Appeals, complaints or grievances with an Insurance Company?
Introduction
The process of appeals & grievances gets very technical, legal, etc. I won’t even attempt to summarize it here. Please follow the links below, guides & summaries to the right, check your policy – evidence of coverage and check the law.
Medical Procedures?
- Was your procedure Medically Necessary?
- Independent Medical Review IMR
- Did you use the Correct MD or hospital – Provider List and
- Did you Review the procedures in your actual policy, evidence of coverage?
Reasons why the Claim might be denied
- Did you tell the truth on your application?
- Nearly 15% of claims submitted to private payers are initially denied
- Insurers’ denial rates — a critical measure of how reliably they pay for customers’ care — remain mostly secret to the public. Federal and state regulators have done little to change that.
- Claims Denials and Appeals in ACA Marketplace Plans in 2021 kff.org
- Wrestling With a Giant: How to Dispute a Hospital Bill
- Here’s where they write to your MD, prior to ACA/Obamcare before a claim is even turned in.
- How about doing a pros & cons spreadsheet – Ben Franklin method? It’s important to know the other sides point of view and potential arguments & evidence.
- Billing Codes – Satire or how it really works?
- Was the policy in force? Lapse non pay?
- Department of Labor on Filing a Health Claim
- Most U.S. adults don’t know they can fight insurance denials, new study finds
Insurance Company & Regulatory Agency
Grievance Procedures & Forms
- Check your EOC – Evidence of Coverage for procedures & where to get forms.
- Aetna
- Blue Cross Grievance Procedures
- Notice
- Blue Shield – General Info. Appeals & Grievances PO Box 629007 El Dorado Hills , CA 95762 – 9007 Fax: (916) 350 – 7585
- CA Department of Insurance
- IMR – Independent Medical Review
- REQUEST FOR REVIEW Molina Health Care OF CANCELLATION, RECISSION, OR NONRENEWAL OF HEALTH CARE SERVICE PLAN BENEFITS
- hhs.gov/curbing-insurance-cancellations
- DGS Office of Administrative Hearings
- Kaiser Member Grievance Form
- #Appeal Guides
- DOI Washington State
- Navigating the Appeals Process -Patient Advocate Foundation
- NAIC Sample Appeals letter & process
- VIDEO Clark Howard - How to appeal
- LA Times appeal explanation 1.19.2022
- Kantor & Kantor Attorneys VIDEO
CA #SmallClaims Court Guide 56 Pages
Gathering the documents you need
- courts.ca.gov/selfhelp-smallclaims
- Nolo Guide to Small Claims in CA
- California Small Claims – Court Site – Self Help
- Fillable Forms
- Small Claims Adviser Los Angeles 213.974.9759
- If you have a claim for more than the Small Claims Limit, you can sue, but you waive the amount over the limit.
-
Small Claim Court Study Guide for temporary – pro tem judges – highly likely you might have an attorney whose volunteering to be a Judge for the day.
Department of Consumer Affairs - Mediation Request ONLINE
How Mediation Works & Paper Mediation Request Form
- Fair Shake.com Arbitration - They will send a demand letter!
Appeals? Grievances?
Check the FULL policy, EOC - Evidence of Coverage Also, here's a guide in how to read and interpret contracts. that's what an Insurance Policy is.
Then if you do decide to do an appeal, (page 151 in specimen policy) or view our webpage on appeals, you'll know what to argue about.
See our main webpage on appeals & grievances
Consumer Links & Resources
- How to gather documents to prove your case – Small Claims Manual
- Prove you never got a letter?
- How to tell your story, timeline and background
- How to create a TIMELINE in Word, Excel, PowerPoint
- Health Net faces suit over refusal to cover treatments LA Times 9.13.2012
- Appeal Guide – Washington State Department of Insurance 62 pages pdf
- Nolo – Medical Malpractice Basics
- Todd Friedman, Esq. can help if debt collectors are harassing you when you don’t owe the $$$
- Find an Attorney
- Health Consumer Alliance HCA
Part of Department of Managed Health Care - Patient Advocate.org
- Health Consumer Alliance
- Center for Health Care Rights
- National Association of Health Care Advocacy
- California Health Consumer Advocacy Coalition
- CA Health Care Advocates
- HICAP
- Legal Brief Blue Shield allegations about Narrow Networks
- Los Angeles Times how to fight back
- Register an account with CDSS
Reasons to file a Claim
Procedures
#Reasons for filing a Covered CA appeal
Your eligibility notice explains what you are eligible for and the programs for which you do not qualify. Depending on your eligibility results, you may appeal any of the following (check as many boxes as you would like):
- I was denied enrollment into a Covered California health plan
- The amount of Premium Assistance (tax credits that help pay my monthly premium) is not correct – Get Calculation
- The level of Cost Sharing Reduction (help paying my out of pocket expenses) is not correct
- I was denied eligibility for an exemption from the individual responsibility CA Mandate Penalty
- Covered California did not process my information in a timely manner
- Covered California stated that I am not a US Citizen or US National or a lawfully present individual living in the United States
- Covered California stated that my application was incomplete
- I do not have other health coverage (such as free Medi-Cal or employer sponsored insurance) that prevents me from qualifying for insurance through Covered California
- Covered California stated that I am not a California Resident
- Covered California stated that I did not pay my premiums by my due date
- Covered California stated that my MAGI income is too low chart to qualify for Covered California coverage Get Calculation
- Other Tell us more about why you disagree with Covered California’s decision. You may attach additional sheets of paper if you need more space to write. Covered CA Appeals Request Form *
We STRONGLY suggest you attach additional sheets of paper and explain your case, with citations, evidence & exhibits. Be sure to read all the helpful aids we have on this page. You are going up against well versed opponents!
Resources & Links
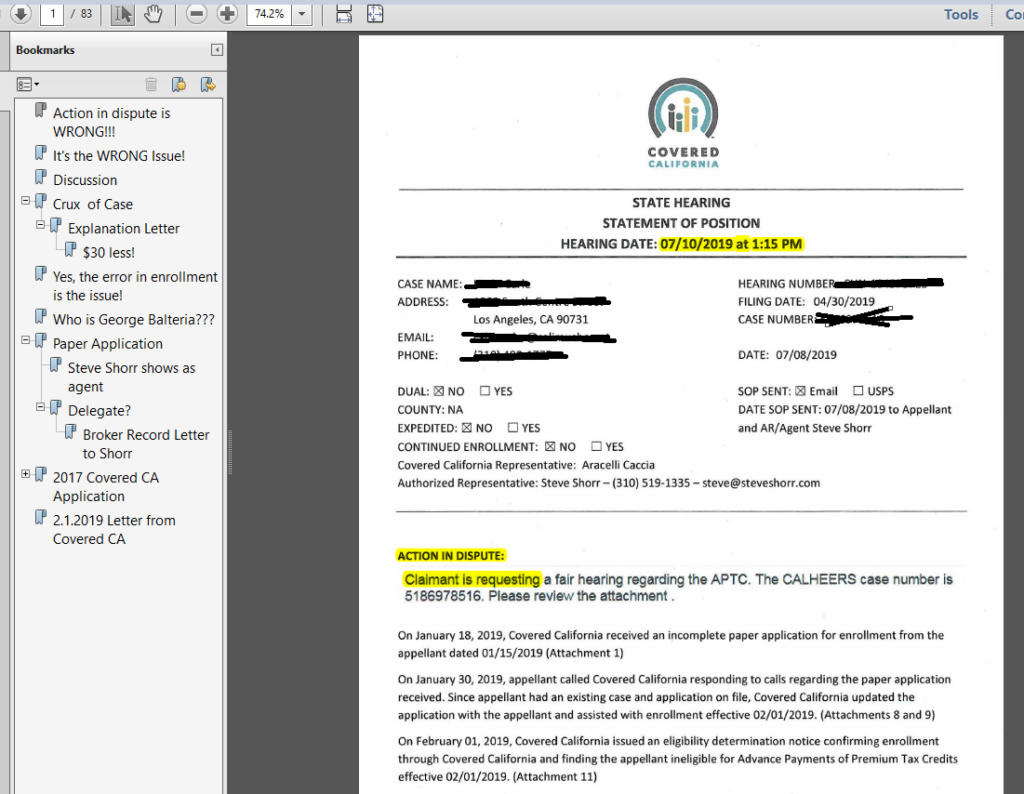
Cover Page for Covered CA’s Brief to the Administrative Law Court
Administrative Law – Prepare to Win
Writing a better brief – Law Repository – UAir University
CDSS State Hearings Division’s Decision Registry – Read prior cases – names are redacted
Covered CA Appeals Decision #Polk Case
- Sample Letter for Appeal
- Explanation on Insure Me Kevin . com - Polk Case
- Check out where administrative law judge said he wished he could make Covered CA pay the costs of their bogus advise but didn't have that authority
- Doesn't matter what Covered CA says, it's what the IRS says Form 8962 attaches to Form 1040
California Administrative Procedure Act 119 pages
Overview of Administrative Hearing Procures 12 pages
Western Center on Law & Poverty
1. Medi-Cal Eligibility Appeals
a. Notice: Content and Timing Requirements
b. Requesting a Fair Hearing
c. Expedited Hearings
d. Retaining Benefits During the Fair Hearing Process – Aid Paid
Pending
e. Informal Resolution
f. Dismissals
g. Setting and Notice of Hearing; Position Statement
h. The Fair Hearing
i. After the Fair Hearing
2. Covered California Eligibility Appeals
a. Notice: Content and Time Requirements
b. Request for Hearing
c. Expedited Appeals
d. Eligibility Pending Appeal – Continuing Enrollment
e. Informal Resolution
f. Notification of Hearing and Position Statement
g. The Fair Hearing
h. Hearing Decision and Other Post-Hearing Processes
a. Shared Appeals Entity
b. Informal Resolution Process
c. The Fair Hearing
4. Medi-Cal Access Program (MCAP) Eligibility Appeals
California Code of Regulations
Article 7. Appeals Process for the Individual Exchange
-
§ 6600. Definitions.
- § 6602. General Eligibility Appeals Requirements.
- § 6604. Notice of Appeal Procedures.
- § 6606. Appeal Requests.
- § 6608. Eligibility Pending Appeal.
- § 6610. Dismissals.
- § 6612. Informal Resolution.
- § 6614. Hearing Requirements.
- § 6616. Expedited Appeals.
- § 6618. Appeal Decisions.
- § 6620. Appeal Record.
- § 6622. Employer Appeals Process.
Medicare Appeals
How to file #Medicare appeals, deal with issues, claims, problems, etc.
- Medicare Appeals can get complex, so we won’t really try to summarize it. Please review the brochures, information and links below and on your right. Appeals are a complex subject we are giving you mostly official guides and not our summary, advise or essays.
- Medicare Complaint Form on Medicare.Gov
- See also Fillable pdf 10287 pdf
- How to file a complaint – Medicare.Gov
- Medicare Advantage – Livanta
- Medicare Appeals Publication # 11525 60 pages
- Rights & Appeals for Part D Rx – Guide to Rx # 11109
- Medicare Rights & Protections Publication 11534
- File complaint against Medicare itself?
- Medicare Contact Info * More * Forms *
- HICAP CA * Rest of USA * (Health Insurance Counseling and Advocacy Program) provides free, confidential one-on-one counseling, education, and assistance to individuals and their families on Medicare, Long-Term Care insurance, other health insurance related issues, and planning ahead for Long-Term Care needs. HICAP also provides legal assistance or legal referrals in dealing with Medicare or Long-Term Care insurance related issues.
- HICAP counselors are trained in Medi-Cal and Medicare and can help you understand the complex insurance options to find the best fit for you. You can also learn about Medicare or Medi-Cal by attending community presentations or conferences conducted by HICAP counselors. Medicare & You – see link in side panel
- ***Sure they might be of help, but how much training, licensing, malpractice coverage and experience do licensed agents have. Look at all the information on this site!
- HICAP counselors are trained in Medi-Cal and Medicare and can help you understand the complex insurance options to find the best fit for you. You can also learn about Medicare or Medi-Cal by attending community presentations or conferences conducted by HICAP counselors. Medicare & You – see link in side panel
- National Center on Law & Elder Rights – Case Consultation for Professionals
- Sample Evidence of Coverage – Medicare Advantage
- This is NOT sales literature, but is provided as a public service for educational purposes.
Medicare Technical & Research Links
Medicare Claims Processing Manual Technical 319 Pages
One hour webinar by an attorney, on how to do claims & appeals – You Tube
42 CFR Part 422, Subpart M – Grievances, Organization Determinations and Appeals
- § 422.560 — Basis and scope.
- § 422.561 — Definitions.
- § 422.562 — General provisions.
- § 422.564 — Grievance procedures.
- § 422.566 — Organization determinations.
- § 422.568 — Standard timeframes and notice requirements for organization determinations.
- § 422.570 — Expediting certain organization determinations.
- § 422.572 — Timeframes and notice requirements for expedited organization determinations.
- § 422.574 — Parties to the organization determination.
- § 422.576 — Effect of an organization determination.
- § 422.578 — Right to a reconsideration.
- § 422.580 — Reconsideration defined.
- § 422.582 — Request for a standard reconsideration.
- § 422.584 — Expediting certain reconsiderations.
- § 422.586 — Opportunity to submit evidence.
- § 422.590 — Timeframes and responsibility for reconsiderations.
- § 422.592 — Reconsideration by an independent entity.
- § 422.594 — Notice of reconsidered determination by the independent entity.
- § 422.596 — Effect of a reconsidered determination.
- § 422.600 — Right to a hearing.
- § 422.602 — Request for an ALJ hearing.
- § 422.608 — Medicare Appeals Council (MAC) review.
- § 422.612 — Judicial review.
- § 422.616 — Reopening and revising determinations and decisions.
- § 422.618 — How an MA organization must effectuate standard reconsidered determinations or decisions.
- § 422.619 — How an MA organization must effectuate expedited reconsidered determinations.
- § 422.620 — Notifying enrollees of hospital discharge appeal rights.
- § 422.622 — Requesting immediate QIO review of the decision to discharge from the inpatient hospital.
- § 422.624 — Notifying enrollees of termination of provider services.
- § 422.626 — Fast-track appeals of service terminations to independent review entities (IREs).
Medicare #Appeals 11525
- Livanta ONLINE Appeal System
- AHA wants False Claims Act enforcement of Medicare Advantage care denials Modern Health Care 5.20.2022 See also Beckers Hospital Review
- False Claims Act - Whistle Blower.com

Filing an appeal with Medicare
- Official Medicare Advantage Plan Appeals VIDEO
- How to Appeal a Denial of your Health Claim - VIDEO Kantor & Kantor Attorneys
- Medicare Appeals Fact Sheet – CA Health Care Advocates Hi Cap
- See our other page on appeals
- the exact proper terms.
- Grievance—A complaint about the way your Medicare health plan or Medicare drug plan is giving care. For example, you may file a grievance if you have a problem calling the plan or if you’re unhappy with the way a staff person at the plan has behaved towards you. However, if you have a complaint about a plan’s refusal to cover a service, supply, or prescription, you file an appeal.
- Appeal—An appeal is the action you can take if you disagree with a coverage or payment decision made by Medicare, your Medicare health plan, or your Medicare Prescription Drug Plan. You can appeal if Medicare or your plan denies one of these:
■ Your request for a health care service, supply, item, or prescription drug that you think you should be able to get
■ Your request for payment for a health care service, supply, item, or prescription drug you already got
■ Your request to change the amount you must pay for a health care service, supply, item or prescription drug
You can also appeal if Medicare or your plan stops providing or paying for all or part of a health care service, supply, item, or prescription drug you think you still need. - medicare.gov/Appeals.pdf
- Will see how my Appeal for a TKR now goes, since I’ve met the qualifications of “conservative treatments” over the course of the last 2-3 years!!!
- Please when using technical terms, define them and provide a URL.
/cgsmedicare.com/
-
-
Medicare Billings And Claims
- G-001-Organizing Your Medical Bills – 07-19-12
- G-002-How Medicare Claims Are Processed – 07-19-12
- G-003-Instructions For Creating a Claims Record – 07-19-12
- See our webpage on
- Medicare Appeals & Grievances
- Fraud
- Attorneys - We don't know them... Found on Google
- Medicare Appeals & Grievances
-
#Attorney 's that can help you through the Social Security Disability maze
- west coast disability.com/
- CA State Bar Attorney Referral Service
- Legal Match.com
- Sellers Law
- Hill & Ponton
- premier disability.com
- Cantrell & Green
- We don't necessarily know these attorney's...
- Editorial: Lawyers are fighting innovative proposals for more affordable legal assistance. That’s wrong LA Times 1.30.2022
- We don't necessarily know these attorney's...
Medi Cal Appeals
#Medi-Cal Appeal & Hearing Rights
Health Care Services and Benefits
- Medi-Cal Fair Hearing Dhcs.ca.gov
- You have the right to ask for an appeal if you disagree with the denial of a health care service or benefit.
- If you are in a Medi-Cal managed care plan and you get a Notice of Action letter telling you that a health care service or benefit is denied, you have the right to ask for an appeal.
- You must file an appeal with your plan within 60 days of the date on the Notice of Action. After you file your appeal, the plan will send you a decision within 30 days. If you do not get a decision within 30 days or are not happy with the plan’s decision, you can then ask for a State Fair Hearing. A judge will review your case. You must first file an appeal with your plan before you can ask for a State Fair Hearing. You must ask for a State Fair Hearing within 120 days of the date of the plan’s written appeal decision.
- If you are in Fee-for-Service Medi-Cal and you get a Notice of Action letter telling you that a health service or benefit has been denied, you have the right to ask for a State Fair Hearing right away. You must ask for a State Fair Hearing within 90 days of the date on the Notice of Action.
- You also have the right to ask for a State Fair Hearing if you disagree with what is happening with your Medi-Cal application or eligibility. This can be when:
- • You do not agree with a county or State action on your Medi-Cal application
• The county does not give you a decision about your Medi-Cal application within 45 or 90 days
• Your Medi-Cal eligibility or Share of Cost changes Eligibility Decisions
- • You do not agree with a county or State action on your Medi-Cal application
- If you get a Notice of Action letter telling you about an eligibility decision that you disagree with, you can talk to your county eligibility worker and/or ask for a State Fair Hearing. If you cannot solve your disagreement through the county, you must request a State Fair
Hearing within 90 days of the date on the Notice of Action. You can ask for a State Fair Hearing by contacting your local county office. You can also call or write to:- California Department of Social Services
Public Inquiry and Response
PO Box 944243, M.S. 9-17-37
Sacramento, CA 94244-2430
1-800-743-8525, (TTY 1-800-952-8349) - You can also file a hearing request online at:
- cdss.ca.gov/hearing-requests
- California Department of Social Services
- If you believe you have been unlawfully discriminated against on the basis of sex, race, color, religion, ancestry, national origin, ethnic group identification, age, mental disability, physical disability, medical condition, genetic information, marital status, gender, gender identity, or sexual orientation, you can make a complaint to the DHCS Office of Civil Rights.
- You can learn how to make a discrimination complaint in “Federally Required Notice Informing Individuals About Nondiscrimination and Accessibility Requirements” on page 21.
- About State Fair Hearings
- The State will tell you it got your hearing request. You will get a notice of the time, date and place of your hearing. A hearing representative will review your case and try to resolve your issue. If the county/State offers you an agreement to solve your issue, you will get it in writing.
- You can give permission in writing for a friend, family member or advocate to help you at the hearing. If you cannot fully solve your issue with the county or State, you or your representative must attend the State Fair Hearing. Your hearing can be in person or by phone. A judge who does not work for the county or Medi-Cal program will hear your case.
- You have the right to free language help. List your language on your hearing request. Or tell the hearing representative you would like a free interpreter. You cannot use family or friends to interpret for you at the hearing.
- If you have a disability and need reasonable accommodations to fully take part in the Fair Hearing process, you may call 1-800-743-8525 (TTY 1-800-952-8349).
- You can also send an email to To get help with your hearing, you can ask for a legal aid referral. You may get free legal help at your local
legal aid or welfare rights office MyMedi-Cal Pamphlet *
#My Medi-Cal
How to get the Health Care
You Need
24 pages
Smart Phones - try turning sideways to view pdf better
-
- More explanation

- Enroll with Benefits Cal
- What is Medi Cal - VIDEO
-
How to VIDEO
-
Medi-Cal Managed Care HMO – Health Care Options
- Benefits Cal is a one-stop-shop to apply for...
- Cal Fresh
- Ages 26 through 49 Adult Full Scope Medi-Cal Expansion regardless of immigration status
- Cal WORKs
- Medi-Cal
- CMSP (County Medical Services Program)
- Disaster Cal Fresh
- GA/GR (General Assistance and General Relief )
- Briefing — Medi-Cal Explained: An Overview of Program Basics
- chcf.org/medi-cal-explained/
- #BenefitsCal is a one-stop-shop to apply for...
- Medi-Cal
- County Medical Services Program (CMSP),
- Food Assistance - Cal Fresh (formerly known as Food Stamps)
- How to use Eat Fresh.org VIDEO
- Cooking & Nutrition
- California Work Opportunity and Responsibility to Kids (CalWORKs) or check their other website
- Medi-Cal
-
Here you can review and choose the HMO that you want to deliver your Medi-Cal health Care.
-
BIC Benefits Identification Card
Customer Service – Enforcement
Enforcement
Anthem Blue Cross Fined $415K since the California Department of Managed Health Care said it found 40 cases in which Anthem deprived members of their grievance and appeal rights. – CA Healthline 5.3.2016
WOW!!! 2.8 Million June 2019 CA Managed Health Care * Insure Me Kevin.com *
Dealing with Customer Service Issues
- First and foremost, be polite. These are crazy days as well for service reps, nearly all of whom aren’t to blame for their companies’ penny-pinching practices. A little civility goes a long way.
- Don’t be shy about escalating. Front-line service reps are frequently not given the power to resolve matters on their own and will often give an unsatisfactory response. Ask to speak with a supervisor.
- If that doesn’t work, write to the company’s chief executive or president, detailing the nature of the problem and providing as much documentation as possible. Most big companies have special dispute-resolution departments at senior levels.
- Be persistent. If it becomes clear that you’re not going away, some companies will finally throw in the towel and offer the response you’re seeking. Squeaky wheels and all that. LA Times 8.8.2020 *
#SNAFU - Situation Normal - All Fouled Up

I learned the word SNAFU Situation Normal, All Fouled Up in the dorm, when I attended San Diego State in the early 70's and earned a degree in Insurance. In all that time, I've never been able to use the word in a sentence, until last 10.1.2013, when Covered CA.com, Health Care.Gov nor the Insurance Company Websites or my own Quote Engine that I pay around $250/month for were supposed to launch, but did not do it properly.
Unauthorized Practice of Law
What is the #unauthorized practice of law?
Unlawful Practice of Law [§6125 – 6133]
California broadly defines the “practice of law” as dispensing legal advice or service, even if the advice or service does not relate to any matter pending before a court. * Legal Advice vs Legal Information * Shouse Law * (Mickel v. Murphy (1957) 147 Cal.App.2d 718, 721.) Davis Stirling.com * Advising HOA boards on how the statutes pertain to them or what actions would violate the law or the governing documents. * Supreme Court opinion. * Davis Stirling.com *1. Advising HOA boards about rights, duties and liabilities. That includes but is not limited to:
- Interpreting the Davis-Stirling Act,
- Interpretation of contract provisions,
- Disputed maintenance and repair issues,
- Settlement issues.
2. Preparing documents that alter rights, duties and liabilities. Managers and management companies can prepare documents that are incidental to the regular course of their business. Anything beyond that must be prepared by legal counsel. That includes but is not limited to:
- Amendments to CC&Rs, Bylaws, and Articles of Incorporation,
- Contracts and contract provisions,
- Election rules,
- Rules enforcement policies,
- Settlement agreements, and Davis Stirling.com *
What is “#Advice?”
Legal advice refers to the written or oral counsel about a legal matter that would affect the rights and responsibilities of the person receiving the advice. In addition, actual legal advice requires careful analysis of the law as it applies to a person’s specific situation – as opposed to speculation based on generic facts. From a legal standpoint, the giving of legal advice is tantamount to the practice of law, In a nutshell, legal advice has the following characteristics:
- Requires legal knowledge, skill, education and judgment
- Applies specific law to a particular set of circumstances
- Affects someone’s legal rights or responsibilities
- Creates rights and responsibilities in the advice-giver
Unlike legal information – such as information posted on a street sign – legal advice proposes a specific course of action a client should take. For instance, it’s the difference between telling someone what to do (legal advice) as opposed to how to do it (legal information). Examples:
- Selecting, drafting, or completing legal documents or agreements that affect the legal rights of a person
- Negotiating legal rights or responsibilities on behalf of a person
- Speculating an outcome
- Selecting or filling out specific forms on behalf of a client Findlaw.com *
Webster Definition
The hourly rates for HOA lawyers typically range from $175 to $350, whereas legal advice from a manager is free. It is understandable that boards would try to save money by seeking free legal counsel from their managers. However, doing so exposes directors to significant risk. By statute, directors are protected from personal liability for errors in judgment if they follow the Business Judgment Rule, which requires that decisions by directors be:
- In good faith,
- In a manner which the director believes to be in the best interests of the corporation, and
- With such care, including reasonable inquiry, as an ordinarily prudent person in a like position would use under similar circumstances. (Corp. Code §7231(c).)
If a board relies on legal counsel from a manager and things go awry, directors will have difficulty convincing a jury that seeking legal advice from a manager was prudent. Davis Stirling.com Los Angeles County Bar Assoc. – lacba.org
Legal Document Assistant
It is unlawful for any person engaged in the business or acting in the capacity of a legal document assistant or unlawful detainer assistant to do any of the following:
(d) Provide assistance or advice which constitutes the unlawful practice of law pursuant to Section 6125, 6126, or 6127.
(e) Engage in the unauthorized practice of law, including, but not limited to, giving any kind of advice, explanation, opinion, or recommendation to a consumer about possible legal rights, remedies, defenses, options, selection of forms, or strategies. §6411 *
Links & Resources
- hirealawyer.findlaw.com/
- 12 page booklet from CA Courts Legal Advice vs Legal Information
- California State Bar – File a Complaint
- California Bar – Cease & Desist Notices
- Supreme Court of Florida Ruling
County of Los Angeles
District Attorney
*****************
Technical Stuff for Attorneys
Appeals Law
§155.505 General eligibility appeals requirements.
§155.510 Appeals coordination.
§155.515 Notice of appeal procedures.
§155.525 Eligibility pending appeal.
§155.535 Informal resolution and hearing requirements.
§155.555 Employer appeals process.
Interim Final Rules for Group Health Plans and Health Insurance Issuers Relating to Internal Claims and Appeals and External Review Processes Under the Patient Protection and Affordable Care Act
- June 22, 2011 CMS-9993-IFC2: Group Health Plans and Health Insurance Issuers: Rules Relating to Internal Claims and Appeals and External Review Processes – Opens in a new window
- July 26, 2011 CMS-9993-CN: Group Health Plans and Health Insurance Issuers: Rules Relating to Internal Claims and Appeals and External Review Processes; Correction – Opens in a new window (PDF – 184 KB)
From CMS Site
- Regulations & Guidance
- Fact Sheets & FAQs
- Letters & News Releases
- State External Appeals Review Processes
Resources, Child Pages & Links
- Insure Me Kevin.com
- Patient Advocate.org
- Prove you never got a letter?
- Medical Necessity Grievances
- Appeal & Grievances?
#Advocates Guide to Surprise Medical Bills
- Hidden Cost of Surprise Medical Bills 3.3.2016 Time Magazine
- heart bypass surgery, replacement of one valve and repair of another. raging infection that required powerful IV antibiotics to treat. spent a month in the hospital, some of it in intensive care, before she was discharged home.
- surprise: Bills totaling more than $454,000 for the medical miracle that saved her life. Of that stunning amount, officials said, she owed nearly $227,000 after her health insurance paid its part. Time.com 3.21.2019 *
- heart bypass surgery, replacement of one valve and repair of another. raging infection that required powerful IV antibiotics to treat. spent a month in the hospital, some of it in intensive care, before she was discharged home.
- Newscast about Hospitals being required to post rates - charges VIDEO
- PBS Trump Price Transparency Executive Order VIDEO
- Our webpage on Balance Billing & No Surprises
- Americans often "forced" to pay medical bills they don't owe, feds say CBS News
- Colorado's Supreme Court has ruled in favor of a woman who expected to pay about $1,300 for spinal fusion surgery but was billed more than $300,000 by a suburban Denver hospital that allegedly included charges it never disclosed she might be liable for. Read more: CBS News 5.19.2022
- What the Federal ‘No Surprises Act’ Means in California
- CA Department of Insurance Summary
Technical Links – Appeals & Grievances
Page 19 Section §2719 of Health Care Reform -Appeals Process
45 CFR Part 147 Interim Final Rules for Group Health Plans and Health Insurance Issuers – Appeals
§ 147.136 — Internal claims and appeals and external review processes.
7/26/2011 – Final Rules – EBSA – Group Health Plans and Health Insurance Issuers: Rules Relating to Internal Claims and Appeals and External Review Processes; Correction [PDF]
More Final Rules for EBSA
§10123.13. (a) Every insurer…shall reimburse claims …, whether in state or out of state, … as soon as practical, but no later than 30 working days after receipt…
(b) If an uncontested claim is not reimbursed … within 30 working days…interest shall accrue and shall be payable at the rate of 10 percent per annum …
Search & Find CPT Current Procedural Terminology codes and their relative values at CPT Code/Value Search – Medicare Billing Codes This is a free site for patients and consumers.
See also Medical Necessity
California Insurance Code §790.03 (h) Knowingly committing or performing with such frequency as to indicate a general business practice any of the following unfair claims settlement practices: Calif. Code of Regulations TITLE 10. CHAPTER 5 ADOPT SUBCHAPTER 7.5 with new 2004 amendments on CA Department of Insurance Site
Claim Splitting Res Judicata
Claim Splitting – #Res Judicata
you can’t just sue someone two or more times to get around the small claims court limit.
Laws Against
Claim Splitting – Preclusion – Res Judicata
You Tube Video’s on Res Judicata (Double Jeopardy)
- Rule:
- If judgment is rendered in favor of a plaintiff in a particular suit, the plaintiff is precluded from raising claims (in any future litigation) which were raised in (or could have been raised) in that lawsuit.
- Elements:
- Before a court will apply the doctrine of res judicata to a claim,three elements must be satisfied:
- There must have been prior litigation in which identical claims were raised (or could have been raised). In general, claims are sufficiently identical if they are found to share a “common nucleus of operative fact.”
- scope:
- Res judicata bars relitigating of claims that were previously litigated as well as claims that could have been litigated in the first lawsuit. sparknotes.com lectlaw caught.net
- Before a court will apply the doctrine of res judicata to a claim,three elements must be satisfied:
If your claim is over the small claims monetary limit,you may file a case in the regular superior court, where you can either represent yourself or hire an attorney to represent you. Instead of doing that,you may choose to reduce the amount of your claim and waive(give up) the rest of the claim in order to stay within the small claims court’s monetary limit on claims. Before reducing your claim, discuss your plans with a small claims adviser or an attorney. Once the dispute is heard and decided by the small claims court, your right to collect the amount that you waive will be lost forever.
Definition – Claim Splitting lectlaw.com Dividing a single or indivisible claim or cause of action into separate parts and bringing separate suits upon it, either in the same court , or in separate courts or jurisdictions.
Res Judicata
You cannot divide a claim into 2 or more claims (called claim splitting) just to avoid the limit…..Or, lower the amount you ask for and give up (or waive) the rest. That way you can keep your claim in Small Claims court.
.occourts.org
fees charged by the attorney for private assistance are not recoverable as court costs or damages. (dca.ca.gov)
Small Claims Procedures & Practices
§6.14 Res Judicata
Under the doctrine of res judicata, a small claims court judgment is a bar to a second suit on the same cause of action. [Pitzen v Superior ; Allstate Ins. Co. v Mel Rapton, Inc. (2000) 77 CA4th 901, 905.] * Allstate v Rapton – waiver of damages over $5k limit,
A small claims judgment for a plaintiff, however, is not given collateral estoppel issue-preclusion effect on other actions against the defendant. It would be unfair to have plaintiff’s choice of small claims court bind the defendant when the record does not fully reflect the issues raised and decided there. [Sanderson v Niemann]
But a defendant may raise collateral estoppel issue preclusion if the defendant prevailed in a previous small claims action. There is no rationale for refusing to afford collateral estoppel effect to issues litigated and decided against a plaintiff. Fundamental fairness dictates that a plaintiff who chose to litigate in small claims court cannot cite the informality of that forum to gain a second chance to litigate a decided issue. Relitigating decided issues is also inconsistent with the public policy that a small claims plaintiff is bound by an adverse judgment. [Bailey v Brewer; Pitzen v Superior Court] §6.14 Res Judicata
If you do try to unlawfully collect a debt by claim splitting – you might get busted under Fair Debt Collection Laws!
FAQ’s
FAQ’s
- I’m having a problem finding a lab that’s approved by my Insurance Company. It’s not clear if the lab in the same medical group IPA where my doctor PCP is. I’m waiting to hear back.
- What if my illness gets worse?
- One thing we have to be careful of, is not to let your illness get worse. There is a duty to mitigate your damages, not to let your health get worse. Insurance Companies are NOT your parents! IMHO they are not responsible for your health. You have a simple contract to pay them a premium and if you have a claim, they have to pay what the contract – policy says. IMHO people don’t want to take responsibility. They want someone else to be in charge. Like having the Government take over?
- injury victims often fail to mitigate their damages is in seeking medical treatment. An injured person should seek reasonable medical treatment for any injuries that he or he has suffered. If a delay in seeking medical treatment exacerbates the injuries and causes further harm, or if delays in seeking treatment lead medical costs to increase, the victim may not be able to recover the additional damages for the added harm.
- For example, a pedestrian may suffer a broken arm when she is hit by a car. If she delays getting the break set, and it then heals incorrectly, causing her extended pain and the eventual medical bills to increase, she cannot recover for the increase in damages.
- duty to mitigate requires only that the plaintiff made reasonable efforts and expenditures to resolve, lessen, and otherwise minimize their injuries and the suffering caused by such injuries.
- You should always take reasonable steps towards resolving your injuries and the suffering caused by your injuries, for three reasons:
- 1) for your own well-being, you should pursue proper medical care and therapy as soon as possible;
- 2) you are entitled to damages for any expenditures put towards reasonable mitigation efforts; and
- 3) if you do take reasonable steps to mitigate, then the defendant will have an excellent defense argument that may ultimately reduce their damages liability and leave you with a much smaller damages award. Kopp Law *
- Jury Instructions Mitigate Damages
- You should always take reasonable steps towards resolving your injuries and the suffering caused by your injuries, for three reasons:
- Check out our tools to find providers for most Insurance Companies in CA
.
.
- I recently had an appt appointment to establish care with a #primary physician after 3 yrs without. Various tests were done to assess my current health.
- I was surprised that all were not covered as part of a well woman visit or as preventative screenings.
- A test for Hep C antibodies was covered but the Hep C detection test was not.
- Blood test for lipids and triglycerides was covered but not for other blood chemicals.
- I would suspect both were necessary to provide a health profile.
- The Dr. noticed a bulge of sorts by my naval so she ordered an Abdominal Aortic Aneurysm ultrasound which was not covered.
- The AAA test is covered under the Affordable Care Act and I met four of the risk factors for checking so why was that not considered preventative screening.
- I have filed a grievance but wonder if there’s more info I need to submit from the Doctor as to why the various tests were done.
- We are talking about what ACA defines as preventative care. Not “establishing” care or “assessing current” health.
- Here’s what is listed as preventative care:
- healthcare.gov
- Blue Shield’s List
- Our Webpage on Preventative Care
- Screenings and other services are covered with no deductible for adults and children with no current symptoms or history of a health problem. Specimen Policy Page 92
- If one has history or symptoms, then it’s covered under the diagnostic benefit Page 74 Subject to Co-Pays & the Deductible.
- Maintenance of a known problem, like those listed below as common risk factors, is certainly preventative, but isn’t defined that way under ObamaCare and is subject to the regular co-pays and deductibles. Peter Lee of Covered CA thinks that’s a BIG problem, read more by on the link. Annual physicals may not be a benefit LA Times 8.2.2016
- Medical Necessity
- Clinical Guidelines Blue Shield .
.
.
- Here’s what is listed as preventative care:
- My Medicare Advantage plan, with United Health Care denied coverage for a home health care nurse who came to our house two or three days a week for almost four months.
- I was being treated by Wound Care at Mission Hospital in Asheville, NC. Because I live 75 miles away from them, the doctors authorized a home health nurse and had me come in one day each week and later every other week.
- It was a great service since my husband is 88 and cannot drive the 150 mile round trip and my injury was to my right ankle so I was not supposed to be driving long distances.
- I have read that Medicare Advantage plans often deny this coverage although Medicare provides it.
- Any advice for appealing this???
- Well let’s research the issue first:
- Surgical dressing services
- Medicare Part B (Medical Insurance) covers medically necessary treatment of a surgical or surgically treated wound.
- Your costs in Original Medicare
- You pay 20% of the Medicare-approved amount for your doctor’s or other health care provider’s services. You pay a fixed Copayment for these services when you get them in a hospital outpatient setting. The Part B deductible applies. You pay nothing for the supplies. https://www.medicare.gov/coverage/surgical-dressing-services
- UHC Bulletin on Wound Care This bulletin is beyond our paygrade… Try the links above.
- Home health aide services: Medicare will pay for part-time or intermittent home health aide services (like personal care), if needed to maintain your health or treat your illness or injury. Medicare doesn’t cover home health aide services unless you’re also getting
- skilled care. Skilled care includes:
- ■ Skilled nursing care
- ■ Physical therapy
- ■ Speech-language pathology services
- ■ Continuing occupational therapy, if you no longer need any of the above
- Medicare & Home Health Care # 10969
- Medicare Benefit Policy Manual
- Medstarvna.org Wound Care at Home
- Medically Necessary – means health care services, supplies, or drugs needed for the prevention, diagnosis, or treatment of your sickness, injury or illness that are all of the following as determined by us or our designee, within our sole discretion:
- • In accordance with Generally Accepted Standards of Medical Practice.
- • Most appropriate, in terms of type, frequency, extent, site and duration, and considered effective for your sickness, injury, or illness.
- • Not mainly for your convenience or that of your doctor or other health care provider.
- • Meet, but do not exceed your medical need, are at least as beneficial as an existing and
- available medically appropriate alternative, and are furnished in the most cost-effective manner that may be provided safely and effectively.
- Home Health Aide – A home health aide provides services that don’t need the skills of a licensed nurse or therapist, such as help with personal care (e.g., bathing, using the toilet, dressing, or carrying out the prescribed exercises). Home health aides do not have a nursing license or provide therapy.
- Home Health Care – Skilled nursing care and certain other health care services that you get in your home for the treatment of an illness or injury. Covered services are listed in the Benefits Chart in Chapter 4, Section 2.1 under the heading “Home health agency care.” If you need home health care services, our plan will cover these services for you provided the Medicare coverage requirements are met. Home health care can include services from a home health aide if the services are part of the home health plan of care for your illness or injury. They aren’t covered unless you are also getting a covered skilled service. Home health services don’t include the services of housekeepers, food service arrangements, or full-time nursing care at home.
- Medically Necessary – Services, supplies, or drugs that are needed for the prevention, diagnosis, or treatment of your medical condition and meet accepted standards of medical practice. Our webpage on Medical Necessity
- Medicare-Covered Services – Services covered by Medicare Part A and Part B. All Medicare health plans, including our plan, must cover all of the services that are covered by Medicare Part A and B.
- Prior Authorization – Approval in advance to get covered services or certain drugs that may or may not be on our drug list (formulary). Covered services that need prior authorization are marked in the Benefits Chart in Chapter 4. Covered drugs that need prior authorization are marked in the formulary.
- Send me copies of your actual bills and the denials… It doesn’t look hopeful at this time. Did you follow the appeals procedure for UHC?
.
.
- I have a dental claim that was denied as the Insurance Company says I didn’t have 12 months of coverage as mandated in the policy.
-
A 12-month waiting period applies to all Major Services Page 1 of EOC
My first appeal was denied as the Appeals Review said:
You have requested that xxx Insurance Company waves the waiting period and reprocess the claims referenced below to allow benefit coverage. We are unable to approve your request.
During the research of your concerns it was determined that the waiting period has not been satisfied. As stated in your plan’s Evidence of Coverage (EOC) there is a 12-month waiting period before xxx Insurance will pay for major services.
I want to file another appeal, as the Insurance Company should have it in their records that I’ve had continuous coverage since 2014. The appeals court should find in my favor as the Insurance Company should just pay me, as their records should show that!
-
- I don’t think so. The Insurance Company has clearly stated in unequivocal terms that you had a lapse in coverage from 9.30.2019 to 8.1.2020!
- Sure, their records are wrong as you have cancelled checks and I have my commission statements. If you’re going to take this to Appeals, Complaints with Department of Managed Health Care or Small Claims Court, the burden of proof is on you.
- Please review the Appeals Guides above.
- Here’s some excerpts:
- It is important to remember that you do have rights which are described in your insurance policy handbook.
- A health insurance policy is a contract between you, the policy holder, and the insurance company. A denial is a “contract dispute,” and your appeal must be based both on the reason for the denial and provisions in your insurance policy, contract
- Your health insurance plan must notify you in writing of the reason they did not authorize a specific request or denied payment of a service as well as how to appeal their decision
- One of the most important elements of your appeal packet is a clear, concise letter that addresses very specifically the reason of the denial, and incorporates the terms of your policy (or plan language). Patient Advocate.org
- Gathering the Documents You Need
- Prepare for the hearing by gathering any evidence that will help the judge understand the case. Your evidence may include any written contract, receipt, letters, written estimates, repair orders, photographs, canceled checks, account books, advertisements, warranties, service contracts, or other documents. Like your Insurance Brokers Commission Statements. Small Claims Guide
- Please also review these other pages on our website:
- Read the policy, denial letters and other correspondence like where the Insurance Company said that your coverage was lapsed three times and then when you think you understand it, read it again.
- Our webpage on the important of reading the EOC Evidence of Coverage
- Court case stating a policyholder must read their policy.
- Insurance Companies give the wrong answer and then tell the Department of Insurance that an application was never sent in, when they told the agent it would be denied and not sent in
- I’m not practising law or giving legal advice. I’m just showing you research.
- We are not interested in what someone is alleged to have told someone else over the phone
- Don’t get caught off guard at the appeals hearing or small claims court, make sure you have the evidence that the Insurance Company will show to defend their denial of your claim
- Nah, Steve,
- You’re wrong. I didn’t have to do all the work you said. Blue Shield is paying my claim!
- we have approved your request for payment of claims on September 7, 2020 and September 14, 2020, for $737.00 per claim
- >
- Sorry, no.
- Please read the entire letter:
It is important to understand that this decision has been made on an exception basis and, in making this decision, Blue Shield does not waive any of its rights to enforce the provisions of the enrollee’s health plan. Your dental plan requires that you have continuous coverage for 12 months prior to any major dental services are covered. You had two months of coverage from August 1, 2020 through September 30, 2020
- Let’s be clear what exception means:
- The definition of an exception is something that is outside of the rules or outside of the normal expectations.
- An example of an exception is when you are normally supposed to be home by midnight but your parents let you stay out until 1 AM, just for one night.
- There will be no exceptions to this rule.
- I ask that you grant an exception in this case
- I understand my current policy is not obligated to pay for this, but I would like to request an exception.
- Health Insurance Appeals and Exception Guide
- Thus, if you have any more claims for major work, it WILL NOT be paid!







https://cahealthadvocates.org/beneficiaries-will-have-the-right-to-appeal-hospital-observation-status-next-year/
https://www.dol.gov/agencies/ebsa/about-ebsa/our-activities/resource-center/publications/filing-a-claim-for-your-health-benefits
Yeah!!!! You did it!!! I’m so thankful!!!
You are not superman but SuperSteve!!!!!
You have done the impossible!!!
I know I know, I shouldn’t be celebrating until I get the insurance. Even coming this far was impossible for me. Without your help, I would have just accept their decision and gone without insurance for a year. I either would have used our savings to pay for surgery or have to wait until next year while suffer the consequences.
I couldn’t thank you enough. I’m so grateful to you.
Thank you for the Kudo’s.
Here’s the Draft Appeals Brief had we needed to actually go before the Judge. All your personal information has been redacted
If I lost a small claims court lawsuit against a auto repair shop, can I still file a lawsuit against the mechanics?
I filed a small claims lawsuit against a auto shop for the cost I paid for a procedure I was not happy with. I lost my lawsuit because the commissioner said before he even heard the case, that he knew nothing about auto repairs and unless I had brought an expert witness, which I did not, he was going to rule against me.
My question is, can I file another lawsuit for the same thing ( repair bills) against the mechanics who performed the bad repair. Even though they have their own licenses they are actual employees of the shop. And they did come to court to testify for the shop in the lawsuit I lost.
would this be considered res judicata?
1st off, I can’t give you legal advise. You are not asking Insurance Advise. I’ll see if I can point to something in the law or the guides for you.
Did the Judge say dismissed with or without prejudice? That is, did he say you could come back to court with an expert witness. I presume not, from your question, the case was dismissed with prejudice, meaning you can’t bring the case up again – like double jeopardy in a criminal trial.
The general rule is that a plaintiff who has prosecuted one action against a defendant and obtained a valid final judgment is barred by res judicata from prosecuting another action against the same defendant Upcounsel.com
The mechanics didn’t bill you, the shop did. So, wouldn’t that be the same thing? You’re still suing on the exact same invoice.
I’m sorry, I don’t find a black & white reference for you. See all the information on Small Claims on this website and
Try calling the Small Claims Advisor in your area Los Angeles 213.974.9759
My Insurance Company requires that claims be reported within 90 days. My doctor didn’t meet the deadline, what can I do?
Here’s what we found in the Health Net Bronze PPO Enhanced Care:
GENERAL PROVISIONS
NOTICE OF CLAIM: Written notice of claim must be given to Us within 20 days after the occurrence or commencement of any covered loss, or as soon thereafter as reasonably possible
PROOFS OF LOSS: Written proof of loss must be furnished to Us at P.O. Box 9040, Farmington, MO 636409040, in case of claim for loss for which this Policy provides any periodic payment contingent upon continuing loss, within 90 days after the end of the period of time for which claim is made; in the case of claim for any other loss, written proof of loss must be furnished within 90 days after the date of the loss. Failure to furnish such proof within the time required will not invalidate or reduce any claim if proof is furnished as soon as reasonably possible. Except in the absence of legal capacity, however, We are not required to accept proofs more than one year from the time proof is otherwise required.
****************
Google Research
Investigate when claim was filed, etc. etc. with your doctor and insurance company… Nerdwallet
**********
what if the doctor’s office fails to file the insurance claim?
What if the doctor files the claim after the normal 90-day insurance claim deadline?
Do I still owe the doctor for services that would have been covered under insurance but, due to the negligence of the doctor’s office, are now unpaid?
appeal the coverage denial. In life, the squeaky wheel gets the oil. Start squeaking.
Obtain a copy of the late claim filed with the insurance company and a copy of the coverage denial letter. The court will be interested in seeing a letter denying an untimely claim submitted by the very doctor who assigned the debt to a bill collector.
If you do not receive an Explanation of Benefits within 60 days of seeing a doctor, assume something is wrong and contact your insurer and the doctor’s office.
Sam Turco Law
Steve,
My check has cleared … they should have it in there records… the last time the same thing… it was received and posted but the account was not updated …. November check has also been sent
is it so hard to call the carrier and say… “my client is listed as cancelled yet you have received payments…can you tell me why the account is listed as cancelled or what is needed to correct the matter”
…seems simple and fast…or would you rather wait until I search through cancelled checks to “prove” what is already known?
I really don’t like the telephone to deal with anything of a business matter. I much prefer email. When we approach an Insurance Company I like to follow the advice given above and get all our facts and ducks in a row first and be able to clearly express it to the Insurance Company and if need be to show clear concise emails, documents, cancelled checks, whatever is relevant to the Judge or regulatory authorities.
The reply from the Insurance Company to your email clearly shows the point I’m trying to make.
I have had many problems sense I was injured
I have been a victim of medical malpractice
and my lawyer also had taken advantage of me even with all my notes and complaining to everyone I could think too
I got ignored and with all my problems
took long to be able to feel like I can think and healed about all I am going to now
I suffer and am in desperate need to have answers
my medical records where compromised leaven me to suffer and
my lawyer faild me and destroyed all hope for me
I was double charged and now I can’t work
waiting for disability
We are sorry to hear of your troubles. Did you have a question for us?
I STARTED a POLICY ON FEB 1 EFFECTIVE DATE AND [I] CANCELLED MY POLICY DUE TO UNHAPPY SERVICES ON MARCH 2
THEN WHY DO THEY WAIT TO TERMINATE ME UNTIL APRIL AND DO NOT GIVE ME A REFUND OF MY MONEY .
1st off, you probably upset the Insurance Company, using all caps in your correspondence with them. Net Manners.com
2nd I had to read your email several times and do major edits before I could understand your question.
3rd – I don’t know what kind of a policy you are talking about.
I will assume it’s individual health insurance. In our speciment policy page 22 it says that the agreement is monthly. Thus, when you cancel on March 2nd, you are covered for the rest of March and the policy can cancel the last day of March, NOT March 2nd.
See also the explanation of Monthly premiums on page 32.
See page 34 on the effective date of termination, which clearly says termination is the last day of the billing period that your termination was received.