What is Part A Hospital & Part B MD Visits
How does it work, what is covered?
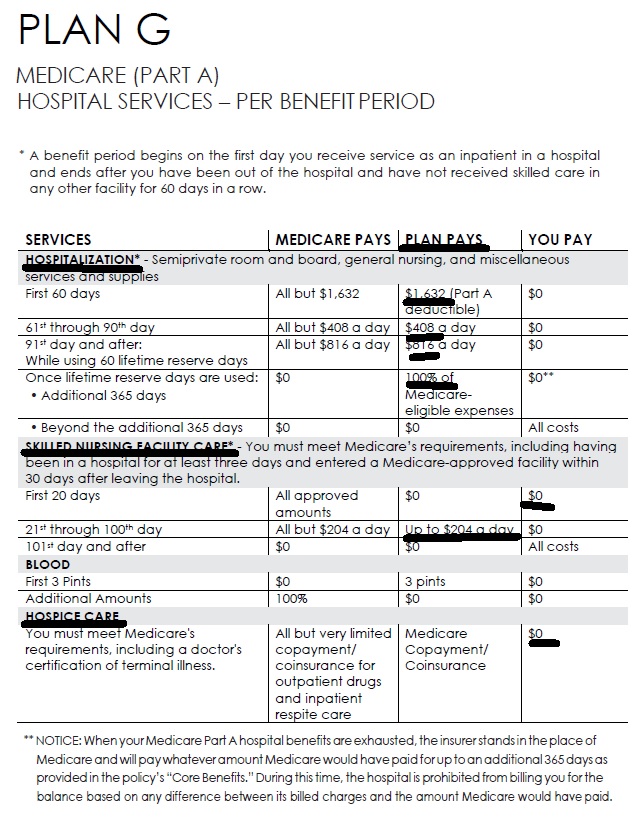
Medicare Part A
(#Hospital Insurance)
Medicare Part A Hospital coverage helps pay for care in hospitals as an inpatient,... skilled nursing facilities, hospice care, and some home health care (see publication # 10969) but not Long Term Care.
Most people get Part A automatically when they turn age 65 at no charge, since they or a spouse paid Medicare taxes while they were working. You need to sign up close to your 65th birthday, even if you will not be retired by that time. (If you are getting Social Security benefits when you turn 65, your Medicare Hospital Benefits - Part A - start automatically.)
Here's a chart it's just a illustration and is NOT official that shows what Medicare pays, the gaps in Medicare and what you may get when you add a Medi Gap Plan or Medicare Advantage to cover those gaps
-
See full brochure I cut and pasted this from
-
Pays on top of Medicare Parts A & B – Any Medicare Provider
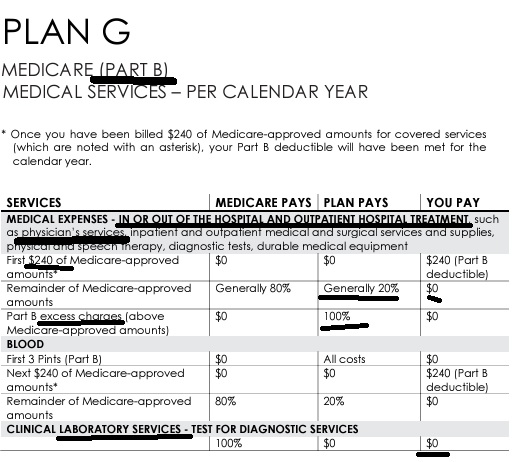
Part B - Outpatient helps Pay For Doctors' services, outpatient hospital care, and some other medical services that Part A does not cover, such as the services of physical and occupational therapists, and some home health care see publication 10969, but not Long Term Care. Part B helps pay for these covered services and supplies when they are medically necessary.
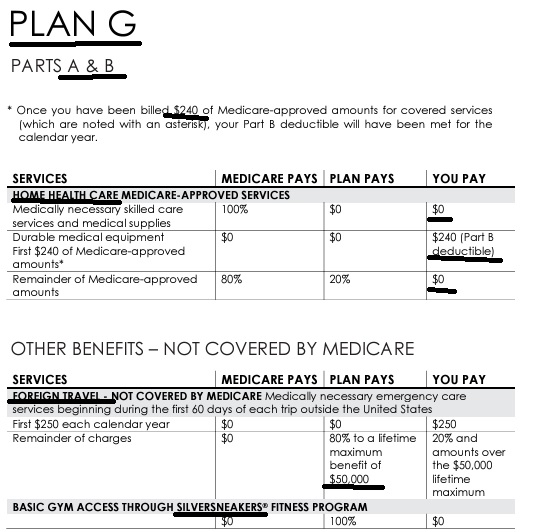
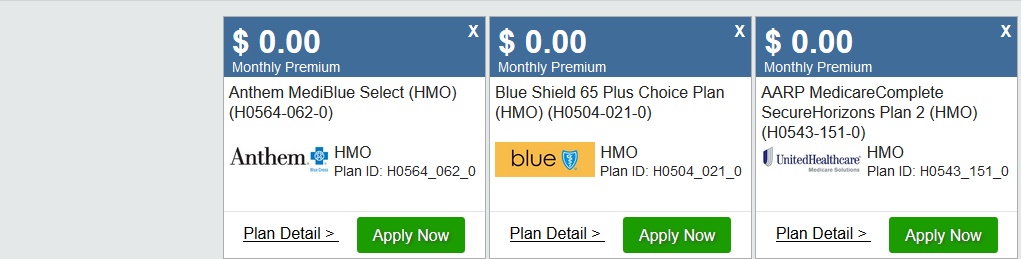
The chart below is a very brief summary. Check the actual Evidence of Coverage for the plan you want to enroll in, Medicare & You or actual Medicare documents.
2024 Fact Sheet Medicare Costs
Our Webpages with more detail:
- Coverage in Part A Hospital & B Doctor Visits? Part D Rx
- Chiropractic – Medicare A & B – MAPD
- Diabetes – Prevention & Coverage under Medicare & ACA
- Durable Medical Equipment
- End Stage Renal – Kidney Failure
- Hearing Aids
- Physical therapy – occupational speech
- Skilled Nursing SNF & Home Health What Medicare Pays
- Togetherness – Loneliness Social Determinants of Health
- Mental Health
- How to sign up for Medicare?
- FAQ Medical Necessity our Medical Necessity Webpage
- Original Medicare & Medi-Gap – Supplement vs Medicare Advantage MAPD
- Medicare Beneficiaries’ Out-of-Pocket Spending for Health Care AARP
#Medicare10050 and You 2024
Everything you want to know
- Steve's Video Seminar Introduction to Medicare & You
- Audio from Medicare.Gov
- Clear View to Medicare Patient Advocate.org - 36 pages
***********
- Your Medicare #Benefits # 10116
- Audio MP 3
- Inpatient ONLY - How Medicare Pays for your Surgery Part A vs Part B Very Well Health.com
- medicare.gov/coverage
- What's Covered App for Smartphones
- Medicare Coverage Database Search
- medicare.gov/procedure-price-lookup
- MLN Items & Services Not Covered Under Medicare
- An Overview-05-19-23 CA Health Care Advocates Hi Cap
- Original Medicare: An Overview CA Health Care Advocates Hi Cap
- 2024 Premiums, Coinsurance & Deductibles – 10-19-23 CA Health Care Advocates Hi Cap
- Supplementing Medicare: An Overview 10-30-20 CA Health Care Advocates Hi Cap
- Enroll in Blue Cross
- Learn about UHC United Health Care
- Enroll in Blue Shield
- SCAN
- Use our scheduler to Set a phone, Skype or Face to Face meeting
- #Intake Form - We can better prepare for the meeting (National Contracting Center)
- TITLE XVIII—HEALTH INSURANCE FOR THE AGED - Medicare AND DISABLE
-
- Welcome to Medicare 2022 Publication # 11095
- Our webpage on Enrolling ONLINE for Medicare Part A Hospital & B Doctor Visits
- Part A Hospital rules for zero premium
- Part B – Doctors – How to sign up – Benefits
- How to apply for Part B when you lose employer coverage - during your special enrollment period # 10012
- Fact Sheet Deciding Whether to Enroll in Medicare Part A and Part B When You Turn 65 CMS.gov 15 pages
- Medicare & You: Deciding to Sign Up for Medicare Part B VIDEO
- CMS form to fill out L 564 E to prove you had Employer Coverage and get a special enrollment period, when you retire. VIDEO
- HI CAP CA Health Care Advocates Medicare Enrollment Periods
FAQ's from Medicare.Gov
#Should I get Parts A & B?
Most people should enroll in Medicare Part A (Hospital Insurance) when they're first eligible, but certain people may choose to delay Medicare Part B (Medical Insurance). In most cases, #How
It depends on the type of health coverage you may have.
- Deciding to Sign Up for Medicare Part B VIDEO
- You must pay your Part B premium every month for as long as you have Part B (even if you don’t use it).
- If I'm low income - are there any breaks?
- Interactive Q & A from IRS on when to sign up for Medicare
- I have coverage through my spouse who is currently working.
- I have retiree coverage (from my former employer or my spouse’s former employer) or COBRA coverage.
- I have TRICARE, and I'm a retired service member.
- I have TRICARE, and I'm an active-duty service member.
- I have CHAMPVA.
- I have End-Stage Renal Disease (ESRD).
- I have Marketplace Covered CA or other private insurance.
- I don't have any of these.
- medicare.gov/should-i-get-parts-a-b
- How to apply for Part B during your special enrollment period # 10012
- Fact Sheet Deciding Whether to Enroll in Medicare Part A and Part B When You Turn 65 15 pages
- FAQ's that we did
#Durable1 medical equipment (DME)
Medicare covers items like oxygen equipment and supplies, wheelchairs, walkers, and hospital beds ordered by a doctor or other health care provider enrolled in Medicare for use in the home. Some items must be rented. You pay 20% of the Medicare-approved amount, and the Part B deductible applies. If you have a Medi Gap plan, that should pay the 20%! Medicare Advantage, check the summary of benefits or EOC Evidence of Coverage.
Make sure your doctors and DME suppliers are enrolled in Medicare. Doctors and suppliers have to meet strict standards to enroll and stay enrolled in Medicare. If your doctors or suppliers aren’t enrolled, Medicare won’t pay the claims they submit. It’s also important to ask your suppliers if they participate in Medicare before you get DME. If suppliers are participating suppliers, they must accept assignment (that is, they’re limited to charging you only coinsurance and the Part B deductible for the Medicare-approved amount). If suppliers aren’t participating and don’t accept assignment, there’s no limit on the amount they can charge you.
To find suppliers who accept assignment, visit Medicare.gov/supplier directory or call 1-800-MEDICARE (1-800-633-4227). TTY users can call 1-877-486-2048. You can also call 1-800-MEDICARE if you’re having problems with your DME supplier, or you need to file a complaint. Copied from Medicare & You – see link in side panel
What about Stair Lifts?
- acorn stair lifts.com
- Medical Necessity of Stair Lifts & Lifting devices Clinical Bulletin?
- Durable Medical Equipment
- Seat Life Mechanisms
- Do Condominiums have to provide stair lifts, under ADA?
- Pride Mobility.com Steps to get Medicare to pay
- Law Dictionary.com Does Insurance Cover Stair Lift?
- hhs.gov research 1989
Guide Dog or Other Service Animal
You can include in medical expenses [but apparently not as durable medical expense] the costs of buying, training, and maintaining a guide dog or other service animal to assist a visually impaired or hearing disabled person, or a person with other physical disabilities. In general, this includes any costs, such as food, grooming, and veterinary care, incurred in maintaining the health and vitality of the service animal so that it may perform its duties. irs.gov/
- Maybe you can get a grant?
Resources & Links
- CMS discontinues medical device forms to ease physician administrative burdens Fierce Health Care * Rev Cycle Intelligence *
- Biden repeals Trump rule that expedited coverage for “breakthrough technology” Modern Health Care * 9.13.2021 prior article * Federal Register 42 CFR Part 405 [CMS-3372-P2] RIN 0938-AT88 *
- Wheelchair users can face hefty costs not covered by insurance, under age 65… LA Times 11.15.2021 *
- Coverage for catheters?
- wikipedia.org/Certificate_of_medical_necessity
What does Medicare cover for
#Durable Medical Equipment, wheel chairs, stair lifts etc # 11045
Medicare Coverage – #Ambulance # 11021
Resources & Links
- forbes.com/insurance-for-ambulance-rides/
- New California Law Offers Fresh Protection From Steep Ambulance Bills KFF.org – no balance billing – out of network
FAQ’s
- Question: Non-emergency ambulance transportation
- Answer You may be able to get non-emergency ambulance transportation if you need it to treat or diagnose your health condition and the use of any other transportation method could endanger your health — Get the details on page 6 of the above publication, even MORE details Medicare Benefit Policy Manual Chapter 10 – Ambulance Services
#Chiropractic coverage in Medicare
VIDEO explanation Chiropractic
Here’s how Medicare A & B and the a Typical MAPD Plan. and Medi Gap would pay the 20% that Medicare allows, but leaves as a co payment.
Medicare Part B pays 80% for spinal manipulation if medically necessary. Thus, Medi Gap and Medicare Advantage only pay, if Medicare does.
Medicare doesn’t cover other services or tests ordered by a chiropractor, including X-rays, massage therapy, and acupuncture. If you think your chiropractor is billing Medicare for chiropractic services that aren’t covered, you can report suspected Medicare fraud Medicare.gov *
Medical Necessity get’s quite complicated.
Here’s more detailed definitions:
Here’s a Medicare Fact Sheet, something a little easier to read for the lay person.
For chiropractic services, medically necessary means the patient must have “a significant health problem in the form of a neuromusculoskeletal condition necessitating treatment, and the manipulative services rendered must have a direct, therapeutic relationship to the patient’s condition and provide a reasonable expectation of recovery or improvement of function. The patient must have a subluxation of the spine, as demonstrated by x-ray or physical exam.”
Treatment by means of manual manipulation of the spine to correct a subluxation (incomplete or partial dislocation of a joint or organ.[1] Wikipedia ) (that is, by use of the hands).
Patient must require treatment by means of manual manipulation.
Manipulation services rendered must have direct therapeutic relationship to the patient’s condition.
There must be a reasonable expectation of recovery or improvement of function resulting from the planned treatment. CMS.gov *
Medicare Exclusions from Coverage
Note that the specimen Medicare Advantage policy we used to analyze coverage has exclusions on page 115 for chiropractic, they only cover what Medicare covers, nothing extra!
For those of you who think that “Medicare for All” will be the solution to every health problem and that Medicare pays everything, take a look at this NINE page bulletin on the the Medicare records required from your chiropractor.
Sample Medicare Advantage Plan
Use Ctrl F & Search adobe.com/searching-pdfs
Sample Medi Gap EOC Plan G
Medi Gap will provide coverage for the coinsurance amount or, in the case of hospital outpatient Services, the copayment amount of Medicare Eligible Expenses under Part B …, subject to the Medicare Part B Deductible provided the Subscriber is receiving concurrent benefits from Medicare for the same Services. Blue Shield EOC *
Do #Health Care Reform compliant plans cover chiropractic?
No, Chiropractic is Excluded on page 106 of the Specimen policy, Page 14 brochure It’s not an essential benefit, in CA
Here’s the CA Kaiser Benchmark Plan which is the “model” for ACA compliant plans
Other States may cover chiropractic, but CA doesn’t. Here’s a report from dynamic chiropractic.com
However,
Chiropractor benefits available for Silver 1950 PPO and Silver 2600 HDHP PPO plans as of Jan 1, 2021
We are the first off-exchange health plan to offer embedded chiropractic services to members through the American Specialty Health (ASH) network with Silver 1950 PPO and Silver 2600 HDHP PPO plans.
Benefits include:
$15 copayments for Silver 1950 PPO
35% coinsurance for Silver 2600 HDHP PPO
Both plans have an annual limit of 15 visits
At one time you could Buy your OWN Chiropractic Plan!
But Landmark Health Plan has discontinued selling for individuals. Employer Groups can still enroll.
#Understanding Medicare Advantage Plans (PDF) #12026
Insurance Companies get a fee from the Federal Government, when you enroll in an MAPD plan. MAPD Plans must cover all A & B services Medicare.Gov *
That's why the premium is very low or ZERO!
- Set a phone or Skype Meeting
- We can now do SOC Scope of Appointment, before the Meeting via a 3 minute recorded meeting 2 days before. AHIP Training Module 4 Page 14 *
- #Intake Form - We can better prepare for the meeting
- Medicare Advantage (Medicare Part C): An Overview Hi Cap
- HMO - Narrow Networks?
- HI Cap CA Health Care Advocates Fact Sheet
- Do I just sign up with a Medicare Advantage Company and automatically get * Parts A & B or do I have to get those from Medicare.Gov * VIDEO
- Get Quotes, Full Information and Enroll
- MANDATED wording!: Think Advisor * ‘‘We do not offer every plan available in your area. Any information we provide is limited to those plans we do offer in your area. Please contact Medicare.gov or 1–800–MEDICARE to get information on all of your options.’’
- We disagree with the above wording, as we can use the same tools on Medicare.gov as they do!
- FYI a 4.27.2022 HHS Office of the Inspector General report found that MAPD plans denied 13% of prior authorizations that would have been covered under original Medicare (Conversely, Medi Gap, just follows what Medicare pays.)
- 88% of MAPD enrollees are happy
-
MAPD plans often include Dental & Part D - Rx Prescriptions and often have NO premiums!
-
How is that possible?
-
The Federal Government pays them around $700/month to handle your medical care. You must continue to pay your Medicare Part B premium of about $170/month. It's best to apply when you turn 65 for the supplement plans or advantage plans, as that's the main "Open Enrollment" period, guaranteed issue for any plan.
-
-
-
Medicare Advantage Plans also have an annual open enrollment now known as AEP Annual Election Period October 7 to December 15th.
-
Additional Coverage is important as Medical Bills are increasing Seniors Credit Card Debt or leading to possible bankruptcy?
- If You Have Problems with Your Medicare Advantage Plan
- When Medicare Advantage Plans Terminate Coverage
- Medi-Cal D-SNP Feasibility Study
Medicare Coverage of #Cancer Treatment # 11931
- Our FAQ Cancer Experimental Rx
- Chemotherapy covered under Part B and not Part D Forbes *
- FAQ on cancer coverage in ACA/Obamacare plans
- Kaiser Health News - Cancer & Medical Debt
- Our webpage on Medical Necessity
- ESMO Clinical Practice Guideline for the diagnosis, staging and treatment of patients with metastatic breast cancer
- Chemotherapy (Medicare.Gov)
- Mammograms
- Comparison of Treatment Costs for Breast Cancer, by Tumor Stage and Type of Service
- Cancer Care.org
- How Cancer Treatment Is Improving for People Living in Rural Areas Healthline.com 5.19.2022
- Medicare Dental Care
- Why Are So Many Young People Getting Cancer? It’s Complicated Time.com
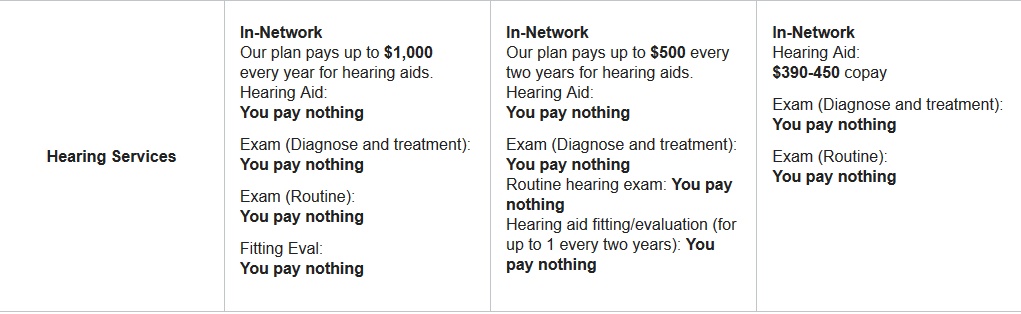
#Hearing & balance exams & hearing aids
How often is it covered?
- Medicare Part B (Medical Insurance) covers diagnostic hearing and balance exams if your doctor or other health care provider orders these tests to see if you need medical treatment. medicare.gov/hearing-balance-exams * medicare.gov/hearing-aids *
- Medicare doesn’t cover hearing exams, hearing aids, or exams for fitting hearing aids.
- Say That Again: Using Hearing Aids Can Be Frustrating for Older Adults, but Necessary
Who’s eligible?
Your costs in Original Medicare
- You pay 100% for exams and hearing aids.
- You pay 20% of the Medicare-approved amount for the doctor’s services for covered exams, and the Part B deductible applies.
- In a hospital outpatient setting, you also pay the hospital a copayment. Source Publication 10116 Your Medicare Benefits * Medicare.Gov
Medicare Advantage Plans might cover Hearing Aids
- Oscar Clinical Guideline
- Kaiser Health News – Hearing Aids can be purchased without a prescription
-
- npr.org/what-to-know-now-that-hearing-aids-are-available-over-the-counter
- How to choose the right one Mayo Clinic
- Buying Hearing Aids On Your Own ASHA American Speech Language Assoc.
- hearing care solutions.com/
- California Hearing Center
- FDA finalizes rule to make hearing aids available over the counter The Hill * KHN
- The FDA says you can get hearing aids without a prescription. Here’s how LA Times
- The FDA got it right with hearing aids. Updating Medicare coverage is next
- Rule in Federal Register 8.17.2022
- Our webpages on:
- Health Savings Accounts HSA?
- Medi Cal coverage
- Medi-Cal covers hearing aids when supplied by a hearing aid dispenser on the prescription of an otolaryngologist, or the attending physician ‹‹(in consultation with the evaluating otolaryngologist, if possible)›› when no otolaryngologist is available in the community. An audiological evaluation, including a hearing aid evaluation performed by, or under the supervision of, the above prescribing physician, or by a licensed audiologist, is required. Source *
- Hearing Aid FAQ’s
- Hearing Loss.org
- Does ACA/Obamacare cover hearing aids?
-
-
At this time, there is no Federal coverage for hearing aids under Medicare, Medicaid, or any mandate that requires private insurers to provide hearing aid coverage.
-
#Cochlear Implants
A cochlear implant is a small electronic device that can help “make” sound if you have severe or total hearing loss. The implant does the job of the damaged or absent nerve cells that in a normal ear make it possible to hear (auditory nerves). Cochlear implants can be programmed according to your specific needs and degree of hearing loss. Web MD
Will an implant be covered on your Medical Insurance?
- Aetna’s Bulletin on Cochlear Implants, includes billing codes.
- NO MORE! Pre-Existing Condition Clause
- Is the implant Medically Necessary
- Guaranteed Issue ACA/Obamacare for Individuals & Employer Groups – AB 1672
Consumer Resources
#MedicareRelated Pages
- Medicare – Introduction – Part A Hospital – B Outpatient – D Rx Medi Gap & MAPD
- Coverage in Part A Hospital & B Doctor Visits? Part D Rx
- Enroll ONLINE for Medicare Part A Hospital & B Doctor Visits
- Medi Gap – Supplement Plans – non conical
- Medicare Advantage Plans – Part C
- Part D Rx Prescriptions no index
#Physical therapy/occupational therapy/speech-language pathology services
- Medicare Part B (Medical Insurance) helps pay for medically necessary, see clinical guidelines!,
- outpatient physical medicare.gov/physical-therapy
- and Occupational therapy
- and. Speech-language pathology services
- Your medical record must include information to explain why the services are medically necessary
A Medicare contractor like Livanta may review your medical records to be sure your therapy services were medically necessary. This happens when your bills go over say $2k cms.gov/theraphy caps
Your therapist or therapy provider must give you a written notice before providing services that aren’t medically necessary. This includes therapy services that are generally covered but aren’t medically reasonable and necessary for you at the time. This notice is called an “Advance Beneficiary Notice of Noncoverage” (ABN). The ABN lets you choose whether or not you want the therapy services. If you choose to get the medically unnecessary services, you agree to pay for them.
Who’s eligible?
All people with Part B are covered as long as the services are medically reasonable and necessary.
Your costs in Original Medicare
You pay 20% of the Medicare-approved amount, and the Part B deductible applies. If you have a Medi Gap or Medicare Advantage plan, those will pay all or part of the 20%.
Resources & Links
- The Best Quadriceps Exercises to Build Stronger Thighs Very Well.com
- Your Medicare Benefits Page 91
- Medicare & Home Health Care Page 8
- kindred health care.com your-guide-to-medicare-and-transitional-care
- torrance memorial.org/transitional-care/
- cms.gov/transitional-care-management-services-fact-sheet

- medicare.gov/transitional-care-management-services
- 42 CFR § 410.60 – Outpatient physical therapy services: Conditions
- The complete Medicare guide for physical, occupational, and speech therapy.
- What does Medicare cover for outpatient rehabilitation therapy? Medicare Made Clear
- CMS.gov Physical Therapy – Home Health
- Claims for outpatient physical therapy services provided by Athletic did not comply with
Medicare requirements. Specifically, of the 100 beneficiary days in our random sample, Athletic
properly claimed Medicare reimbursement for 68 beneficiary days. However, Athletic
improperly claimed Medicare reimbursement for the remaining 32 beneficiary days, which had
therapy services that were not medically necessary. Read more oig.hhs.gov - medicare.gov/physical-therapy-services
#DROPPED HEAD SYNDROME
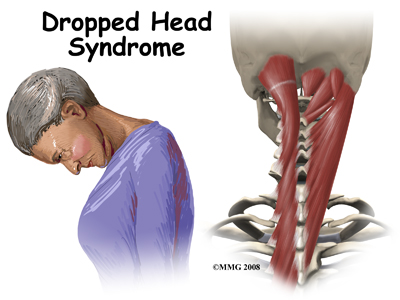
One of the extra things we do for our clients, friends & web visitors who post questions in the comments below, is extensive internet research. Here we go…
In addition to the physical therapy benefit in Medicare, Employer Group or Individual & Family plans, how about doing physical therapy at home, the gym and using silver sneakers?
- humpal physical therapy.com/Dropped-Head-Syndrome photo credit too
- spine-health.com/easy-chest-stretches-neck-pain
- mayfield clinic.com/neck stretches & strengthening
- Impact physical therapy
- Caring Medical.com
Brother - Sister - Sibling Side Pages Subpages
View our website with your Desktop or Tablet for the most information





https://www.forbes.com/health/hearing-aids/hearing-aids-insurance-coverage/
https://www.asha.org/advocacy/state/state-insurance-mandates-for-hearing-aids/
https://khn.org/morning-breakout/watchdog-finds-that-gaps-in-cms-oversight-cost-medicare-part-b-millions/
https://www.commonwealthfund.org/publications/newsletter-article/hospital-home-programs-improve-outcomes-lower-costs-face-resistance
https://www.nbcnews.com/health/health-news/highly-processed-food-linked-faster-cognitive-decline-rcna40999
https://www.sfchronicle.com/bayarea/article/California-pays-less-than-almost-every-state-for-17021716.php
https://apnews.com/article/health-xavier-becerra-medicare-government-and-politics-2ae8ccf461192e337d744bd5981fc192
https://www.statnews.com/2022/05/27/biden-administration-wont-lower-medicare-premiums-aduhelm/
https://healthpayerintelligence.com/news/how-medicare-out-of-pocket-healthcare-spending-cap-may-impact-beneficiaries
Will Medicare cover testing for Corona Virus?
Yes, under Part B. See Medicare.Gov for more details Maybe when the pandemic is over, NO?
Medicare Advantage Plans are mandated to cover A & B, so it will be covered by those too.
Medi Gap plans will pay the 20% co pay that Medicare doesn’t pay.
Coronavirus testing looks for signs of a coronavirus infection in nasal secretions, blood, or other body fluids. Coronaviruses are types of viruses that infect the respiratory system. They are found in both animals and people. Coronavirus infections in people are common throughout the world. They don’t usually cause serious illness.
Sometimes a coronavirus that infects animals will change and turn into a new coronavirus that can infect people. These coronaviruses can be more serious and sometimes lead to pneumonia. Pneumonia is a life-threatening condition in which fluid builds up in the lungs.
Three of these new coronaviruses have been discovered in recent years:
SARS (severe acute respiratory syndrome), a serious and sometimes fatal respiratory illness. It was first discovered in China in 2002 and spread around the world. An international effort helped quickly contain the spread of disease. There have been no new cases reported anywhere in world since 2004.
MERS (Middle East respiratory syndrome), a severe respiratory illness discovered in Saudi Arabia in 2012. The illness has spread to 27 countries. Only two cases have been reported in the United States. All cases have been linked to travel or residence in or around the Arabian Peninsula.
COVID-19 (coronavirus disease 2019). It was discovered in late 2019 in Wuhan City, in the Hubei Province of China. Most infections have occurred in China or are related to travel from Hubei Province. There have been some cases reported in United States. The outbreak is being closely monitored by the Centers for Disease Control (CDC) and the World Health Organization (WHO).
See our main page on Corona Virus and Insurance Coverage – Including Government Benefits
If I stay overnight in a hospital, doesn’t that make me an inpatient, so that I can then qualify for Skilled Nursing care, etc?
Am I an inpatient or outpatient?
Staying overnight in a hospital doesn’t always mean you’re an inpatient. Your doctor must order your hospital admission and the hospital must formally admit you for you to be inpatient. Without the formal inpatient admission, you’re still an outpatient, even if you stay overnight in a regular hospital bed, and/or you’re getting emergency department services, observation services, outpatient surgery, lab tests, or X-rays. You or a family member should always ask the hospital and/or your doctor if you’re an inpatient or an outpatient each day during your stay, since it affects what you pay and can affect whether you’ll qualify for Part A coverage in a skilled nursing facility.
A “Medicare Outpatient Observation Notice” (MOON) is a document that lets you know you’re an outpatient in a hospital or critical access hospital. You must receive this notice if you’re getting observation services as an outpatient for more than 24 hours. The MOON will tell you why you’re an outpatient receiving observation services, rather than an inpatient. It will also let you know how this may affect what you pay while in the hospital, and for care you get after leaving the hospital. Citation Medicare & You 10050 or Medicare Benefits 10116 See links above
Is the part b premium tax deductible?
Not that I’m aware of. Please check with competent tax or legal counsel. Here’s some links and information I do have.
Self Employed – Line 29 deduction of health Insurance Premiums
Savings from an HSA – Health Savings Account can be used to pay premiums – double check the rules and citations on our HSA webpage. See Publication 502 Medical & Dental Expenses
See the Kaiser Foundation Report on Part D & B premiums vs spending.