[5] https://en.wikipedia.org/wiki/Underwriting#Insurance_underwriting
- Here’s our webpage on the rate review process. That is, the CA Department of Insurance reviews the rates and underwriting guidelines to make sure they are actuarially sound.
- COST OF TREATMENT FOR SQUAMOUS CELL CARCINOMA OF THE HEAD AND NECK IN THE UNITED STATES
- Average per patient cost of care for SCCHN in the US was estimated to be $20,876.
- Higher costs resulted for patients that present with advanced cancers.
- The estimated cost of treating a patient with Stage IV lip SCC ($19,274) was four times that of Stage 0 lip SCC ($5,062).
- The site with the lowest cost of treatment was lip ($7,261) while the highest cost was associated with hypopharyngeal SCC ($28,584).
- The cost per patient for palliative care ranged from $2,052 for lip SCC (28% of total cost of care) to $7,172 for sinonasal SCC (30% of total cost of care).
- The lifetime cost of managing annual incident SCCHN cases was estimated to approximate $976 million.
- CONCLUSION: This study found that tumor stage and location are useful predictors of increased treatment costs. The results suggest that prevention and early detection are critical in reducing the treatment costs of SCCHN. wiley.com/
- I’m living outside the USA, if I apply for a Medigap plan and am subject to underwriting, how much extra would coverage cost and what are the underwriting requirements?
- The requirements or at least the questions are in the respective insurance company applications.
- The price – premium is the same for those who enroll during a SEP or Guaranteed Enrollment Period. You can get those rates on our webpages for each company by using the site map, menu above or the link above to Blue Cross and Blue Shield affiliate sites.
- I find it very odd that there are some situations where you can be offered an underwriting-free MediGap choice upon return to the US.
- Is this only if you have or once had a policy?
- What if the provider cancels the policy when you are out of state/country (as it can do)?
- Those situations are limited to getting a Medicare Advantage Plan and then using the Trial Period to get a Medi-Gap plan or did I forget an SEP into Medi Gap?
- MAPD enrollment when returning to USA doesn’t matter on if you had a MAPD or Medi Gap policy before.
- I’m not aware that a Medi Gap carrier can cancel coverage when you move out of state or country. Residency is only required when you purchase coverage.
- I don’t ever want to deal with underwriting because even though I’m a healthy person, the insurance companies may look at the info in the MIB and think I am not. So it sounds like I should get a regular Plan F at the get go when starting Medicare in June. Is that what you would recommend?
- How healthy are you, related to the questions on the applications above?
- Have your reviewed your MIB Medical Information Bureau File? https://www.mib.com/request_your_record.html
- MIB shouldn’t have anything that isn’t being asked in the applications. There’s a law somewhere that says Insurance Companies cannot deny you based only on the MIB file. They can only use it to indicate things that need to be investigated further.
- If you want the Medi Gap plan with the highest benefits Plan F and don’t want to worry about underwriting, yes.
“Underwriting #Holiday”
Freedom to Switch
Blue Shield is offering a Underwriting Holiday offer beginning on June 1 through December 31, 2023. Email 8.31.2022 & 9.27.2022
This offer allows you to enroll in ANY* available Blue Shield of California Medicare Supplement plan without answering any health questions or obtaining underwriting approval. You can enroll in ANY* available Blue Shield of California Medicare Supplement Plan without answering any health questions or obtaining underwriting approval.
email us [email protected] for more details
Sometimes, The Insurance Companies might have a “Underwriting Holiday” or Freedom to Switch where you can change to the Insurance Company celebrating the Holiday with NO health questions, as long as you currenlty have a Medi Gap Plan and sometimes a Medicare Advantage Plan.
We don’t have a crystal ball and the Companies don’t seem to allow us to post information about the holidays. So, email us [email protected] and we can let you know the current offerings.
Be sure to do this early in AEP so that there isn’t any lapse in getting Part D Rx… See our webpage on Part D enrollment periods.
*Plan F is limited to those who became Medicare eligible before 1.1.2020, learn more MACRA
InsuBuy International Medical Coverage –
Instant Quotes & Enrollment
Coverage for Travel - $50k Emergency under Medicare Medi Gap or MAPD Advantage may not be enough!
CA Insurance Code §10192.11 (h) open enrollment birthday Rule
(h) (1) An individual shall be entitled to an annual open enrollment period lasting 30 days or more, commencing with the individual’s birthday, during which time that person may purchase any Medicare supplement policy that offers benefits equal to or lesser than those provided by the previous coverage. During this open enrollment period, no issuer that falls under this provision shall deny or condition the issuance or effectiveness of Medicare supplement coverage, nor discriminate in the pricing of coverage, because of health status, claims experience, receipt of health care, or medical condition of the individual if, at the time of the open enrollment period, the individual is covered under another Medicare supplement policy or contract. An issuer shall notify a policyholder of his or her rights under this subdivision at least 30 and no more than 60 days before the beginning of the open enrollment period.,
CA Health Advocates More
(a)
(1) With respect to the guaranteed issue of a Medicare supplement policy, eligible persons are those individuals described in subdivision (b) who seek to enroll under the policy during the period specified in subdivision (c), and who submit evidence of the date of termination or disenrollment or enrollment in Medicare Part D with the application for a Medicare supplement policy.
(2) With respect to eligible persons, an issuer shall not take any of the following actions:
(A) Deny or condition the issuance or effectiveness of a Medicare supplement policy described in subdivision (e) that is offered and is available for issuance to new enrollees by the issuer.
(B) Discriminate in the pricing of that Medicare supplement policy because of health status, claims experience, receipt of health care, or medical condition.
(C) Impose an exclusion of benefits based on a preexisting condition under that Medicare supplement policy.
(b) An eligible person is an individual described in any of the following paragraphs:
(1) The individual is enrolled under an employee welfare benefit plan that provides health benefits that supplement the benefits under Medicare and either of the following applies:
(A) The plan either terminates or ceases to provide all of those supplemental health benefits to the individual.
(B) The employer no longer provides the individual with insurance that covers all of the payment for the 20-percent coinsurance.
Definitions leginfo.legislature.ca.gov
(g) “Employee welfare benefit plan” means a plan, fund, or program of employee benefits as defined in Section 1002 of Title 29 of the United States Code (Employee Retirement Income Security Act). erisa
law.cornell.edu/uscode/text/29/1002
(1) The terms “employee welfare benefit plan” and “welfare plan” mean any plan, fund, or program which was heretofore or is hereafter established or maintained by an employer or by an employee organization, or by both, to the extent that such plan, fund, or program was established or is maintained for the purpose of providing for its participants or their beneficiaries, through the purchase of insurance or otherwise, (A) medical, surgical, or hospital care or benefits, or benefits in the event of sickness, accident, disability, death or unemployment, or vacation benefits, apprenticeship or other training programs, or day care centers, scholarship funds, or prepaid legal services, or (B) any benefit described in section 186(c) of this title (other than pensions on retirement or death, and insurance to provide such pensions).
(2) The individual is enrolled with a Medicare Advantage organization under a Medicare Advantage plan under Medicare Part C, and any of the following circumstances apply:
(A) The certification of the organization or plan has been terminated.
(B) The organization has terminated or otherwise discontinued providing the plan in the area in which the individual resides.
Health Net Guide Rev. 7.2015 # 5 on page 6
medicare advocacy.org/when-a-medicare-advantage-plan-does-not-renew-its-contract
(C) The individual is no longer eligible to elect the plan because of a change in the individual’s place of residence or other change in circumstances specified by the secretary. Those changes in circumstances shall not include termination of the individual’s enrollment on the basis described in Section 1851(g)(3)(B) of the federal Social Security Act where the individual has not paid premiums on a timely basis or has engaged in disruptive behavior as specified in standards under Section 1856 of the federal Social Security Act, or the plan is terminated for all individuals within a residence area.
(D)
(i) The Medicare Advantage plan in which the individual is enrolled reduces any of its benefits or increases the amount of cost sharing or premium or discontinues for other than good cause relating to quality of care its relationship or contract under the plan with a provider who is currently furnishing services to the individual. An individual shall be eligible under this subparagraph for a Medicare supplement policy issued by the same issuer through which the individual was enrolled at the time the reduction, increase, or discontinuance described above occurs or, commencing January 1, 2007, for one issued by a subsidiary of the parent company of that issuer or by a network that contracts with the parent company of that issuer. If no Medicare supplement policy is available to the individual from the same issuer, a subsidiary of the parent company of the issuer, or a network that contracts with the parent company of the issuer, the individual shall be eligible for a Medicare supplement policy pursuant to paragraph (1) of subdivision (e) issued by any issuer, if the Medicare Advantage plan in which the individual is enrolled does any of the following:
(I) Increases the premium by 15 percent or more.
(II) Increases physician, hospital, or drug copayments by 15 percent or more.
(III) Reduces any benefits under the plan.
(IV) Discontinues, for other than good cause relating to quality of care, its relationship or contract under the plan with a provider who is currently furnishing services to the individual.
(ii) Enrollment in a Medicare supplement policy from an issuer unaffiliated with the issuer of the Medicare Advantage plan in which the individual is enrolled shall be permitted only during the annual election period for a Medicare Advantage plan, except where the Medicare Advantage plan has discontinued its relationship with a provider currently furnishing services to the individual. Nothing in this section shall be construed to authorize an individual to enroll in a group Medicare supplement policy if the individual does not meet the eligibility requirements for the group.
See our new page on the cost sharing rule
(E) The individual demonstrates, in accordance with guidelines established by the secretary, either of the following:
(i) The organization offering the plan substantially violated a material provision of the organization’s contract under this article in relation to the individual, including the failure to provide on a timely basis medically necessary care for which benefits are available under the plan or the failure to provide the covered care in accordance with applicable quality standards.
(ii) The organization, or agent or other entity acting on the organization’s behalf, materially misrepresented the plan’s provisions in marketing the plan to the individual.
(F) The individual meets other exceptional conditions as the secretary may provide.
-
-
- Question I lost employer coverage MAPD and was not informed of my right to purchase a Medi Gap plan. Would that be a material violation under item # 13 of the Blue Shield listing?
. - Here’s Our Research Check out these references:
- Official Guide to Medi Gap Page 3, right to buy Medi Gap policy and page 4 ESRD and Employer Coverage
- ca health advocates.org
- Question I lost employer coverage MAPD and was not informed of my right to purchase a Medi Gap plan. Would that be a material violation under item # 13 of the Blue Shield listing?
-
(3) The individual is 65 years of age or older, is enrolled with a Program of All-Inclusive Care for the Elderly (PACE) provider under Section 1894 of the federal Social Security Act, and circumstances similar to those described in paragraph (2) exist that would permit discontinuance of the individual’s enrollment with the provider, if the individual were enrolled in a Medicare Advantage plan.
(4) The individual meets both of the following conditions:
(A) The individual is enrolled with any of the following:
(i) An eligible organization under a contract under Section 1876 of the federal Social Security Act (Medicare cost).
(ii) A similar organization operating under demonstration project authority, effective for periods before April 1, 1999.
(iii) An organization under an agreement under Section 1833(a)(1)(A) of the federal Social Security Act (health care prepayment plan).
(iv) An organization under a Medicare Select policy.
(B) The enrollment ceases under the same circumstances that would permit discontinuance of an individual’s election of coverage under paragraph (2) or (3).
(5) The individual is enrolled under a Medicare supplement policy, and the enrollment ceases because of any of the following circumstances:
(A) The insolvency of the issuer or bankruptcy of the nonissuer organization, or other involuntary termination of coverage or enrollment under the policy.
(B) The issuer of the policy substantially violated a material provision of the policy.
(C) The issuer, or an agent or other entity acting on the issuer’s behalf, materially misrepresented the policy’s provisions in marketing the policy to the individual.
(6) The individual meets both of the following conditions:
(A) The individual was enrolled under a Medicare supplement policy and terminates enrollment and subsequently enrolls, for the first time, with any Medicare Advantage organization under a Medicare Advantage plan under Medicare Part C, any eligible organization under a contract under Section 1876 of the federal Social Security Act (Medicare cost), any similar organization operating under demonstration project authority, any PACE provider under Section 1894 of the federal Social Security Act, or a Medicare Select policy.
(B) The subsequent enrollment under subparagraph (A) is terminated by the individual during any period within the first 12 months of the subsequent enrollment (during which the enrollee is permitted to terminate the subsequent enrollment under Section 1851(e) of the federal Social Security Act).
(7) The individual upon first becoming eligible for benefits under Medicare Part A at 65 years of age enrolls in a Medicare Advantage plan under Medicare Part C or with a PACE provider under Section 1894 of the federal Social Security Act, and disenrolls from the plan or program not later than 12 months after the effective date of enrollment.
Some companies are more liberal and offer two years. More detail
(8) The individual while enrolled under a Medicare supplement policy that covers outpatient prescription drugs enrolls in a Medicare Part D plan during the initial enrollment period terminates enrollment in the Medicare supplement policy, and submits evidence of enrollment in Medicare Part D along with the application for a policy described in paragraph (4) of subdivision (e).
(c)
(1) In the case of an individual described in paragraph (1) of subdivision (b), the guaranteed issue period begins on the later of the following two dates and ends on the date that is 63 days after the date the applicable coverage terminates:
(A) The date the individual receives a notice of termination or cessation of all supplemental health benefits or, if no notice is received, the date of the notice denying a claim because of a termination or cessation of benefits.
(B) The date that the applicable coverage terminates or ceases.
(2) In the case of an individual described in paragraphs (2), (3), (4), (6), and (7) of subdivision (b) whose enrollment is terminated involuntarily, the guaranteed issue period begins on the date that the individual receives a notice of termination and ends 63 days after the date the applicable coverage is terminated.
(3) In the case of an individual described in subparagraph (A) of paragraph (5) of subdivision (b), the guaranteed issue period begins on the earlier of the following two dates and ends on the date that is 63 days after the date the coverage is terminated:
(A) The date that the individual receives a notice of termination, a notice of the issuer’s bankruptcy or insolvency, or other similar notice if any.
(B) The date that the applicable coverage is terminated.
(4) In the case of an individual described in paragraph (2), (3), (6), or (7) of, or in subparagraph (B) or (C) of paragraph (5) of, subdivision (b) who disenrolls voluntarily, the guaranteed issue period begins on the date that is 60 days before the effective date of the disenrollment and ends on the date that is 63 days after the effective date of the disenrollment.
(5) In the case of an individual described in paragraph (8) of subdivision (b), the guaranteed issue period begins on the date the individual receives notice pursuant to Section 1882(v)(2)(B) of the federal Social Security Act from the Medicare supplement issuer during the 60-day period immediately preceding the initial enrollment period for Medicare Part D and ends on the date that is 63 days after the effective date of the individual’s coverage under Medicare Part D.
(6) In the case of an individual described in subdivision (b) who is not included in this subdivision, the guaranteed issue period begins on the effective date of disenrollment and ends on the date that is 63 days after the effective date of disenrollment.
(d)
(1) In the case of an individual described in paragraph (6) of subdivision (b), or deemed to be so described pursuant to this paragraph, whose enrollment with an organization or provider described in subparagraph (A) of paragraph (6) of subdivision (b) is involuntarily terminated within the first 12 months of enrollment and who, without an intervening enrollment, enrolls with another such organization or provider, the subsequent enrollment shall be deemed to be an initial enrollment described in paragraph (6) of subdivision (b).
(2) In the case of an individual described in paragraph (7) of subdivision (b), or deemed to be so described pursuant to this paragraph, whose enrollment with a plan or in a program described in paragraph (7) of subdivision (b) is involuntarily terminated within the first 12 months of enrollment and who, without an intervening enrollment, enrolls in another such plan or program, the subsequent enrollment shall be deemed to be an initial enrollment described in paragraph (7) of subdivision (b).
(3) For purposes of paragraphs (6) and (7) of subdivision (b), an enrollment of an individual with an organization or provider described in subparagraph (A) of paragraph (6) of subdivision (b), or with a plan or in a program described in paragraph (7) of subdivision (b) shall not be deemed to be an initial enrollment under this paragraph after the two-year period beginning on the date on which the individual first enrolled with such an organization, provider, plan, or program.
(e)
(1) Under paragraphs (1), (2), (3), (4), and (5) of subdivision (b), an eligible individual is entitled to a Medicare supplement policy that has a benefit package classified as Plan A, B, C, F (including a high deductible Plan F), K, L, M, or N offered by any issuer.
(2)
(A) Under paragraph (6) of subdivision (b), an eligible individual is entitled to the same Medicare supplement policy in which he or she was most recently enrolled, if available from the same issuer. If that policy is not available, the eligible individual is entitled to a Medicare supplement policy that has a benefit package classified as Plan A, B, C, F (including a high deductible Plan F), K, L, M, or N offered by any issuer.
(B) On and after January 1, 2006, an eligible individual described in this paragraph who was most recently enrolled in a Medicare supplement policy with an outpatient prescription drug benefit is entitled to a Medicare supplement policy that is available from the same issuer but without an outpatient prescription drug benefit or, at the election of the individual, has a benefit package classified as a Plan A, B, C, F (including high deductible Plan F), K, L, M, or N that is offered by any issuer.
(3) Under paragraph (7) of subdivision (b), an eligible individual is entitled to any Medicare supplement policy offered by any issuer.
(4) Under paragraph (8) of subdivision (b), an eligible individual is entitled to a Medicare supplement policy that has a benefit package classified as Plan A, B, C, F (including a high deductible Plan F), K, L, M, or N and that is offered and is available for issuance to a new enrollee by the same issuer that issued the individual’s Medicare supplement policy with outpatient prescription drug coverage.
(f)
(1) At the time of an event described in subdivision (b) by which an individual loses coverage or benefits due to the termination of a contract or agreement, policy, or plan, the organization that terminates the contract or agreement, the issuer terminating the policy, or the administrator of the plan being terminated, respectively, shall notify the individual of his or her rights under this section and of the obligations of issuers of Medicare supplement policies under subdivision (a). The notice shall be communicated contemporaneously with the notification of termination.
(2) At the time of an event described in subdivision (b) by which an individual ceases enrollment under a contract or agreement, policy, or plan, the organization that offers the contract or agreement, regardless of the basis for the cessation of enrollment, the issuer offering the policy, or the administrator of the plan, respectively, shall notify the individual of his or her rights under this section, and of the obligations of issuers of Medicare supplement policies under subdivision (a). The notice shall be communicated within 10 working days of the date the issuer received notification of disenrollment.
(g) An issuer shall refund any unearned premium that an insured paid in advance and shall terminate coverage upon the request of an insured.
(Amended by Stats. 2012, Ch. 162, Sec. 113. Effective January 1, 2013.)
#Medicare10050 and You 2024
Everything you want to know
- Steve's Video Seminar Introduction to Medicare & You
- Audio from Medicare.Gov
- Clear View to Medicare Patient Advocate.org - 36 pages
***********
- Your Medicare #Benefits # 10116
- Audio MP 3
- Inpatient ONLY - How Medicare Pays for your Surgery Part A vs Part B Very Well Health.com
- medicare.gov/coverage
- What's Covered App for Smartphones
- Medicare Coverage Database Search
- medicare.gov/procedure-price-lookup
- MLN Items & Services Not Covered Under Medicare
- An Overview-05-19-23 CA Health Care Advocates Hi Cap
- Original Medicare: An Overview CA Health Care Advocates Hi Cap
- 2024 Premiums, Coinsurance & Deductibles – 10-19-23 CA Health Care Advocates Hi Cap
- Supplementing Medicare: An Overview 10-30-20 CA Health Care Advocates Hi Cap
- Enroll in Blue Cross
- Learn about UHC United Health Care
- Enroll in Blue Shield
- SCAN
- Use our scheduler to Set a phone, Skype or Face to Face meeting
- #Intake Form - We can better prepare for the meeting (National Contracting Center)
- TITLE XVIII—HEALTH INSURANCE FOR THE AGED - Medicare AND DISABLE
-
- Welcome to Medicare 2022 Publication # 11095
- Our webpage on Enrolling ONLINE for Medicare Part A Hospital & B Doctor Visits
- Part A Hospital rules for zero premium
- Part B – Doctors – How to sign up – Benefits
- How to apply for Part B when you lose employer coverage - during your special enrollment period # 10012
- Fact Sheet Deciding Whether to Enroll in Medicare Part A and Part B When You Turn 65 CMS.gov 15 pages
- Medicare & You: Deciding to Sign Up for Medicare Part B VIDEO
- CMS form to fill out L 564 E to prove you had Employer Coverage and get a special enrollment period, when you retire. VIDEO
- HI CAP CA Health Care Advocates Medicare Enrollment Periods
FAQ's from Medicare.Gov
#Should I get Parts A & B?
Most people should enroll in Medicare Part A (Hospital Insurance) when they're first eligible, but certain people may choose to delay Medicare Part B (Medical Insurance). In most cases, #How
It depends on the type of health coverage you may have.
- Deciding to Sign Up for Medicare Part B VIDEO
- You must pay your Part B premium every month for as long as you have Part B (even if you don’t use it).
- If I'm low income - are there any breaks?
- Interactive Q & A from IRS on when to sign up for Medicare
- I have coverage through my spouse who is currently working.
- I have retiree coverage (from my former employer or my spouse’s former employer) or COBRA coverage.
- I have TRICARE, and I'm a retired service member.
- I have TRICARE, and I'm an active-duty service member.
- I have CHAMPVA.
- I have End-Stage Renal Disease (ESRD).
- I have Marketplace Covered CA or other private insurance.
- I don't have any of these.
- medicare.gov/should-i-get-parts-a-b
- How to apply for Part B during your special enrollment period # 10012
- Fact Sheet Deciding Whether to Enroll in Medicare Part A and Part B When You Turn 65 15 pages
- FAQ's that we did




Humana was my supplementary insurance [Medi Gap]
I have Medicare part A and B- I received a letter from Humana last week stating that are no longer providing the plan I had with them. I’m in Iowa.
I still have my drug coverage with them however. I need to find a new supplemental insurance
We don’t handle Iowa, but can give you some direction.
Here’s how to use Medicare.Gov’s plan finder
Assuming Zip Code 50301 Des Moines Here’s a list of Insurance Companies offering plans:
Guide to Medi Gap
Find an agent outside CA
Here’s Our Research Check out these references:
Official Guide to Medi Gap Page 3, right to buy Medi Gap policy and page 4 ESRD and Employer Coverage
ca health advocates.org
shrm.org