Medi Cal based on income below 138% of Federal Poverty Level
Medi Cal Qualification under MAGI Income
- For most individuals, Medi-Cal eligibility will be #based on your household size and your Federal MAGI – Income. Dhcs.gov * My Medi Cal * Western Poverty Law * If you have less than 138% of Federal Poverty Level, for children 266%, that’s it.
- Medi Cal eligibility under Health Care Reform expanded is when you have family household income (MAGI) under 138% of Federal Poverty Level (subsidy income chart for ObamaCare) dhcs.gov for the parents and 266% for children and no more asset or means testing, there is no more estate recovery for health insurance.
- If your children qualify for Medi Cal, and the parents for Covered CA – Private Insurance with subsidies you can now apply for both using the Covered CA online application Cbp.org page 65, with us as your agent at no additional charge, just follow these instructions, starting with find help in the upper right hand corner if you fill out the Covered CA application ONLINE, yourself.
- If you are not applying for a subsidized private plan with us as your agent, no charge through Covered CA the easiest and fastest way to apply for or renew Medi-Cal is:
- Directly though your local county human service agency CA State wide listing
- Benefits Cal.org for all Welfare Benefits…
- Please note that we can no longer do extensive research on Medi Cal questions as we are not authorized representatives for Medi Cal, nor do we get compensated one nickel for this website or our time. Please contact Medi Cal or your Medi Cal HMO directly. We will do research and education for a fee.
- Assets are no longer counted! VIDEO * Western Poverty Law Page 24 *
- Covered CA Income and FPL Federal Poverty Level Chart
- Covered CA Medi-Cal Overview
- Medi Cal Maze, why many people don’t enroll CHCF 9/13/2021
- There are nominal premiums for children if you’re at more than 160% of FPL DHCS *
What’s on this page?
- Medi Cal Brochure
- Medi Cal Expansion to 138% of Federal Poverty Level
- Detailed explanation & rules from Western Poverty Law
- Mandate to report changes
- Monthly income qualification
- Free Tax Help
- Code of Federal Regulations
- When does Medi Cal coverage start?
- Annual Redetermination
- Out of state emergency rules
Benefits
Medical
Dental
#My Medi-Cal
How to get the Health Care
You Need
24 pages
Smart Phones - try turning sideways to view pdf better
-
- More explanation

- Enroll with Benefits Cal
- What is Medi Cal - VIDEO
-
How to VIDEO
-
Medi-Cal Managed Care HMO – Health Care Options
- Benefits Cal is a one-stop-shop to apply for...
- Cal Fresh
- Ages 26 through 49 Adult Full Scope Medi-Cal Expansion regardless of immigration status
- Cal WORKs
- Medi-Cal
- CMSP (County Medical Services Program)
- Disaster Cal Fresh
- GA/GR (General Assistance and General Relief )
- Briefing — Medi-Cal Explained: An Overview of Program Basics
- chcf.org/medi-cal-explained/
- #BenefitsCal is a one-stop-shop to apply for...
- Medi-Cal
- County Medical Services Program (CMSP),
- Food Assistance - Cal Fresh (formerly known as Food Stamps)
- How to use Eat Fresh.org VIDEO
- Cooking & Nutrition
- California Work Opportunity and Responsibility to Kids (CalWORKs) or check their other website
- Medi-Cal
-
Here you can review and choose the HMO that you want to deliver your Medi-Cal health Care.
-
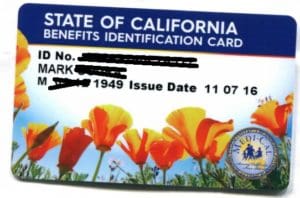
BIC Benefits Identification Card
Improvements?
Trump, whatever less coverage
2025 Possible Increases or decreases in Funding and Coverage
- How Trump Administration Cuts Could Hurt Medi-Cal
Federal funds cover more than 60% of California’s low-income health insurance plan. Losing even part of that money could result in cutbacks on care for kids or state tax hikes. Read more * - California OKs $2.8B to close Medicaid funding gap after expanding immigrant coverage Read More *
- A fifth of Americans are on Medicaid. Some of them have no idea.
Programs with consumer-friendly names and private insurance company involvement add to the confusion. Read More * - Defending Medi Cal in 2025 CHCF *
- Medi-Cal Waivers and State Plan Amendments Chcf *
IHSS Cal AIM Waivers
- This series of short explainers outlines the overlaps and gaps between three Medi-Cal Home and Community-Based Services programs and CalAIM Community Supports. The three explainers focus on:
- Assisted Living Waiver
Home and Community-Based Alternatives Waiver
California Community Transitions Read More *
- Assisted Living Waiver
FAQ’s
When does coverage #start?
- I applied for Medi-Cal but have not received any information from the county
- Medi-Cal will pay medical bills for 3 months prior to acceptance into medi-cal, but one must ask for retroactive coverage Western Poverty Law Center Page 5.211. * Excerpt of email from [email protected]
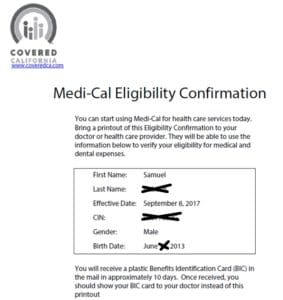
- Note that you can get immediate confirmation of provisional Medi-Cal enrollment when you apply direct or through an agent – at no additional charge on Covered CA’s website. If you scroll down on the eligibility page and find it.
- Scroll down for Other ways to get immediate medical care and more proof that you have coverage while waiting for your ID cards.
Documentation Required during
Covered CA 90 Day #Conditional Eligibility
A 90 day conditional eligibility notice means that you get coverage for 90 days even though Covered CA hasn’t verified that you qualify. As long as you send the proofs that are being asked for, everything is fine! There is NOTHING to worry about! Just comply. If you have trouble with compliance, email us.
Clients need to submit valid documentation for one or more of the following reasons:
- U.S. Citizen/National or non-citizen with a lawfully present status
- Income (MAGI Line 37*) Insure Me Kevin.com 2.19.2016
- Social Security Number (SSN)
- Incarceration Status – Insure Me Kevin.com
- American Indian/Alaska Native Status
You can upload, fax, send to their Certified Agent or mail their documentation. More than one document may be required.
View our Conditional Eligibility Quick Guide * or Job Aid for more information on the notice and to view a list of acceptable Verification Documentation.
Look for this sentence in the letter that you get from Covered CA.
We need your proof within 90 days. If we get a response and you prove your citizenship by the due date above, you will keep your insurance through Covered California.
Here’s the biggest lesson I learned in one year of law school. Read everything 3 times and when you think you understand it, read it again.
Resources & Links
- Medi-Cal’s website for Pending Applications & Newly Enrolled
- More Information – Covered CA Start Date – Conditional Eligibility
Immediate & Retroactive Medi Cal Coverage
more proofs
If you have already applied, you do not need to apply again. Medi-Cal is processing your application as quickly as possible. Due to the large number of Medi-Cal applications received, processing is taking longer than expected, and proof of certain information is required in order to complete each application. Covered CA.com *
DHCS – Medi Cal Website
Pending Applicants
- For those who applied and
- are likely [: having a high probability of occurring or being true : very probable – rain is likely today Webster * ]
- eligible, [qualified to participate or be chosen – eligible to retire Webster * ]
- See our webpage on mandate for Government to write in plain English.
-
Contra proferentem is a rule of contract interpretation that states an ambiguous contract term should be construed against the drafter of the contract. The term contra proferentem is derived from a Latin phrase meaning “against the offeror.”
Contra proferentem has become increasingly important with the rise of contracts of adhesion. Contracts of adhesion involve pre-written contracts which are offered on a strict take-it or leave-it basis, leaving no opportunity for a party to bargain over specific contractual terms. Because the party does not have an opportunity to negotiate, they may reasonably interpret a term in a different manner than the contract offeror intended. Contra proferentem exists to place the burden of ambiguity on the party most capable of mitigating that ambiguity – the person who wrote it.
The doctrine of contra proferentem is also especially important in the field of insurance law due to the generalized nature of many of its terms. For example, it may be unclear if a policy that covers “water damage” will cover damage caused by a rainstorm induced mudslide. The doctrine of contra proferentem encouraged insurance providers to create enumerated lists of events that are excluded under a given policy, ultimately increasing clarity for insurance purchasers. Source Cornell Law *
-
- See our webpage on mandate for Government to write in plain English.
-
but are waiting for their application to be finalized, there are ways you can get immediate care while you wait:
-
-
- You can go to a hospital for emergencies. The Hospital Presumptive Eligibility (PE) program provides adults, pregnant individuals, children, and former foster care enrollees with temporary, no cost Medi-Cal benefits for up to two months. In order to receive Hospital PE benefits, you must complete a simplified application online during a hospital stay. You will be notified immediately of your eligibility determination.
- You can visit your local county human services office. You can use your information to confirm your Medi-Cal eligibility and get a temporary identification card. This will allow you to get services until your enrollment is complete.
- Pregnant individuals can get temporary Medi-Cal coverage from certain Medi-Cal providers and clinics.
- Children can get temporary Medi-Cal coverage provided by enrolled Medi-Cal providers and clinics that see children.
-
Once your Medi-Cal eligibility is confirmed, the health coverage is effective beginning the first day of the month when you applied.
If you would like more information or to check the status of your application, please contact your county human services agency. Source DHCS.CA.Gov *
Western Poverty Law
An applicant can receive Medi-Cal coverage (and payment for Medi-Cal covered benefits received) for up to three calendar months preceding the month of application if they would have been eligible for Medi-Cal during those months. 148
Applicants can apply for retroactive Medi-Cal on the Medi-Cal application or after applying for Medi-Cal or CalWORKs by indicating the request on the application or by separate written request.149
Retroactive Medi-Cal can be requested for up to one year after the date of application150 so if there are outstanding bills, the Medi-Cal member should submit them to Medi-Cal for reimbursement or ask the provider to bill Medi-Cal.
Footnotes
147. Welf. & Inst. Code §§ 14017.7, 14017.8. Note that an individual is only sent a BIC if one has not been issued to that person previously. If the person was previously assigned a BIC, it is re-activated. If the beneficiary needs to request a new card, they can contact the county. Additionally, beneficiaries can request a paper BIC from the county so they do not have to wait for the plastic card to arrive in the mail if they have an urgent need.
148. Welf. & Inst. Code §§ 14019, 14019.6; 22 CCR § 50197; MEDIL 14-27 (May 15, 2014),
149. 22 CCR § 50148(a)(2). 150. 22 CCR § 50148(b). Source Western Poverty Law Page 5.211 *
Email from at Chief at Medi Cal
Hello Mr.
Thank you for your email, and apologies for the delay in responding.
Due to the large number of Medi-Cal applications received through the Covered California website, it is taking longer than expected to verify all of the applications. Once an application is found likely eligible for Medi-Cal, it is sent to the applicant’s county of residence for processing. You and/or the applicant do not need to submit another application to the county if one has already been submitted. A tax penalty will NOT affect those who applied by the deadline and are waiting on an eligibility determination.
If the individuals you’re assisting would like more information about their applications and eligibility statuses, you or they can contact the applicant’s county human services agency
Please remember that in the event of an emergency where medical care is needed, individuals should call 9-1-1 or go to their nearest hospital. Medi-Cal will cover costs associated with services rendered while their application is pending.
Thank you for your patience.
Crystal Crystal M. Haswell,
Chief Outreach and Enrollment Unit
Medi-Cal Eligibility Division California Department of Health Care Services
Emails Rec’d from actual client
6.2.2023
Hi Steve,
Thanks for all the work you have put into this. [redacted] called the County level medi-cal this afternoon to ask about eligibility and inquiring about [redacted] SSN. It was an hour wait but we got to talk to someone.
They confirmed that they have her correct SSN and that [redacted] is covered with temporary Medi-cal coverage until they finish processing her application. So that’s a relief. Once they’re done, we’ll get notified with whether she will be on medi-cal or a covered california plan.
We have case numbers and her temp medi-cal number so we can get updates if we don’t hear back. I think we are good to go regarding [redacted]’s coverage. Thanks again for your help in this.
[redacted]
Ditto for what [my wife] said!!
THANK YOU STEVE for all of you hard work!!!!
[redacted]
#Redetermination when Pandemic Ends
Medi-cal [Medicaid nationally] has not disenrolled anyone for say the past year and a half due to the COVID 19 pandemic. When the pandemic emergency is declared over it’s estimated that millions will lose coverage. Those whose incomes are over 138% of Federal Poverty level can get Covered CA, FREE QUOTES.
Learn More ==> Our webpage on Redetermination
Medi-Cal Managed Care HMO – Health Care Options
Here you can review and choose the HMO that you want to deliver your Medi-Cal health Care.
Learn more:
- Disability Rights.org –
- What are Medi Cal Managed Care Plans? What do I need to know?
- Medi-Cal Managed Care Health Plan Directory
- Medi-Cal Listing of HMO plans by county *
- Medi-Cal Managed Care Provider Search
- Medi Cal HMO – Managed Care Providers by County
- health care options.dhcs.ca.gov/tips-help-you-choose-medical-plan
- health care options.dhcs.ca.gov/frequently-asked-questions-faqs
- California’s County-Based Health Plans 2022 CHCF
- Medi-Cal’s Fragmented System Can Make Moving a Nightmare Read More CA Health Line *
- Poor Care Co-Ordination? New contracting process Deficient Oversight CA Health Line *
- Disability Rights – Medi Cal provider HMO’s, what are they? What do I need to know about them?
- Medi-Cal Managed Care – Health Care Options
- EOC’s, Forms & Income Charts from Insure Me Kevin.com
- Sacramento? dhcs.ca.gov//mmcd health plan dir
- Battle Lines Are Drawn Over California Deal With Kaiser Permanente
- Exemption from enrolling in a Health Care Plan
- health care options.dhcs.ca.gov - Download Forms
- You May Get A Medical Exemption If:
- You have a complex medical condition; AND
- The care you get from your Regular Medi-Cal doctor for the complex medical condition cannot be changed, because your condition could get worse; AND
- Your Regular Medi-Cal doctor is NOT part of a plan in your county. You may see more than one Regular Medi-Cal doctor. If you do, have the form filled out by the doctor who sees you most often. Ask your Regular Medi-Cal doctor if he or she is part of a Plan in your county. This should be done before you submit this form.
- You have a complex medical condition; AND
- Provider Search – Statewide Fee for Service
- See our webpage on IMR Independent Medical Review
Health Insurance unfortunately is very complicated
President Trump February 27, 2017
- Thus, if we haven't simplified and explained in PLAIN ENGLISH what you are looking for:
Trump Make America Healthy Again
Nearly half of the U.S. population is pre-diabetic or has type-2 diabetes. Every month, diabetes causes 13,000 new amputations, 5,000 new cases of kidney failure and up to 2,000 new cases of blindness in our country. In 1960, approximately 13 percent of American adults were obese. Now, more than 40 percent of Americans are obese, and more than 70 percent are either obese or overweight.
Even more shockingly, one-quarter of our teenagers today are pre-diabetic or have type-2 diabetes, and obesity is the leading medical reason that 71 percent of young Americans are disqualified from military service. Learn More >>> The Hill
6 positions
1. Mr. Kennedy has prioritized addressing chronic disease, which accounts for over $1 trillion in annual U.S. healthcare costs. He has stated that President-elect Trump seeks "measurable impacts" to combat the chronic disease epidemic within two years — a goal that has drawn attention from healthcare leaders, some of whom have praised its ambition while noting potential challenges.
Mr. Kennedy identified chronic disease as a key priority before his nomination to lead HHS. "I'm going to urge President Trump on day one to do the same thing they did in COVID, which is to declare a national emergency, but not for infectious disease, but for chronic disease," Mr. Kennedy said in a Sept. 26 interview, about one month after he dropped out of the presidential race.
His vision extends beyond healthcare delivery to address broader contributors to chronic disease. Mr. Kennedy has criticized the influence of the pharmaceutical and food industries, linking issues like obesity and diabetes to ultra-processed foods, federal subsidies and dietary guidelines. He has called for reforms targeting food additives, pesticides and environmental health risks, alongside overhauls of agencies like the CDC and FDA.
Health systems may find some common ground in Mr. Kennedy's focus on prevention and early intervention to reduce chronic disease burdens, which could align with some of their efforts to address social determinants of health. However, experts, including former CDC Director Tom Frieden, MD, caution against oversimplification. "There are some things that RFK Jr. gets right," Dr. Frieden told NPR. "We do have a chronic disease crisis in this country, but we need to avoid simplistic solutions and stick with the science."
2. He's called for an end to direct-to-consumer advertising for prescription drugs. Mr. Kennedy has criticized the advertising relationships between pharmaceutical companies and news outlets, arguing that pharmaceutical advertising influences editorial content and public discourse beyond its intended purpose of promoting products. When his campaign was active in early 2024, Mr. Kennedy said if elected he would issue an executive order on his first day in office to ban pharmaceutical advertising on television.
Direct-to-consumer advertising of prescription drugs surged after the FDA eased restrictions in 1997 and totaled nearly $10 billion in 2016. Proponents argue it educates consumers and empowers patient involvement, while critics warn it can misinform patients, drive inappropriate prescribing and inflate healthcare costs. Concerns also include promoting costly brand-name drugs over cheaper alternatives, straining patient-physician relationships.
3. He has expressed interest in redirecting Medicare spending toward promoting healthy behaviors rather than covering certain pharmaceuticals. Mr. Kennedy has been a vocal opponent of Medicare and Medicaid funding for GLP-1 drugs used for weight loss, arguing that these programs should instead prioritize covering gym memberships and healthier food options for enrollees.
"For half the price of Ozempic, we could purchase regeneratively raised, organic food for every American, three meals a day and a gym membership, for every obese American," Mr. Kennedy said during a Congressional roundtable in September, as reported by the Associated Press.
The Biden administration recently proposed broader coverage of GLP-1 and weight loss drugs for Americans with obesity, a move that could put Mr. Kennedy in a reactive position if he secures confirmation to lead HHS.
4. He is considering changes to the Medicare physician fee schedule. Mr. Kennedy and his advisers are considering an overhaul of Medicare's payment formula, four anonymous sources told The Washington Post in November. The move could mark a bid to shift the health system's incentives toward primary care and prevention.
The Medicare physician fee schedule was adopted in 1992, establishing a complex system of administrative pricing based on the resource inputs used in producing physician services. It influences not only Medicare payments, but also private insurance payment systems, which often mirror Medicare's methodologies.
Sources told The Post that discussions about the fee schedule are in their early stages and have involved a plan to review the thousands of billing codes that determine how much physicians get paid for performing procedures and services. These codes are integral to determining reimbursement rates and have faced criticism for historically favoring procedural and specialty care over primary care services. An overhaul could address these disparities and potentially reshape the economics of medical practice across the country.
5. He has raised controversial and widely challenged claims about vaccine safety for nearly 20 years. Mr. Kennedy's suspicion of vaccines dates back to at least 2005, when he published an article called "Deadly Immunity" in unusual publications for the topic: Rolling Stone magazine (print) and Salon (digital). The article claimed that thimerosal, eliminated in routine childhood vaccines in 2001, caused autism. The article was amended and corrected several times before, years later, Salon announced in 2011 that it was retracting "Deadly Immunity" in entirety. An explanation of that decision and the corrections made to Mr. Kennedy's article are detailed by Salon here.
More recently, Mr. Kennedy said in a 2023 podcast interview that, "There's no vaccine that is safe and effective." The nonprofit Mr. Kennedy was aligned with for nearly a decade, Children's Health Defense, has been a vocal critic of COVID-19 vaccines and public health mandates, with its claims frequently challenged by public health experts. The group has filed dozens of federal and state lawsuits since 2020, many challenging vaccines and public health mandates. Mr. Kennedy has been on leave from the group as its founder, chairman and chief litigation counsel since he announced his plans to run for president in April 2023.
When described as anti-vaccine, Mr. Kennedy has pushed back. Instead, he argues that he wants to improve the science of vaccine safety. "We're not going to take vaccines away from anybody," he told NPR in November. "We are going to make sure that Americans have good information. Right now the science on vaccine safety particularly has huge deficits in it, and we're going to make sure those scientific studies are done and that people can make informed choices about their vaccinations and their children's vaccinations."
6. He supports abortion rights up to the point of fetal viability, after which he favors restrictions. Mr. Kennedy believes abortion should be legal up to a point he describes as when the fetus becomes viable outside the womb, after which he supports restrictions. Mr. Kennedy clarified this position in a video released in June 2024, though he did not specify an exact number of weeks for viability. He acknowledged that his views on abortion have evolved over time as he continued to explore the issue. In May 2024, he had expressed support for a woman's right to choose an abortion at any stage of pregnancy, including full term.
Mr. Kennedy has also pointed to the importance of addressing economic factors in discussions about abortion and reproductive health. "We should be looking at why there are so many abortions in the first place," he said, emphasizing the need to understand the financial challenges and economic pressures that contribute to abortion rates among individuals and families.
Mr. Kennedy introduced a plan while running for president called "More Choices, More Life" that called for a subsidized daycare initiative aimed at making childcare more accessible. He said universal childcare has the capacity to add $1 trillion to the U.S. GDP. "And since economics is a major driver of abortion, this policy will do more to lower abortion rates than any coercive measure ever could," the website for the plan states. Becker Hospital Review *
Medi Cal Contact Information
- #Email Addresses & Phone #'s
- Who to #contact at Medi Cal
- Main Email to Get a hold of Medi Cal --- [email protected]
- All inquiries related to Medi-Cal, including questions about terminating Medi-Cal coverage, must be referred to the beneficiary’s local county Social Services office.
- • Department of Health Care Services County Listings:
- • Covered California’s Medi-Cal page:.
- • Medi-Cal Reminders and When to Contact County Social Services:
- guide outlining information that certified enrollers can use when assisting Medi-Cal beneficiaries who may be eligible for and wish to enroll into a Covered California plan.
- • Department of Health Care Services County Listings:
- dhcs.ca.gov/medi-cal/Contacts
- health care options.dhcs.ca.gov/contact-us
- Medi-Cal Rx Customer Service Center
- Department of Health Care Services Contacts
- [email protected] regarding general Medi-Cal eligibility.
- If the question contains specific details the county or the district office that handles your case must answer.
- Benefits Cal - Enrollment Website

- • Assisting Medi-Cal Eligible Consumers FAQ:
- frequently asked questions and glossary terms to understand the Medi-Cal enrollment process and learn how to seek help for various scenarios.
- California Department of Health Care Services 1-844-253-0883
- Non MAGI Medi Cal 1.916.345.8675
- [email protected] Ms. Leslie Benson
- IHSS In Home Supportive Services
- Ombudsman Webpage
- Phone: 1-888-452-8609
- Email: [email protected]
- The Office of Ombudsman cannot approve/terminate/reinstate Medi-Cal eligibility; alter aid codes, change/update addresses, change/update name or initiate inter-county transfers.
- Complex Questions Assistance
-
- Health Consumer Alliance at 1-888-804-3536.
- Disability Rights California at 1-800-776-5746.
-
-
- HICAP – Health Insurance Counseling & Advocacy Program
- CA Health Care Advocates – 1-800-434-0222 Volunteer counselors can help you understand your specific rights and health care options
- CA Health Care Advocates – 1-800-434-0222 Volunteer counselors can help you understand your specific rights and health care options
- Medi Cal Consulting Services
- National Center on Law & Elder Rights
- VITA Volunteers Income Tax Assistance
- Bet Zdedek Legal Services
- Medi Cal - Technical Comprehensive Reference Materials
- Our webpage on education, research & tutoring for a fee
- aging.ca.gov/Medicare_& Medi Cal Counseling
- Elder Care locator
- medi helper.com

- Pdf Brochure - I was told their fee is $3k
- HICAP – Health Insurance Counseling & Advocacy Program
See our Main Webpage on Medi Cal contact information
Non MAGI Medi Cal
Medi Cal
out of state and #emergency coverage?
- CA Medi Cal – Out-of-state medical care is limited to the following:
- (a) (1) When an emergency arises from accident, injury or illness; or
- (2) Where the health of the individual would be endangered if care and services are postponed until it is feasible that he/she return to California; or
- (3) Where the health of the individual would be endangered if he/she undertook travel to return to California; or
- (4) When it is customary practice in border communities for residents to use medical resources in adjacent areas outside the State; or
- (5) When an out-of-state treatment plan has been proposed by the beneficiary’s attending physician and the proposed plan has been received, reviewed and authorized by the Department before the services are provided; and the proposed treatment is not available from resources and facilities within the State.
- (6) Prior authorization is required for all out-of-state services, except:
- (A) Emergency services as defined in §51056.
- “emergency services” means those services required for alleviation of severe pain, or immediate diagnosis and treatment of unforeseen medical conditions, which, if not immediately diagnosed and treated, would lead to disability or death.
- (B) Services provided in border areas adjacent to California where it is customary practice for California residents to avail themselves of such services. texas.gov/medicaid
- Medi Cal Treatment Authorization Request
- 540-1 (a) (5) When an out-of-state treatment plan has been proposed by the beneficiary’s attending physician and the proposed plan has been received, reviewed and authorized by the Department before the services are provided; and the proposed treatment is not available from resources and facilities within the State
- (A) Emergency services as defined in §51056.
- Medi Cal only covers outside of CA for emergencies and very special circumstances. Cornel Law *
- Sources
- cdss.ca.gov/Medi-Cal-Out-of-State-Coverage
- casetext.com/section-51006-out-of-state-coverage
- Cornel Law
#Explanation from Western Poverty Law
Chapter 2. MAGI Medi-Cal Programs
1. Tax Filer Rules
2. Non-Filer Rules
3. Counting Households with a Pregnant Woman
B. Counting Income
C. MAGI Medi-Cal Programs
1. Expansion Adults
2. Parents and Caretaker Relatives
3. Pregnant Women
a. MAGI Medi-Cal Programs for Pregnant Women
b. Medi-Cal Access Program (MCAP) for Pregnant Women and Newborns up to Age 2
4. Children: MAGI Medi-Cal, the Targeted Low-Income Children’s Program, and MCAP Infants and Babies
a. Infants: 0 to 1 year old
b. Children: Ages 1 to 6
c. Children: Ages 6 to 19
-
- California Advancing and Innovating Medi-Cal (CalAIM) is a long-term commitment to transform and strengthen Medi-Cal, offering Californians a more equitable, coordinated, and person-centered approach to maximizing their health and life trajectory.
- Medicaid.gov
- Disability Benefits 101
- Western Poverty Law Center Guide
- Medi-Cal enrollees not sure how to use coverage california health line.org
- Medi-Cal pays $415 to $575/month or MORE to HMO’s to take care of you Learn More⇒ Insure Me Kevin.com 3.4.2016 5.11.2014
- Medi Cal Explained CHCF
- Medi-Cal Facts and Figures, 2024 Edition Gives a lot of information on ALL Health Insurance Programs
- chcf.org/cal aim-resources-
- cal matters.org/medi-cal-eligibility/
- dhcs.ca.gov/Budget-Highlights
- ebudget.ca.gov/Full Budget Summary
-
Prescription drugs.
- Hearing Aid Cap FAQ’s
- Health screenings for kids
- Preventive and wellness services and chronic disease management.
- Mental Health CHCF Fact Sheet
- Substance abuse CHCF Article
- Maternity
Ongoing Care & Recovery
- Personal care services (IHSS)
- Nutrition Food & Meals
More Details
- My Medi-Cal brochure
- dhcs.ca.gov/Medi-Cal_EHB_Benefits
- dhcs.ca.gov/Benefits_services.aspx
- dhcs.ca.gov/Benefits-Chart
- Check with your HMO Providers Evidence of Coverage
- Insure Me Kevin.com – Medi Cal HMO same coverage as Covered CA HMO! Provider list may differ!
-
Medi-Cal determines eligibility based on #monthly, not annual income.
- Even you you make $100k per year, but have a month with no income, you would qualify. This can even get you around the Open and Special Enrollment restrictions. That is, if you have a bad month, enroll, then when you get kicked out of Medi-Cal for making too much money, as you reported it, as required by law, within 10 days, thank G-d, you have a special enrollment into Covered CA or direct with an Insurance Company. No extra charge for us to help you enroll in Covered CA! Insure Me Kevin.com * Western Poverty Law * DHCS ACWDLS * 2015 Medi-Cal Eligibility Division Information Letters (MEDILs) * 15-03 *
- Plain English from Covered CA Broker Department Email
- In regards to Medi-cal, they review monthly income.
- So if a client has been making $2000 a month and they do a report a change and it goes now to $1000 a month for 1 person, they will now be eligible for medi-cal.
- If the income goes back up to $2000 a month, they contact [report a change] Medi-cal and they are dis-enrolled from medi-cal and now are eligible for Covered CA. Response By Email (Argelia) (09/08/2016 11:56 AM)
FAQ’s
Conditional & Temporary Coverage
- What if Medi-Cal took hold of my file, but says I don’t qualify, is there a lapse in coverage?
Will Covered CA backdate coverage? - Answer – you have conditional coverage while Medi Cal is investigating your application. When Medi Cal disenrolls you, you are automatically enrolled under SB 260 into a Covered CA plan. We can help you with that. Just appoint us as your broker. No extra charge.
Links & Resources
- california healthline.org/illegal resident-expansion
- kff health news.org/morning-breakout/californians-face-long-wait-times-when-calling-medi-cal-analysis-finds/
- https://www.chcf.org/publication/medi-cal-facts-and-figures-2024-edition/
- https://www.chcf.org/blog/medi-cal-considers-income-not-assets-enrollees/
- FAQ Medi Cal Rx
https://medi-calrx.dhcs.ca.gov/cms/medicalrx/static-assets/documents/faq/Medi-Cal_Rx_Members_FAQ.pdf - Medi Cal for illegal aliens…
- https://www.dhcs.ca.gov/services/medi-cal/eligibility/Pages/Adult-Expansion.aspx
- https://www.dhcs.ca.gov/services/medi-cal/eligibility/Pages/youngadultexp.aspx
- https://www.dhcs.ca.gov/services/medi-cal/eligibility/Pages/OlderAdultExpansion.aspx
- https://www.dhcs.ca.gov/services/medi-cal/Pages/Medi-CalFairHearing.aspx
- https://healthconsumer.org/wp/wp-content/uploads/2017/04/cs032WorkingDisabled.pdf
- https://insuremekevin.com/magi-medi-cal-income-eligibility-for-2023-increases-over-6/
- https://www.dhcs.ca.gov/services/medi-cal/eligibility/Pages/youngadultexp.aspx#:~:text=This%20initiative%2C%20called%20the%20Young,DHCS)%20website%20for%20SB%2075
- https://www.coveredca.com/learning-center/information-for-immigrants/deferred-action-for-childhood-arrival/
- https://khn.org/morning-breakout/cms-proposes-rules-to-ease-enrollment-in-medicaid-chip/
- https://insuremekevin.com/medi-cal-bridging-the-gap-for-adults-26-49-years-old/
- https://www.shouselaw.com/ca/defense/fraud/medi-cal-fraud/
- https://www.desertsun.com/story/news/health/2022/05/03/california-expands-medi-cal-services-undocumented-seniors/9620961002/
- Our webpage on child support & medi cal
- https://www.chcf.org/wp-content/uploads/2019/03/MediCalExplainedEligibilityEnrollment.pdf
- https://www.chcf.org/wp-content/uploads/2019/03/MediCalExplainedEligibilityEnrollment.pdf
- https://www.chcf.org/wp-content/uploads/2019/02/MediCalExplainedPaymentManagedCarePlansCurrentProcessChallenges.pdf
- Newsom Wants to Expand Medi-Cal to All Undocumented Immigrants by 2024. Advocates Say They Need It Soonerhttps://www.sacbee.com/news/politics-government/capitol-alert/article262935493.html
- Disability Rights CA Medi Cal Resources
- Medi-Cal Info on Covered CA Website
- wikipedia.org on Medi Cal
- Mental Health
- Eligibility
- Payments to HMO’s
- Medi Cal budget
- Insurers make billions off Medicaid in California during Obamacare expansion LA Times 11.5.2017
-
ObamaCare – #Expansion to 138% of FPL
-
Assembly Bill 1 ** Senate.bill.1.
- If you don’t have free Medicare Part A
- Work Requirements
Report Changes Promptly
#Report changes as they happen - within 30 days! 10 CCR California Code of Regulations § 6496
10 days for Medi Cal 22 CCR § 50185
Our webpage on ARPA & Unemployment Benefits - Silver 94

IRS Form 5152 - Report Changes
- Our VIDEO on how to report changes to Covered CA
- Lost your job? How to keep your Health Insurance. Shelter at Home VIDEO
- References & Links
- Here's instructions, job aid, reporting change in income
- Our webpage on the exact definition of MAGI Income
- If you've appointed us - instructions - as your broker, no extra charge, we can do it for you.
- Voter Registration
- Denial of benefits and possible criminal charges if you don't report changes in income!
- When Increasing Your Covered California Income Estimate Creates an Ethical Dilemma Insure Me Kevin.com
- Fudging Income?
- Western Poverty Law on reporting changes
- How to cancel coverage.
- agents and brokers who suspect or know a fraudulent application for insurance has been submitted to report the potential fraud to the California Department of Insurance Fraud Division. Read more >>> Wshblaw.com
- Visit our webpage on how to report changes
#VITA Volunteers Income Tax Assistance
get your taxes done Free
- Publication 3676 with more details on VITA
- Our Webpage on VITA & Covered CA prohibition to give tax advice
- More places to find FREE tax help Covered CA list
- Turbo Tax -
- See more tax calculation links in the section on IRS Publication 974 Premium Tax Credit
**********************************
#Covered CA Certified Agent
No extra charge for complementary assistance
- Get Instant Health Quotes, Subsidy Calculation & Enroll
- Appoint us as your broker
- Get Instant Health Quotes, Subsidy Calculation & Enroll
- Videos on how great agents are
MORE
Much more on Medi Cal
- Medi Cal Explained CHCF
- More
- Historical Guide 2006 CHCF 174 pages
- Cal AIM California Advancing and Innovating Medi-Cal — is a far-reaching, multiyear plan to transform California’s Medi-Cal program and to make it integrate more seamlessly with other social services. The goal of CalAIM is to improve outcomes for the millions of Californians covered by Medi-Cal, especially those with the most complex needs.
- You Tube Videos
- DHCS.CA.Gov
- chcf.org/focus-on-cal aim
- VIDEO Introduction to Medi Cal Los Angeles DPSS
- California voters give Medi-Cal doctors a raise by passing Prop. 35
- 10 Essential Health Benefits
- Our Webpage on Medi Cal Benefits
- Denti Cal
******************************************
- Western #Poverty Law – Exact Legal Rules on Coverage for Low Income Californian’s
Nolo Social Security, Medicare, Medi Cal & Government Pensions
-
Our Webpage on COVID 19
- CA State Senator Steven Bradford 35th District
- His Webpage on COVID 19 Resources
-
BIC Benefits Identification Card
FAQ’s “C-CHIP County Children’s Health Initiative Program”
- I am a (the?) legal guardian of my Great Granddaughter. She receives benefits from Social Sec. since her Mother is deceased. I need to get her covered with health insurance, but I don’t know were to apply. Every time I try, They ask for my information I’m on Medicare and I don’t want to change it. I’m 70 years old. Can you please help ?.
- First – Enter yours and your great granddaughters information here and get a quote. What is their your family MAGI income? Does your great granddaughter live with you? Are you taking the deduction for her on your tax return? See the household definition chart. Once I know yours and their income, I would be able to tell you if you go Medi Cal, it’s a function of Income, see chart, where I don’t get paid to help you or Covered CA where if I’m lucky, I get minimum wage. They are asking for your information, as their qualification for Medi Cal or Covered CA is a function of Household income. You will still stay on Medicare! Here’s the ONLINE application Medi Cal.
- MY TWO CHILDREN ARE eligible FOR C CHIP PROGRAM, BUT I AM UNABLE TO GET THROUGH TO GET THEM REGISTERED IN THE PROGRAM. I WAS NOT ABLE TO SPEAK TO ANYONE THat MAde SENSE. COVERED CAL. TOLD ME TO TALK TO CCHIP, CCHIP TOLD ME TO TALK TO COVERED CA. PLEASE HELP!
- We don’t get paid to help people enroll in Medi-Cal, so this would be pro-bono for us. Please appoint us as your Covered CA agent – Instructions – or just call them and have us appointed. My guess is, that you don’t have your ducks in a row, to show the proper income levels. What have you filed? How about going ONLINE and completing the paperwork?
- The County Children’s Health Initiative Program (C-CHIP) a health insurance program (Medi-Cal) that offers affordable and comprehensive medical, dental, and vision insurance for children age 0-19 who qualify. Qualification is in 3 Northern CA counties and is for those who are just out of the normal Medi Cal income limits 266-322% Federal Poverty Level (FPL).
- Learn more by clicking on the links below:
- InsureKidsNow.gov
- Health Care.Gov
- Medicaid.gov
- LA County.Gov
- Children’s Health Outreach
- cchi 4 families.org
- Disability Benefits 101 – Excellent explanation!
- Los Angeles ONLINE Enrollment – Contact Information for other counties
- Work Requirements?
- CHIP Children’s Health Insurance Program
- Hospital Presumptive Eligibility HPE
- Undocumented age 50 & over
- Learn more by clicking on the links below:
FAQ’s
- How does Covered California work with Medi-Cal?
- Covered California will act as a “one-stop shop” for health insurance. Through Covered California, you will be able to apply for Medi-Cal benefits electronically and receive a real-time eligibility results. You will also be able to report changes online and receive real-time customer support 24 hours a day. dhcs.gov More FAQ’s DHCS ♦ Insure Me Kevin.com
- Disability Benefits 101 – Medi-Cal The Details
- What is California Advancing and Innovating Medi-Cal (CalAIM)
- Cal Aim is a long-term commitment to transform and strengthen Medi-Cal, offering Californians a more equitable, coordinated, and person-centered approach to maximizing their health and life trajectory.
- Goals of CalAIM
- 1. Identify and manage comprehensive needs through whole person care approaches and social drivers of health.
- 2. Improve quality outcomes, reduce health disparities, and transform the delivery system through value‑based initiatives, modernization, and payment reform.
- 3. Make Medi-Cal a more consistent and seamless system for enrollees to navigate by reducing complexity and increasing flexibility. DHCS *
- why doesn’t medi-cal really help? So long on #hold, so much wasted time?
-
- Why is my website so much more informative than Medi-Cals or Covered CA’s?Medi-Cal like any other “business” wants to expand. So they have a motive to keep you there. The Co-Pays and deductibles are lower. They include adult dental & vision.Medi-Cal and the Insurance Companies don’t pay agents, yet it’s just as time consuming and complex to help people with Medi Cal as a Covered CA or direct plan!
- Here’s links on why Government workers are lazy:
- If you like waiting on hold with Covered CA – Stay there. If you would like to just send an email and I’ll take care of it, appoint me as your agent and I’ll see what I can do.
- Why is my website so much more informative than Medi-Cals or Covered CA’s?Medi-Cal like any other “business” wants to expand. So they have a motive to keep you there. The Co-Pays and deductibles are lower. They include adult dental & vision.Medi-Cal and the Insurance Companies don’t pay agents, yet it’s just as time consuming and complex to help people with Medi Cal as a Covered CA or direct plan!
- It’s been a whirlwind deciding what to do, health-insurance-wise and, after a consultation with our tax guy, we’ve decided to register for Medi-cal. I know you get no money from this, so I’m sorry for wasting your time with Oscar Insurance inquiries. Thank you for all of your help. We’ll be in touch in the future if, as we hope, we can make enough money to get back on CC.
Effective Date? Temporary Instant ID Card”
- I have dropped my coverage from Blue Shield since my income this year has been $0. I haven’t worked since I was laid off last year. I want to move over to medi-cal but I can’t get an application started on account that LA County has me on “pending” for medi-cal. I have been ‘pending’ for a year and a half. I haven’t lived in Los Angeles for a year now. I’m up in Lake County and there medi-cal office says they can’t do anything until LA drops my medi-cal application– that I never put in. Do you know who I need to get a hold of in order to resolve this?
- Try the instructions on our Los Angeles Medi Cal webpage
- Try the contact people and departments on this page
- You might also try going into your Covered CA account and changing your address or call Covered CA 1 800 300 1506
As an agent, I’m not excited about doing all the extra work, as there is no compensation to assist with Medi Cal.
- I have tried to change my address 4 times online and have talked to a covered California Representative 3 times and the medi-cal rep of Lake County once without change. I don’t understand why this would be made so difficult.
- I sent you a video and a screen shot that I completed the change of address and income for you.
- Covered CA wants proof of income
- President Trump said Insurance was very complicated and no one knew that it was, he should have asked me. VIDEO
- Steve’s educational background
- Learn more about Conditional Eligibility












https://www.chcf.org/wp-content/uploads/2017/12/PDF-PhysicianParticipationMediCalEnrollmentBoom.pdf
https://www.cmadocs.org/newsroom/news/view/ArticleId/21480/Study-finds-fewer-California-physicians-accept-Medi-Cal-despite-a-surge-in-patients
https://www.commonwealthfund.org/blog/2025/how-medicaid-state-directed-payments-support-critical-health-care-providers
If your carry over net operating loss (from prior years) is allowed to be taken into account, is it part of the Federal Modified Adjusted Gross Income number ) or does California specifically require you to take it out of the equation?
REPLY
See our webpage on Capital Gains and Carry Over Losses
Medi-Cal is California’s Medicaid program, which provides health insurance to individuals and families who earn low incomes, including 40% of the state’s children, half of Californians with disabilities, and over a million seniors. In total, the program covers more than 12 million people, or nearly one in three Californians.
Medi-Cal also covers a large number of working Californians, many of whom became eligible for the program because of the Affordable Care Act’s Medicaid expansion. Working Californians may be one of the least recognized or understood populations served by the program. In a 2018 poll, 42% of Californians said that they believed that most working-age adults without a disability enrolled in Medi-Cal are unemployed. Twenty percent said they didn’t know. This report combines key findings from survey data with insights from 19 in-depth interviews with enrollees to paint a more accurate and complete picture of working Californians who rely on Medi-Cal, why they came to enroll in the program, and the role it plays in their lives.
The report is accompanied by video stories from a few working Californians who participated in the in-depth interviews
https://www.chcf.org/publication/working-californians-enrolled-medi-cal-stories/
My family is receiving medi-cal in California due to low income.
If I sell my house, will that disqualify me for medi-cal for that year only or will it disqualify me longer?
See the rules about low income subsidy and selling a home for reference.
See our page on Capital Gains and the sale of a home
Being as MAGI Medi Cal is based on monthly earnings, it looks like you only would be in Covered CA for a month, if that’s what you want.
Get Covered CA quotes here.
Did you need life insurance to protect your family?
I am on Medi-Cal ( CA medicaid) as an “expansion adult” qualified based on MAGI.
I am turning 65 next week so supposedly my MAGI eligibility ends right then but I haven’t received any “dis-enrollment” or “recertification” notices.
So I wonder how that works and for how long I am “safe”… That would affect when I want my medicare to start.
We are not aware of any Medicare provision that allows one on MAGI Medi-Cal to delay enrollment. In fact, there are Part B penalties if you don’t enroll on time.
If you have to pay for Part A Hospital and don’t sign up on time, there is a penalty.
You are MANDATED to inform Medi-Cal of any changes to eligibility within 10 days. Medi-Cal might get VERY pissed, if you don’t
Welfare & Institutions Code 14005.37. (h) Beneficiaries shall be required to report any change in circumstances that may affect their eligibility within 10 calendar days following the date the change occurred. See Also Western Poverty Guide page 6.226
BUT, per your redetermination page
and https://www.law.cornell.edu/cfr/text/42/435.916
Once you are renewed by Medi-Cal it’s good for a year!
Yes, but besides the mandate to report changes, the periodic renewal mentions this:
(d) Agency action on information about changes.
(1) Consistent with the requirements of § 435.952 of this part, the agency must promptly redetermine eligibility between regular renewals of eligibility described in paragraphs (b) and (c) of this section whenever it receives information about a change in a beneficiary’s circumstances that may affect eligibility.
Yeah, but Medi Cal already knows my date of birth, so nothing has changed!
You’re going beyond our pay grade. We are not lawyers.
When to report a change in circumstances to Medicaid?
If the Medicaid recipient does nothing, they are breaking the law. A change in circumstance is also for minor but important life events such as change of address. If you don’t let SSA know, then they can’t communicate with you, which will cause a whole host of potential problems.
If the Medicaid recipient does nothing after a significant change in circumstances (such as coming into new money), Medicaid will eventually find out (likely from the IRS) or as part of a random audit and they may kick the Medicaid recipient out of the program and demand retroactive reimbursement for benefits paid while the person was no longer qualified. https://www.elderneedslaw.com/blog/change-in-circumstance
https://www.cbpp.org/health/medicaid-compliance-with-eligibility-requirements
Did you report that you would be eligible for Medicare?
Western Poverty 6.226
Age: Expansion Adults must be at least 19 years old and under age 65
Beneficiaries who turn 65 while they are enrolled in Medi-Cal as an Expansion Adult must be evaluated for eligibility in all other Medi-Cal programs, i.e., non-MAGI programs such as for the aged, blind or disabled, before they are disenrolled.
https://wclp.org/wp-content/uploads/2016/06/Western_Center_2016_Health_Care_Eligibility_Guide_Full_rev.1.pdf#page=50
23. 42 U.S.C. § 1396a(a)(10)(A)(i)(VIII); 42 C.F.R. § 435.119(b)(1); Welf. & Inst. Code § 14005.60(a); MEDIL 13-12 (Sep. 16, 2013) at p. 6,
24. Welf. & Inst. Code § 14005.37(d)
Aged & Disabled?
Covered CA agrees with that on children who turn 26. They can stay on the plan till the end of the year.
Here’s a graph about waiting too long to enroll in Medicare Part B.
Publication 11036
Penalties for Part B even if you had Covered CA…
https://cahealthadvocates.org/equitable-relief-waiver-of-part-b-penalties-ends-sept-30-apply-now/
https://medicare.healthreformquotes.com/seminar/part-b/part-b-doctor-visits-late-enrollment-penalty/covered-ca-waiver-part-b-penalty/
Reply from Medi-Cal!!!
Dear Steve,
You can stay on Medi-Cal after the age of 65 years of age, even if your renewal happens before the age of 65 years old. If you have full Medi-Cal benefits, you pay no Medicare cost sharing.
The medical services must be covered by Medicare and Medi-Cal. share of coast before Medi-Cal pays for your medical expense.
Medi-Cal will only cover these costs and services if you use providers that accept Medi-Cal. … If you qualify for full Medi-Cal (Medi-Cal without a share of cost (SOC)), Medi-Cal will also cover your Medicare Part A and B deductibles and copayments, and pay your monthly Medicare Part B premium.
Let me suggest you review the Medicare webpage , and provide you with more information.
Thank you for allowing DHCS to serve you.
Timothy
Here’s our webpage on signing up for Medicare A & B
Can one trust what a Government Worker says?
President Trump – No one except Steve Shorr knew how complicated Insurance was
https://youtu.be/b_8UFNQqk7k
View more FAQ’s
Hi Steve,
Confusion about MAGI Medi-Cal.
For those young adults who are healthy, not pregnant but have no income goes into the MAGI Medi-cal file.
Although the asset test is said to be no longer required, why do case workers still ask for bank statements and questions about personal assets?
Are they confused?
Medi-Cal has many other programs that you might qualify for. Like food stamps, nursing home, phones, etc. Medi-Cal has a wide range of social services. They are Social or Case workers.
See also our page on “bank statement review”
Hi Steve,
I have a Medi-Cal question you might be able to answer or point me in the right direction.
My wife and I have an adult son with various medical problems. He’s on Medi-Cal since his MAGI is below the limit because he can work only part-time due to his health. So he can’t support himself alone.
He lives with us and we feed him.
However, he files his own income taxes, meaning we don’t have him on our return as a dependent.
Nonetheless, is our financial support somehow jeopardizing his Medi-Cal eligibility?
Thank you for being generous with your time and knowledge.
See our webpage on counting household size for someone filing their own tax return and not being claimed as a dependent elsewhere.
Let me see if providing room and board counts as gift income?
Paying for the living expenses of an individual you do not have a legal obligation to support. In addition to non-related parties, this also could apply to adult children. If you are paying for the room and board for a child you are no longer obligated to support, this may be a gift. http://www.troutcpa.com/blog/what-is-a-gift
Not all money transfers are gifts The IRS isn’t interested in the rental value of your child’s old bedroom, or the amount of food that disappears from your refrigerator.https://blog.taxact.com/gift-tax-supporting-adult-children/
Covered CA list of countable income
This question is really beyond my pay grade. Covered CA suggests you try VITA. I would think the question is beyond their pay grade too. Try your own CPA.
Do you need life insurance to make sure your son is supported if you are not here?
Thank you Steve, I will check these out.
Eligibility is determined by MAGI, but is there also a countable property limit?
See reply to virtually the same question below.
If I remarry, would my child lose his Medi Cal? The child qualified as my spouse passed away.
I’m not familiar with Medi Cal benefits, simply because a parent passed away.
Please advise what program that is.
If you only have private documents from Medi Cal or Social Security so stating, please send that to me privately at [email protected]
If what you mean is, the income for you and the child is below 266% of Federal Poverty Level Chart or $45k for a family of two, then the child would qualify for Medi Cal. Family of 3 $57k.
Family Size basically goes by whose on the tax return. For Covered CA and I presume Medi Cal, married persons must file jointly.
So, please respond anonymously with yours and your “fiances” income and I’ll look at the charts for you…
I have too much money in my bank account assets to qualify for Medi-Cal, but I don’t make enough to qualify for Covered CA subsidies. What can I do?
There is no longer an asset test for Medi Cal. You need to earn at least $17k to get subsidies with Covered CA. Click here to enroll in Medi Cal in Los Angeles County I don’t get paid to help you enroll or to answer questions.
https://wclp.org/wp-content/uploads/2016/06/Western_Center_2016_Health_Care_Eligibility_Guide_Full_rev.1.pdf#page=4
H. Assets or Resources
In an effort to simplify program rules, the MAGI methodology does not consider assets or resources other than income. Thus applications for MAGI Medi-Cal, MCAP, and Covered California do not have any questions about bank accounts, homes, cars, property, etc.
On the other hand, most non-MAGI programs that count income still have limits on what resources an individual may have besides income to qualify for MediCal. However, like everything else with the non-MAGI programs, the rules vary by program.
For example,
the Medicare Savings Programs (QMB, SLMB, etc.) have a countable resource limit of $4,000 for an individual and $6,000 for a married couple, while
the 250% Working Disabled Program has a resource limit of $2,000 for an individual and $3,000 for a couple.
In general, non-MAGI programs that do not count income, such as the program for Former Foster Youth or the Minor Consent program, do not look at resources either.
Medi-cal enrolled a lot of people that were not eligible
http://www.latimes.com/business/la-fi-california-medicaid-expansion-20180326-story.html
Thanks Steve – much appreciated. Two more questions regarding your answer:
At 55 can medical seek premiums from an estate that I am a beneficiary?
Are interest or dividends that are received within a ira considered untaxable intrest/dividends, and therefore added to MAGI?
I don’t think Medi-Cal would have a lien of what you inherit. Their lien would be on what remains in your estate when G-d forbid, you pass away.
On my estate recovery page I’ve done say 20 hours of research putting together the links and information. I’m not an attorney, so I suggest you contact one or read through all the links and brochures that I’ve thought were good enough to make it to my website.
IRA interest is also tax exempt until you withdrawn the money. I’m not a CPA and don’t know your full situation. Learn More ===> IRS Publication 590
I’m a 45 year old male who is single and on medi-cal. I have a Roth worth $11,000 and a car. My earnings this year will be $20,000 approximately. If I contribute $5,000 to a traditional IRA this year to bring my MAGI to below 138% of the poverty level, will I be able to requalify for Medi-cal?
Assets are no longer a factor in MAGI based Medi-Cal qualification. An IRA deduction on line 32 of your 1040 would lower line 37 which is the basis of MAGI income, as most taxpayers don’t have foreign income, social security or tax exempt interest to add back in.
Please be sure to double check with competent tax counsel, the answer appears to be yes.
On the other hand, you are nearing age 55 at which point, the Medi-Cal premiums can be deducted from your estate.
Is there any way you can look for a better job or take another part time job to get your earnings up?
Send us a private email, we can help you set up your IRA.
Using the link in the upper right-hand corner and getting a free quote and subsidy calculation you may find that covered California with subsidies will look very appealing
Plus the enhanced silver benefits also known as cost sharing reductions
Thanks Steve – much appreciated. Two more questions regarding your answer:
At 55 can medical seek premiums from an estate that I am a beneficiary?
Are interest or dividends that are received within a ira considered untaxable intrest/dividends, and therefore added to MAGI?
I don’t think Medi-Cal would have a lien of what you inherit. Their lien would be on what remains in your estate when G-d forbid, you pass away.
On my estate recovery page I’ve done say 20 hours of research putting together the links and information. I’m not an attorney, so I suggest you contact one or read through all the links and brochures that I’ve thought were good enough to make it to my website.
IRA interest is also tax exempt until you withdrawn the money. I’m not a CPA and don’t know your full situation. Learn More ===> IRS Publication 590
This is a lady who was in a major car accident. Her Father called and we set her up with coverage through Covered CA where I did get a measly commission. She flat out accused me of fraud, lack of integrity, criminal motive, etc. for not putting her into no premium Medi-Cal! Thus, we don’t do coverage for competent adults through 3rd parties. Yes, it’s a quandary, as she wasn’t competent at the time.
Hello Mr. Shorr,
I wanted to tell you I’ve two modes of resolution now for the dilemma I’d been fighting w/BS thru Covered CA. First and this was my initial thought I should have just done on the outset was dispute the charge with my bank. They gave BS what they were owed and returned my overpayment to me immediately as I’d proof I no longer had need for their service and was being enrolled in Medi-cal. It took about ten minutes and I already have my money back.
After spending twenty days and three hours on the phone (mostly holding or educating inexperienced employees) the resolution Blue Shield sought was simply finalizing enrollment in Medi-cal. The Medi-cal Ombudsman had told me to bring my issue back to the county and ask for a hearing and all this run around and I threatened them with a lawsuit so they called me somewhat immediately at least ten times. I’d not answered any of the calls as the caller ID was blocked and so I’d not answered the phone. I couldn’t figure out who’d be so rude to call and not leave a message so many times that I finally answered the call mostly as I wasn’t on another call. Every other time they’d called I was already on with one agency or another getting nowhere. The unknown caller was the actual Ombudsman who said they couldn’t help me and again said to file for a hearing at the county. Then she’d noted I’d not enrolled in Medi-cal yet and I told her in response I’d had no time. She said well let me at least do that for you. I chose the same Medi-cal program as my son and immediately everything fell into place. A letter was issued to Blue Shield with correct ending and beginning dates (that would initiate a refund if appropriate) and I’d met the 20 Sept deadline so I wasn’t just thrown into an unknown plan. All that was required to activate the refund. It’s likely that tomorrow on the deadline it would have also been “magically” solved yet I likely would not have known why if the Ombudsman had not told me all that completing enrollment would entail and not realizing herself that she’d issued the statement to Blue Shield that they’d been awaiting and I’d asked for… It’s almost too crazy to believe…
There are so many gaps in these systems and so many people who don’t understand what they’re supposed to do or what they are doing yet their actions often lead to success unknowingly and it must happen often enough that I’m rare if not the only one who had to suffer for weeks all because I’d not had time to phone and select a plan out of all the horrible plans they offered as I was trying to gain a refund first and the clock kept ticking. I don’t really care what I choose as I’m going to keep paying to see my neurologist in cash and only want my medication to still be covered by insurance as it’s quite expensive.
I realize you don’t wish to work in this area any longer yet it’s possible you may encounter this in a transitional phase. Please note if any of your customers had other insurance they must complete signup in every way to close out the current coverage that then initiated a number of automatically generated forms and communications. The same is true for people on Medi-cal who seek different insurance if they’re able to afford it. Someone must finish the entire enrollment process completely or Medi-cal won’t terminate itself even though a refund wouldn’t be an issue in that case. I won’t likely be needing nor receiving anything from Blue Shield as my bank paid for August and I’m enrolled retroactively so I owe them nothing for Sept. Amazing that no one knew this. Amazing that no one else asked me to complete enrollment given that the deadline is tomorrow. I was only made aware of it yesterday. Thought it might be of some value as this wasn’t a minor undertaking.
Jennifer M