MAGI Medi Cal based on income below
138% of Federal Poverty Level

Medi Cal Qualification under MAGI Income
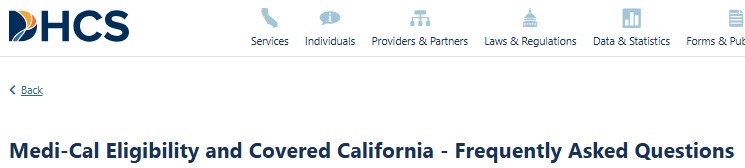
- Medi Changes for 2026 dhcs.ca.gov
- For most individuals, Medi-Cal eligibility will be #based on your household size and your Federal MAGI – Income. Dhcs.gov * My Medi Cal * Western Poverty Law * If you have less than 138% of Federal Poverty Level, for children 266%, that’s it.
- Medi Cal eligibility under Health Care Reform expanded is when you have family household income (MAGI) under 138% of Federal Poverty Level (subsidy income chart for ObamaCare) dhcs.gov for the parents and 266% for children there is no more estate recovery for health insurance.
- Asset test is back for 2026 if you are 65 or older, in a nursing home, have a disabiltiy or make too much money SCROLL DOWN FAQ’s DHCS.CA.Gov *
- If your children qualify for Medi Cal, and the parents for Covered CA – Private Insurance with subsidies you can now apply for both using the Covered CA online application Cbp.org page 65, with us as your agent at no additional charge, just follow these instructions, starting with find help in the upper right hand corner if you fill out the Covered CA application ONLINE, yourself.
- If you are not applying for a subsidized private plan with us as your agent, no charge through Covered CA the easiest and fastest way to apply for or renew Medi-Cal is:
- Directly though your local county human service agency CA State wide listing
- Benefits Cal.org for all Welfare Benefits…
- Please note that we can no longer do extensive research on Medi Cal questions as we are not authorized representatives for Medi Cal, nor do we get compensated one nickel for this website or our time. Please contact Medi Cal or your Medi Cal HMO directly. We will do research and education for a fee.
- Work Requirement Commonwealth Fund.org
- Covered CA Income and FPL Federal Poverty Level Chart
- Covered CA Medi-Cal Overview
- There are nominal premiums for children if you’re at more than 160% of FPL DHCS *
- DHCS.gov Asset Limit FAQ’s
https://developers.facebook.com/docs/plugins/page-plugin/
News & Updates, not yet law
- A looming question confronts California counties: How will they pay for the uninsured? LA Times 12/2025
- What Medicaid changes in Trump’s ‘big beautiful bill’ mean for family caregivers’ health coverage cnbc 1/2026
- Courts, Congress Thwarting Trump’s Cuts On Safety Net Programs, Science KFF News.org 1/2026
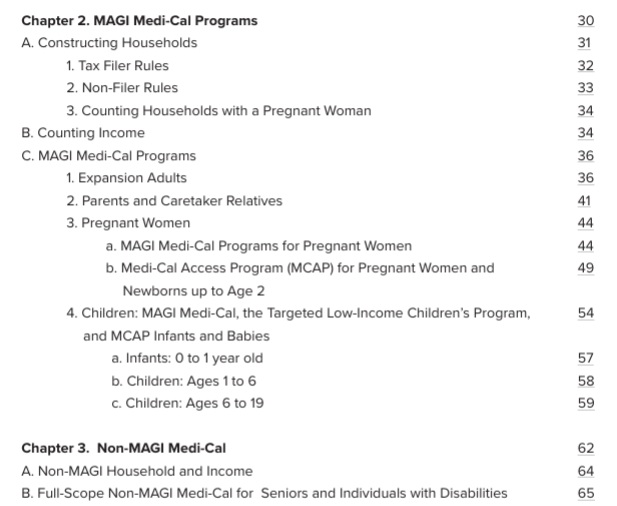
What’s on this page?
- Medi Cal Brochure
- Medi Cal Expansion to 138% of Federal Poverty Level
- Detailed explanation & rules from Western Poverty Law
- Mandate to report changes
- Monthly income qualification
- Free Tax Help
- Code of Federal Regulations
- When does Medi Cal coverage start?
- Annual Redetermination Benefits Cal.com Keep My Medi Cal dhcs.ca.gov WIC 140005.37 42 CFR §435.916
- Out of state emergency rules
- Our main webpage on Medicare
#My Medi-Cal
How to get the Health Care
You Need
24 pages
Smart Phones - try turning sideways to view pdf better
Eligibility
Undocumented, Illegal, Lawful Presence
DHCS.gov Medi Cal Immigrant FAQ on Eligibility
- Visit our webpage on Lawful Presence for Covered CA
- All undocumented Californians would still be covered for emergency medical and pregnancy care — so-called “limited scope” share of cost coverage that is paid for with federal dollars. But those who don’t enroll before January 2026 would be uncovered for other medical expenses, such as prescription drugs and doctor’s visits. Learn More >>> Cal Matters. org
- Main Email to Get a hold of Medi Cal --- [email protected]
- All inquiries related to Medi-Cal, including questions about terminating Medi-Cal coverage, must be referred to the beneficiary’s local county Social Services office.
- • Department of Health Care Services County Listings:
- • Covered California’s Medi-Cal page:.
- • Covered CA Toolkit Medi-Cal Reminders and When to Contact County Social Services:
- guide outlining information that certified enrollers can use when assisting Medi-Cal beneficiaries who may be eligible for and wish to enroll into a Covered California plan.
- dhcs.ca.gov/medi-cal/Contacts
- health care options.dhcs.ca.gov/contact-us
- Medi-Cal Rx Customer Service Center
- Department of Health Care Services Contacts
- [email protected] regarding general Medi-Cal eligibility.
- If the question contains specific details the county or the district office that handles your case must answer.
- Benefits Cal - Enrollment Website

- • Assisting Medi-Cal Eligible Consumers FAQ:
- frequently asked questions and glossary terms to understand the Medi-Cal enrollment process and learn how to seek help for various scenarios.
- California Department of Health Care Services 1-844-253-0883
- How-to Videos
Watch How-to Videos on setting up your account, uploading documents, submitting reports, and more. Benefits Cal.com - Non MAGI Medi Cal 1.916.345.8675
- [email protected] Ms. Leslie Benson
- IHSS In Home Supportive Services
- Ombudsman Webpage
- Phone: 1-888-452-8609
- Email: [email protected]
- The Office of Ombudsman cannot approve/terminate/reinstate Medi-Cal eligibility; alter aid codes, change/update addresses, change/update name or initiate inter-county transfers.
- Complex Questions Assistance
-
- Health Consumer Alliance at 1-888-804-3536.
- Disability Rights California at 1-800-776-5746.
- HICAP – Health Insurance Counseling & Advocacy Program
- CA Health Care Advocates – 1-800-434-0222 Volunteer counselors can help you understand your specific rights and health care options
- CA Health Care Advocates – 1-800-434-0222 Volunteer counselors can help you understand your specific rights and health care options
- Medi Cal Consulting Services
- National Center on Law & Elder Rights
- VITA Volunteers Income Tax Assistance
- Bet Zdedek Legal Services
- Medi Cal - Technical Comprehensive Reference Materials
- Our webpage on education, research & tutoring for a fee
- aging.ca.gov/Medicare_& Medi Cal Counseling
- Elder Care locator
- medi helper.com

- Pdf Brochure - I was told their fee is $3k
-
Medi Cal - #County Office Lookup
See our Main Webpage on Medi Cal contact information
Non MAGI Medi Cal
- dhcs.ca.gov/ Non MAGI Medi Cal
- Western Poverty Law - Non MAGI Medi Cal
- Benefits Cal How to report a change
-
- • Department of Health Care Services County Listings:
Contact Us - Ask Questions - Get More Information - Schedule a Zoom Meeting
[email protected]
By submitting the information below , you are agreeing to be contacted by Steve Shorr a Licensed Sales Agent by email, texting or Zoom to discuss Medicare or other Insurance Plans as relevant to your inquiry. This is a solicitation for Insurance
All our Health plans are Guaranteed Issue with No Pre X Clause
Instant Quote & Subsidy #Calculation
There is No charge for our complementary services, we are paid by the Insurance Company.
- Our Quote Engine Takes all the complexity out of using pencil and paper to figure out the premiums per the Obamacare/ACA rules under CFR §1.36B-3 *
- We are authorized Brokers for Dental, Vision & Covered CA get instant quotes direct and in Covered CA with subsidy calculation for:
- Watch our 10 minute VIDEO that explains everything about getting a quote
Visit our Main Webpage on Medi Cal Share of Cost & How to eliminate it
Benefits
Medical
Dental
Trump Big Beautiful Bill Changes
- Need Medicaid? Then Get a Job
- The deepest cuts to health care spending come from a proposed Medicaid work requirement, which is expected to end coverage for millions of enrollees who do not meet new employment or reporting standards.
- In 40 states and Washington, D.C., all of which have expanded Medicaid under the Affordable Care Act, some Medicaid enrollees will have to regularly file paperwork proving that they are working, volunteering, or attending school at least 80 hours a month, or that they qualify for an exemption, such as caring for a young child. The new requirement will start as early as January 2027.
- The bill’s requirement doesn’t apply to people in the 10 largely GOP-led states that have not expanded Medicaid to nondisabled adults.
- Health researchers say the policy will have little impact on employment. Most working-age Medicaid enrollees who don’t receive disability benefits already work or are looking for work, or are unable to do so because they have a disability, attend school, or care for a family member, according to KFF, a health information nonprofit that includes KFF Health News.
- State experiments with work requirements have been plagued with administrative issues, such as eligible enrollees’ losing coverage over paperwork problems, and budget overruns. Georgia’s work requirement, which officially launched in July 2023, has cost more than $90 million, with only $26 million of that spent on health benefits, according to the Georgia Budget & Policy Institute, a nonpartisan research organization.
- “The hidden costs are astronomical,” said Chima Ndumele, a professor at the Yale School of Public Health. Kff News *
- ICE is gaining access to trove of Medicaid records, adding new peril for immigrants
- Texing???
Medi Cal and Covered CA Eligibility FAQ’s webpage
- Unpacking the Unwinding: Medicaid to Marketplace Coverage Transitions Georgetown University 9/18/2024
- Medi-Cal to Covered California Enrollment Program Toolkit Covered CA 10/15/2024
- AI Summary
-
To move from Medi-Cal to Covered California, you must report the income change to your local county Medi-Cal office within 10 days because they manage Medi-Cal eligibility. After the county office updates your income and your Medi-Cal case is closed, they will often update your Covered California account for you, which may allow you to enroll in a new plan with a premium subsidy.Step 1: Report the change to your local county Medi-Cal office
- Contact your county social services or Medi-Cal office immediately. You can find a list of county offices on the DHCS website.
- You can report changes online through BenefitsCal.com or by calling your county office.
- Be prepared to provide proof of the income change, such as recent pay stubs or tax returns.
- Report this change within 10 days of the income increase.
Step 2: Wait for the county to update your case- The county office will process the change and determine if your income makes you ineligible for Medi-Cal.
- If you are found ineligible for Medi-Cal, the county office will close your case.
Step 3: Confirm your Covered California account is updated- Once your Medi-Cal case is closed, the county eligibility worker will often update the income information in your Covered California account to help facilitate your transition to a new plan.
- Check your Covered California account to see if your eligibility for subsidies has changed.
- If you have questions or don’t see the changes reflected in your account, call the Covered California Service Center at (800) 300-1506 for assistance.
- Resources & Links
- Comparison of Medi-Cal Benefits and Covered California Essential Health Benefits Health Law.org 12/2014
- The Medi-Cal Maze: Why Many Eligible Californians Don’t Enroll chcf.org 9/2021
- Can you get Medi Cal, Covered CA and Private Individual or Employer Group all at the same time? Visit our Dual Coverage Webpage
- Instant Covered CA and Direct Quotes
- Automatic Medi Cal when you get SSI Our webpage
Medi-Cal determines eligibility based on #monthly, not annual income.
- Even you you make $100k per year, but have a month with no income, you would qualify for MAGI Medi Cal
- This can even get you around the Open and Special Enrollment restrictions. That is, if you have a bad month, enroll, then when you get kicked out of Medi-Cal for making too much money, as you reported it, as required by law, within 10 days, thank G-d, you have a special enrollment into Covered CA or direct with an Insurance Company.
- No extra charge for us to help you enroll in Covered CA! Insure Me Kevin.com * Western Poverty Law * DHCS ACWDLS * 2015 Medi-Cal Eligibility Division Information Letters (MEDILs) * 15-03 *
- Medi-Cal Eligibility & Covered California – FAQ’s dhcs.ca.gov *
- Plain English from Covered CA Broker Department Email
- In regards to Medi-cal, they review monthly income.
- So if a client has been making $2000 a month and they do a report a change and it goes now to $1000 a month for 1 person, they will now be eligible for medi-cal.
- If the income goes back up to $2000 a month, they contact [report a change] Medi-cal and they are dis-enrolled from medi-cal and now are eligible for Covered CA. Response By Email (Argelia) (09/08/2016 11:56 AM)
- Get Instant Covered CA Quotes
- Our webpage on reporting changes in income, etc.
- If your income is borderline…you may well qualify for Silver 94 view chart very low net premium and rich benefits
- Scroll down and view the Income Chart
Medi-Cal Managed Care HMO – Health Care Options
Here you can review and choose the HMO that you want to deliver your Medi-Cal health Care.
- Get a lot more detail & analysis on Medi Cal HMO providers see our webpage on that
Learn more:
- Disability Rights.org –
- What are Medi Cal Managed Care Plans? What do I need to know?
- Medi-Cal Managed Care Health Plan Directory
- Medi-Cal Listing of HMO plans by county *
- Medi-Cal Managed Care Provider Search
- Medi Cal HMO – Managed Care Providers by County
- health care options.dhcs.ca.gov/tips-help-you-choose-medical-plan
- health care options.dhcs.ca.gov/frequently-asked-questions-faqs
- California’s County-Based Health Plans 2022 CHCF
- Medi-Cal’s Fragmented System Can Make Moving a Nightmare Read More CA Health Line *
- Poor Care Co-Ordination? New contracting process Deficient Oversight CA Health Line *
- Disability Rights – Medi Cal provider HMO’s, what are they? What do I need to know about them?
- Medi-Cal Managed Care – Health Care Options
- EOC’s, Forms & Income Charts from Insure Me Kevin.com
- Sacramento? dhcs.ca.gov//mmcd health plan dir
- Battle Lines Are Drawn Over California Deal With Kaiser Permanente
- Exemption from enrolling in a Health Care Plan
- health care options.dhcs.ca.gov – Download Forms
- You May Get A Medical Exemption If:
- You have a complex medical condition; AND
- The care you get from your Regular Medi-Cal doctor for the complex medical condition cannot be changed, because your condition could get worse; AND
- Your Regular Medi-Cal doctor is NOT part of a plan in your county. You may see more than one Regular Medi-Cal doctor. If you do, have the form filled out by the doctor who sees you most often. Ask your Regular Medi-Cal doctor if he or she is part of a Plan in your county. This should be done before you submit this form.
- You have a complex medical condition; AND
- Provider Search – Statewide Fee for Service
- See our webpage on IMR Independent Medical Review
- Medi Cal Explainers chcf.org/explainers
While you can have an employer or Indivudaul Plan and Medi Cal, there is However a
#MANDATORY Medi Cal Managed Care – HMO health
Enrollment
One must choose a Managed Care – HMO health plan – provider within 30 days after enrollment in Medi-Cal otherwise the State will pick plan for you. Medi-Cal Website Unless you have Other Health Coverage -OHC, then you must go Fee for Service.
When you have an HMO managed health care, the State of California makes a deal with health plans and pays a fixed amount each month per member enrolled in the plan – capitation. The HMO health plan is then responsible for providing you all your Medi-Cal services included under the EOC Evidence of Coverage. HMO Plans are required under state and federal law to maintain an adequate Medi-Cal provider network to ensure that each member has a primary care physician and must report on quality and access measures.
- Medi Cal Managed Care Find a Provider
- See the email we rec’d May 17th from Medi Cal to clarify some of these issues
- chcf.org/primary-care-matters * More readable summary * Health care systems with strong levels of primary care investment have better and more equitable health outcomes, lower care costs, and better care quality. We can build a healthier future for all Californians by focusing resources back to patients and their relationship with primary care providers.
#Clarification from Medi-Cal on
HMO Mandatory Enrollment and other coverage OHC
- What are the Medi Cal HMO’s doing to stop those with other coverage from enrolling?
- On this DHCS page, the public is told they must choose an HMO. Nothing is said about if you have other coverage, it’s excluded. [not mentioned on the DHCS page?]
The website above only applies to Medi-Cal beneficiaries who are required to enroll in a Medi-Cal managed care plan, which is the large majority of the Medi-Cal population.
- On or about 10.26.2020 the Medi Cal Ombudsman emailed and said that if one had private insurance they could NOT enroll in a Medi Cal Managed Care Plan!
If a Medi-Cal beneficiary has active other health coverage upon Medi-Cal enrollment, they are currently not eligible for enrollment into a managed care plan.
- When one has a Medi Cal HMO and other coverage – can the patient still pick which provider or plan to go to?
- When a member uses HMO services, how does the HMO collect & bill other coverage?
- When a member uses say his Employer’s HMO or PPO how does the collect copays & deductibles from Medi Cal HMO and/or fee for service?
The DHCS Health Insurance Premium Payment program does offer an option for a narrow population of newly enrolled Medi-Cal beneficiaries to receive reimbursement for OHC co-pays and deductibles for a limited time, subject to eligibility requirements. Please see dhcs.ca.gov for additional information.
- Of the four approaches to Managed Care & Third Party Liability on Medicaid.Gov which
is CA using?
- How is this being enforced & implemented?
CA currently uses the two out of four approaches:
You cannot choose a medical HMO Managed Care plan if:
You are a member of a commercial medical plan through private insurance Health Care Options DHCA.Gov * response from the Medi Cal Ombudsman * Western Poverty Law Page 5.219 * Medicaid.gov *
You must take Fee for Service.
Request for exemption from enrollment in Managed Care Plan, but I don’t see OHC as a reason
IEHP Provider manual seems to imply their HMO will allow it?
- EHP .org/manuals Medi-Cal
- 20 – Claims Processing (PDF)
See the email we rec’d May 17th from Medi Cal to clarify some of these issues
Visit our Webpage on Cal AIM Improvements?
Trump, whatever less coverage
FAQ’s
When does coverage #start?
- I applied for Medi-Cal but have not received any information from the county
- Medi-Cal will pay medical bills for 3 months prior to acceptance into medi-cal, but one must ask for retroactive coverage Western Poverty Law Center Page 5.211. * Excerpt of email from [email protected]
- Note that you can get immediate confirmation of provisional Medi-Cal enrollment when you apply direct or through an agent – at no additional charge on Covered CA’s website. If you scroll down on the eligibility page and find it.
- Scroll down for Other ways to get immediate medical care and more proof that you have coverage while waiting for your ID cards.
- Medi-Cal Eligibility & Covered California – FAQ’s DHCS.gov
- Hospital Presumptive Eligibility (PE) program
Documentation Required during
Covered CA 90 Day #Conditional Eligibility
A 90 day conditional eligibility notice means that you get coverage for 90 days even though Covered CA hasn’t verified that you qualify. As long as you send the proofs that are being asked for, everything is fine! There is NOTHING to worry about! Just comply. If you have trouble with compliance, email us.
Clients need to submit valid documentation for one or more of the following reasons:
- U.S. Citizen/National or non-citizen with a lawfully present status
- Income (MAGI Line 37*) Insure Me Kevin.com 2.19.2016
- Social Security Number (SSN)
- Incarceration Status – Insure Me Kevin.com
- American Indian/Alaska Native Status
You can upload, fax, send to their Certified Agent or mail their documentation. More than one document may be required.
View our Conditional Eligibility Quick Guide * or Job Aid for more information on the notice and to view a list of acceptable Verification Documentation.
Look for this sentence in the letter that you get from Covered CA.
We need your proof within 90 days. If we get a response and you prove your citizenship by the due date above, you will keep your insurance through Covered California.
Here’s the biggest lesson I learned in one year of law school. Read everything 3 times and when you think you understand it, read it again.
Resources & Links
- Medi-Cal’s website for Pending Applications & Newly Enrolled
- More Information – Covered CA Start Date – Conditional Eligibility
Medi Cal
out of state and #emergency coverage?
- CA Medi Cal – Out-of-state medical care is limited to the following:
- (a) (1) When an emergency arises from accident, injury or illness; or
- (2) Where the health of the individual would be endangered if care and services are postponed until it is feasible that he/she return to California; or
- (3) Where the health of the individual would be endangered if he/she undertook travel to return to California; or
- (4) When it is customary practice in border communities for residents to use medical resources in adjacent areas outside the State; or
- (5) When an out-of-state treatment plan has been proposed by the beneficiary’s attending physician and the proposed plan has been received, reviewed and authorized by the Department before the services are provided; and the proposed treatment is not available from resources and facilities within the State.
- (6) Prior authorization is required for all out-of-state services, except:
- (A) Emergency services as defined in §51056.
- “emergency services” means those services required for alleviation of severe pain, or immediate diagnosis and treatment of unforeseen medical conditions, which, if not immediately diagnosed and treated, would lead to disability or death.
- (B) Services provided in border areas adjacent to California where it is customary practice for California residents to avail themselves of such services. texas.gov/medicaid
- Medi Cal Treatment Authorization Request
- 540-1 (a) (5) When an out-of-state treatment plan has been proposed by the beneficiary’s attending physician and the proposed plan has been received, reviewed and authorized by the Department before the services are provided; and the proposed treatment is not available from resources and facilities within the State
- (A) Emergency services as defined in §51056.
- Medi Cal only covers outside of CA for emergencies and very special circumstances. Cornel Law *
- Sources
- cdss.ca.gov/Medi-Cal-Out-of-State-Coverage
- casetext.com/section-51006-out-of-state-coverage
- Cornel Law
-
- California Advancing and Innovating Medi-Cal (CalAIM) is a long-term commitment to transform and strengthen Medi-Cal, offering Californians a more equitable, coordinated, and person-centered approach to maximizing their health and life trajectory.
- Medicaid.gov
- Disability Benefits 101
- Western Poverty Law Center Guide
- Medi-Cal enrollees not sure how to use coverage california health line.org
- Medi-Cal pays $415 to $575/month or MORE to HMO’s to take care of you Learn More⇒ Insure Me Kevin.com 3.4.2016 5.11.2014
- Medi Cal Explained CHCF
- Medi-Cal Facts and Figures, 2024 Edition Gives a lot of information on ALL Health Insurance Programs
- chcf.org/cal aim-resources-
- cal matters.org/medi-cal-eligibility/
- dhcs.ca.gov/Budget-Highlights
- ebudget.ca.gov/Full Budget Summary
-
Prescription drugs.
- Hearing Aid Cap FAQ’s
- Health screenings for kids
- Preventive and wellness services and chronic disease management.
- Mental Health CHCF Fact Sheet
- Substance abuse CHCF Article
- Maternity
Ongoing Care & Recovery
- Personal care services (IHSS)
- Nutrition Food & Meals
More Details
- My Medi-Cal brochure
- dhcs.ca.gov/Medi-Cal_EHB_Benefits
- dhcs.ca.gov/Benefits_services.aspx
- dhcs.ca.gov/Benefits-Chart
- Check with your HMO Providers Evidence of Coverage
- Insure Me Kevin.com – Medi Cal HMO same coverage as Covered CA HMO! Provider list may differ!
-
Medi Cal Renewal
Much more on Medi Cal
- Medi Cal Explained CHCF
- More
- Historical Guide 2006 CHCF 174 pages
- Cal AIM California Advancing and Innovating Medi-Cal — is a far-reaching, multiyear plan to transform California’s Medi-Cal program and to make it integrate more seamlessly with other social services. The goal of CalAIM is to improve outcomes for the millions of Californians covered by Medi-Cal, especially those with the most complex needs.
- You Tube Videos
- DHCS.CA.Gov
- chcf.org/focus-on-cal aim
- VIDEO Introduction to Medi Cal Los Angeles DPSS
- California voters give Medi-Cal doctors a raise by passing Prop. 35
- 10 Essential Health Benefits
- Video
- Our Webpage on Medi Cal Benefits
- Denti Cal
******************************************
- Western #Poverty Law – Exact Legal Rules on Coverage for Low Income Californian’s
Nolo Social Security, Medicare, Medi Cal & Government Pensions
-
Our Webpage on COVID 19
- CA State Senator Steven Bradford 35th District
- His Webpage on COVID 19 Resources
-
BIC Benefits Identification Card
FAQ’s “C-CHIP County Children’s Health Initiative Program”
- The County Children’s Health Initiative Program (C-CHIP) sccgov.org a health insurance program (Medi-Cal) that offers affordable and comprehensive medical, dental, and vision insurance for children age 0-19 who qualify. Qualification is in 3 Northern CA counties and is for those who are just out of the normal Medi Cal income limits 266-322% Federal Poverty Level (FPL).
- Learn more by clicking on the links below:
FAQ’s
- How does Covered California work with Medi-Cal?
- Covered California will act as a “one-stop shop” for health insurance. Through Covered California, you will be able to apply for Medi-Cal benefits electronically and receive a real-time eligibility results. You will also be able to report changes online and receive real-time customer support 24 hours a day. dhcs.gov More FAQ’s DHCS ♦ Insure Me Kevin.com
- Disability Benefits 101 – Medi-Cal The Details
- What is California Advancing and Innovating Medi-Cal (CalAIM)
- Cal Aim is a long-term commitment to transform and strengthen Medi-Cal, offering Californians a more equitable, coordinated, and person-centered approach to maximizing their health and life trajectory.
- Goals of CalAIM
- 1. Identify and manage comprehensive needs through whole person care approaches and social drivers of health.
- 2. Improve quality outcomes, reduce health disparities, and transform the delivery system through value‑based initiatives, modernization, and payment reform.
- 3. Make Medi-Cal a more consistent and seamless system for enrollees to navigate by reducing complexity and increasing flexibility. DHCS *
- why doesn’t medi-cal really help? So long on #hold, so much wasted time?
-
- Why is my website so much more informative than Medi-Cals or Covered CA’s?Medi-Cal like any other “business” wants to expand. So they have a motive to keep you there. The Co-Pays and deductibles are lower. They include adult dental & vision.Medi-Cal and the Insurance Companies don’t pay agents, yet it’s just as time consuming and complex to help people with Medi Cal as a Covered CA or direct plan!
- Here’s links on why Government workers are lazy:
- If you like waiting on hold with Covered CA – Stay there. If you would like to just send an email and I’ll take care of it, appoint me as your agent and I’ll see what I can do.
- Why is my website so much more informative than Medi-Cals or Covered CA’s?Medi-Cal like any other “business” wants to expand. So they have a motive to keep you there. The Co-Pays and deductibles are lower. They include adult dental & vision.Medi-Cal and the Insurance Companies don’t pay agents, yet it’s just as time consuming and complex to help people with Medi Cal as a Covered CA or direct plan!
- It’s been a whirlwind deciding what to do, health-insurance-wise and, after a consultation with our tax guy, we’ve decided to register for Medi-cal. I know you get no money from this, so I’m sorry for wasting your time with Oscar Insurance inquiries. Thank you for all of your help. We’ll be in touch in the future if, as we hope, we can make enough money to get back on CC.
Effective Date? Temporary Instant ID Card”
-
- Benefits Cal is a one-stop-shop to apply for…
- Cal Fresh
- Ages 26 through 49 Adult Full Scope Medi-Cal Expansion regardless of immigration status
- Cal WORKs
- Medi-Cal
- CMSP (County Medical Services Program)
- Disaster Cal Fresh
- GA/GR (General Assistance and General Relief )
- Briefing — Medi-Cal Explained: An Overview of Program Basics
- chcf.org/medi-cal-explained/
- #BenefitsCal is a one-stop-shop to apply for…
- Medi-Cal
- County Medical Services Program (CMSP),
- Food Assistance – Cal Fresh (formerly known as Food Stamps)
- How to use Eat Fresh.org VIDEO
- Cooking & Nutrition
- California Work Opportunity and Responsibility to Kids (CalWORKs) or check their other website
- Medi-Cal
-
Here you can review and choose the HMO that you want to deliver your Medi-Cal health Care.
- Benefits Cal is a one-stop-shop to apply for…
-
BIC Benefits Identification Card
Medi Cal & Seniors
- Medi-Cal is California’s Medicaid program, which provides health insurance to individuals and families who earn low incomes, including 40% of the state’s children, half of Californians with disabilities, and over a million seniors. In total, the program covers more than 12 million people, or nearly one in three Californians.
- Medi-Cal also covers a large number of working Californians, many of whom became eligible for the program because of the Affordable Care Act’s Medicaid expansion. Working Californians may be one of the least recognized or understood populations served by the program. In a 2018 poll, 42% of Californians said that they believed that most working-age adults without a disability enrolled in Medi-Cal are unemployed. Twenty percent said they didn’t know. This report combines key findings from survey data with insights from 19 in-depth interviews with enrollees to paint a more accurate and complete picture of working Californians who rely on Medi-Cal, why they came to enroll in the program, and the role it plays in their lives.
- VIDEO
- Working Californians Enrolled in Medi-Cal Share Their Stories
- Chcf Policy at a Glance
Links & Resources
- california healthline.org/illegal resident-expansion
- kff health news.org/morning-breakout/californians-face-long-wait-times-when-calling-medi-cal-analysis-finds/
- https://www.chcf.org/publication/medi-cal-facts-and-figures-2024-edition/
- https://www.chcf.org/blog/medi-cal-considers-income-not-assets-enrollees/
- FAQ Medi Cal Rx
https://medi-calrx.dhcs.ca.gov/cms/medicalrx/static-assets/documents/faq/Medi-Cal_Rx_Members_FAQ.pdf - Medi Cal for illegal aliens…
- https://www.dhcs.ca.gov/services/medi-cal/eligibility/Pages/Adult-Expansion.aspx
- https://www.dhcs.ca.gov/services/medi-cal/eligibility/Pages/youngadultexp.aspx
- https://www.dhcs.ca.gov/services/medi-cal/eligibility/Pages/OlderAdultExpansion.aspx
- https://www.dhcs.ca.gov/services/medi-cal/Pages/Medi-CalFairHearing.aspx
- https://healthconsumer.org/wp/wp-content/uploads/2017/04/cs032WorkingDisabled.pdf
- https://insuremekevin.com/magi-medi-cal-income-eligibility-for-2023-increases-over-6/
- https://www.dhcs.ca.gov/services/medi-cal/eligibility/Pages/youngadultexp.aspx#:~:text=This%20initiative%2C%20called%20the%20Young,DHCS)%20website%20for%20SB%2075
- https://www.coveredca.com/learning-center/information-for-immigrants/deferred-action-for-childhood-arrival/
- https://khn.org/morning-breakout/cms-proposes-rules-to-ease-enrollment-in-medicaid-chip/
- https://insuremekevin.com/medi-cal-bridging-the-gap-for-adults-26-49-years-old/
- https://www.shouselaw.com/ca/defense/fraud/medi-cal-fraud/
- https://www.desertsun.com/story/news/health/2022/05/03/california-expands-medi-cal-services-undocumented-seniors/9620961002/
- Our webpage on child support & medi cal
- https://www.chcf.org/wp-content/uploads/2019/03/MediCalExplainedEligibilityEnrollment.pdf
- https://www.chcf.org/wp-content/uploads/2019/03/MediCalExplainedEligibilityEnrollment.pdf
- https://www.chcf.org/wp-content/uploads/2019/02/MediCalExplainedPaymentManagedCarePlansCurrentProcessChallenges.pdf
- Newsom Wants to Expand Medi-Cal to All Undocumented Immigrants by 2024. Advocates Say They Need It Soonerhttps://www.sacbee.com/news/politics-government/capitol-alert/article262935493.html
- Disability Rights CA Medi Cal Resources
- Medi-Cal Info on Covered CA Website
- wikipedia.org on Medi Cal
- Mental Health
- Eligibility
- Payments to HMO’s
- Medi Cal budget
- Insurers make billions off Medicaid in California during Obamacare expansion LA Times 11.5.2017
-
ObamaCare – #Expansion to 138% of FPL
-
Assembly Bill 1 ** Senate.bill.1.
- If you don’t have free Medicare Part A
- Work Requirements
Child - Subpages
- Aged and Disabled Federal Poverty Level Program
- Share of Cost – Eliminate with Dental, Vision Medi Gap Insurance Premiums
- Appeals Medi Cal
- Calculate Instantly Medi Cal Share of Cost and Zero it out!
- FAQ’s Share of Cost
- How to upload documents to BenefitsCal.com
- How to use medical expenses to lower share of cost
- IHSS In Home Supportive Services
- Medi Gap to lower share of cost Medi Cal IHSS
- Timing & Redetermination Medi Cal Share of Cost
- SSI – Supplemental Security Benefits – Automatic Medi Cal – SSDI
- Share of Cost – Eliminate with Dental, Vision Medi Gap Insurance Premiums
- Dual Coverage?

















https://ktla.com/news/california/california-bill-seeks-to-restore-medi%e2%80%91cal-coverage-for-undocumented-adults-in-2027/
https://www.instagram.com/p/DVMR_XHEbz6/?igsh=MzRlODBiNWFlZA==
https://healthconsumer.org/access-coverage/
My son has medi-cal
I lost his card and need a replacement
Do it through your Benefits.Cal account or through the automated system at 888-472-4463
Source