California Based Health Insurance
Emergency and Urgent Care, ONLY? when Traveling?
Introduction
How does my California Coverage work out of Area?
- What coverage is there under a California issued Health Policy, when you need:
-
- Emergency or Urgent Care
- Out of CA – Not an Emergency or Urgent? Like if you want to seek out specialists at prestigious world famous clinics and hospitals
-
- Find the EOC Evidence of Coverage for YOUR Insurance Company
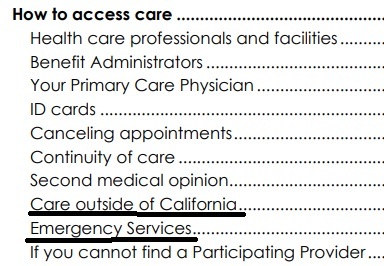
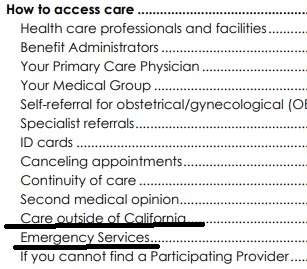
- Blue Shield PPO Table of Contents
-
- Out of your HMO Service Area?
- Outside of USA?
- Learn more and enroll in International Travel Insurance.
- Medicare outside of USA
- Note – Employer Group Plans appear MUCH more liberal!
-
CA Insurance Company Travel Guides
- Kaiser – KP.org Travel Care away from home * 951-268-3900 *
- Provider Finder for all our companies
- Sharp
- sutter health plus.org/care-while-traveling
- Free Quotes, Brochures and complete information on travel coverage and International Medical Plans
- Medicare.Gov/Travel
- $50k Emergency Coverage in Medi Gap aka Supplemental & Medicare Advantage Plans - Check your EOC! See our section on Medicare Below
- California Medi Cal rules on out of area coverage
- Constitutional right to travel from one state to another 14th Amendment
#Insubuy Travel Health Insurance
Instant Quotes, Details and ONLINE Enrollment
Steve talks about International Travel Insurance VIDEO
US State Department - Travel - Insurance
Our webpage on Travel Insurance
Definition Urgent Care and #Emergency Services
Emergency Medical Condition
An illness, injury, symptom (including severe pain), or condition severe enough to risk serious danger to your health if you didn’t get medical attention right away. If you didn’t get immediate medical attention you could reasonably expect one of the following:
1) Your health would be put in serious danger; or
2) You would have serious problems with your bodily functions; or
3) You would have serious damage to any part or organ of your body. Health Net Glossary *
Urgent Care
Care for an illness, injury, or condition serious enough that a reasonable person would seek care right away, but not so severe as to require emergency room care.
Prior Authorization – Preauthorization
- A decision by your health insurer or plan that a health care service, treatment plan, prescription drug or durable medical equipment (DME) is medically necessary. EOC * Our Webpage * Sometimes called prior authorization, prior approval or precertification. Your health insurance or plan may require preauthorization for certain services before you receive them, except in an emergency. Preauthorization isn’t a promise your health insurance or plan will cover the cost. Health Net Glossary * Our webpage on Prior Authorization *
Be sure to check the definition in YOUR EOC
Links related to Urgent & Emergency Care Definition
- Urgent Care vs ER
- Emergency Room – Obligation to treat uninsured patients
- Emergency Room – Balance Billing
- Health Net Provider Networks & Search
- Definitions – Glossary
- Providence Health – Difference between ER and Urgent Care
- Viewpoints: Insurance Companies Can Drop Patients Whenever; Choosing Between Doctor Vs. Urgent Care KFF
Specimen Individual Policy #EOC with Definitions
Employer Group Sample Policy
It's often so much easier and simpler to just read your Evidence of Coverage EOC-policy, then look all over for the codes, laws, regulations etc! Plus, EOC's are mandated to be written in PLAIN ENGLISH!
- Find your own Individual EOC Evidence of Coverage
- It' important to use YOUR EOC not just stuff in general!
- Obligation to READ your EOC
- Plain Meaning Rule - Plain Writing Act
- Our Webpage on Evidence of Coverage
- OOP Out of Pocket Maximum - Many definitions are explained there.
VIDEO Steve Explains how to read EOC
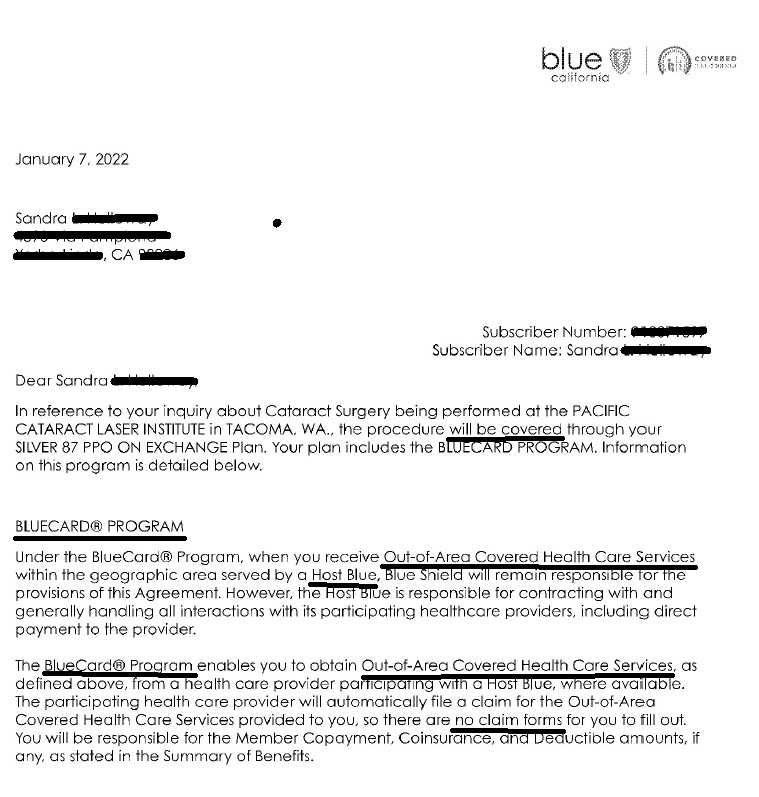
Blue Shield INDIVIDUAL Plans
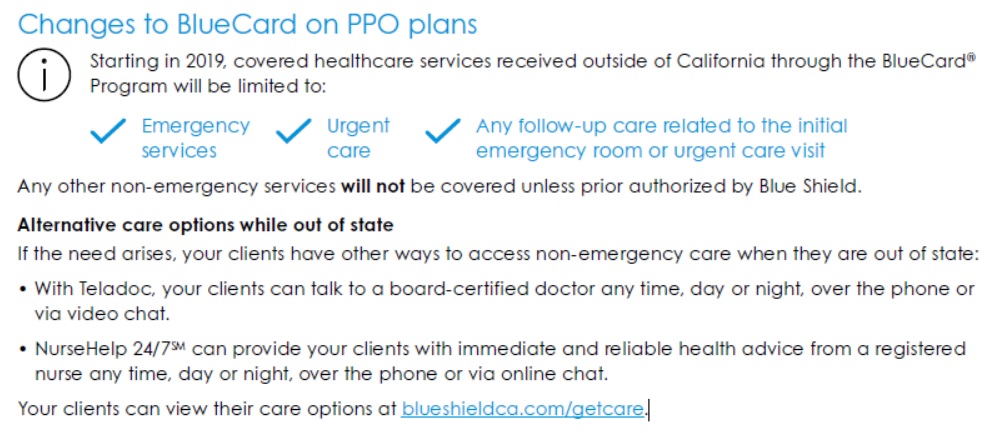
Unauthorized Excerpt of Confidential Agent Guide
Blue Shield BlueCard Program frequently asked questions
Going to Urgent Care vs ER Emergency Room
What if you’re out of the area, out of state?
Visiting an urgent care center can cost up to five times less than a visit to the ER and significantly reduce your wait time. While the average wait at a California ER is 4 hours and 34 minutes, urgent care center wait times are usually under an hour*. That means you can bypass the crowds and take your first step on the road to recovery.
- 49 Ways to stay out of the ER – Emergency Room Kevin MD.com
-
Why CA Insurance Companies limited out of area – CA to urgent and emergency only
Too Many Claims
BlueCard Program for Doctors & Hospitals
& Inter plan Arrangements -
for members traveling out of state & outside of the united states
Excerpt from Typical EOC Evidence of Coverage
Out-of-area services
- Blue Shield has a variety of relationships with other Blue Cross and/or Blue Shield licensees. Generally, these relationships are called Inter-Plan Arrangements and they work based on rules and procedures issued by the Blue Cross Blue Shield Association. Whenever you receive health care services outside of California, the claims for those services may be processed through one of these Inter-Plan Arrangements described below.
- When you access health care services outside of the Plan Service Area, you will receive the care from one of two kinds of providers.
- Most providers are participating providers and contract with the local Blue Cross and/or Blue Shield licensee in that other geographic area (Host Blue). S
- home providers are non-participating providers because they do not contract with the Host Blue. Blue Shield’s payment practices in both instances are described below and in the Introduction section of this Agreement.
- This Blue Shield plan provides limited coverage for health care services received outside of the Plan Service Area. Out-of-Area Covered Health Care Services are restricted to
-
- Emergency Services,
- Urgent Services, and
- Out-of-Area Follow-up Care.
- Any other services will not be covered when processed through an Inter-Plan Arrangement unless prior authorized by Blue Shield. Please see the Medical Management Programs section for additional information on prior authorization and the Emergency Benefits section for information on emergency admission notification.
- View YOUR actual EOC - It's YOUR EOC Policy that rules, not what you read on the Internet
-
- Here's the Individual Blue Shield Silver PPO It's a lot of material, so we won't just copy and paste, nor summarize it. It's mandated to be in plain English.
- Please note that Employer Group Plans may have MUCH better coverage than Individual, namely they may cover out of state Non Emergency, Non Urgent. Here's a Blue Cross Group EOC.
-
- Co Pays, Deductibles, OOP In vs Out of Network
- Appoint us as your Covered CA broker, no extra charge
- Get Instant California Health Quotes
- Get a Blue Shield Member Portal
Contact us – Get Quotes
All our Health plans are Guaranteed Issue with No Pre X Clause
Instant Quote & Subsidy #Calculation
There is No charge for our complementary services, we are paid by the Insurance Company.
- Our Quote Engine Takes all the complexity out of using pencil and paper to figure out the premiums per the Obamacare/ACA rules under CFR §1.36B-3 *
- We are authorized Brokers for Dental, Vision & Covered CA get instant quotes direct and in Covered CA with subsidy calculation for:
- Watch our 10 minute VIDEO that explains everything about getting a quote
Contact Us - Ask Questions - Get More Information - Schedule a Zoom Meeting
[email protected]
By submitting the information below , you are agreeing to be contacted by Steve Shorr a Licensed Sales Agent by email, texting or Zoom to discuss Medicare or other Insurance Plans as relevant to your inquiry. This is a solicitation for Insurance
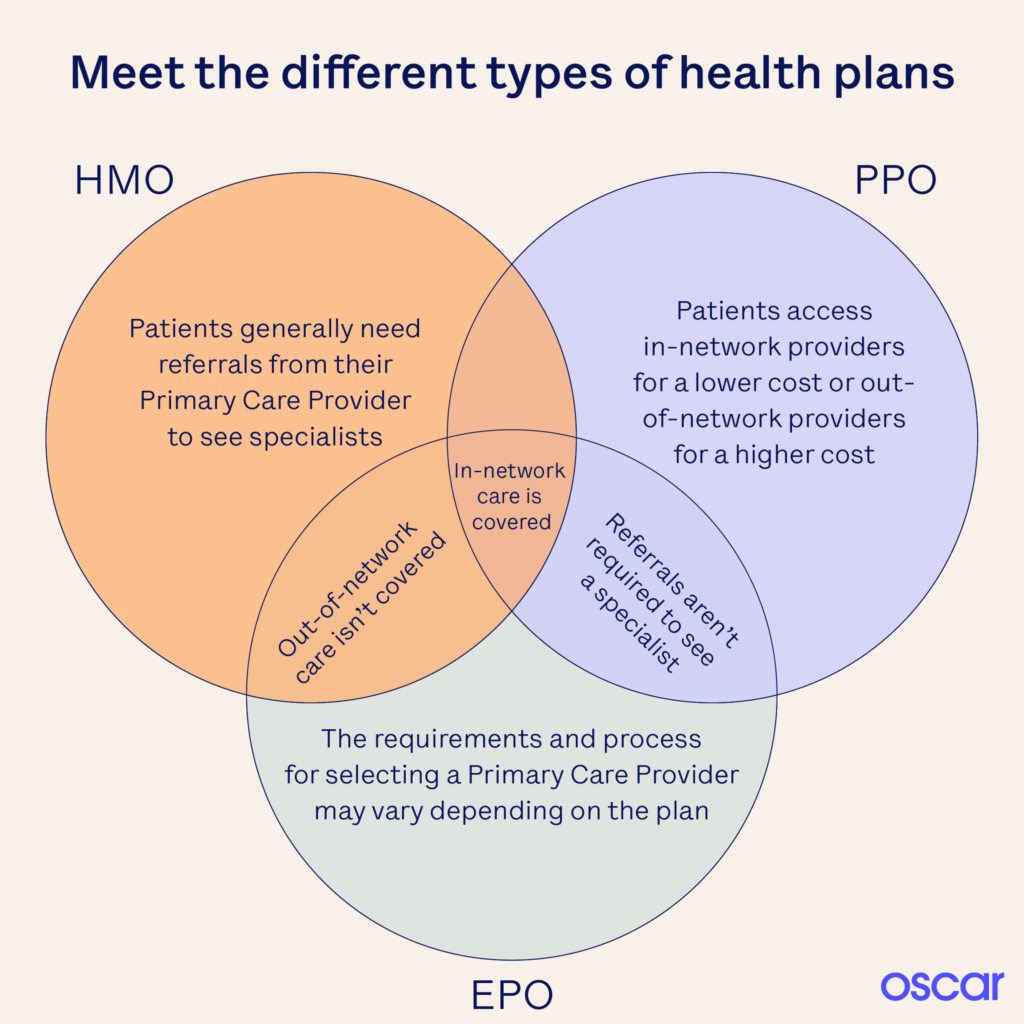
HMO - PPO - EPO
- Learn More - Oscar Explanation
- Provider Finder See also our Site Map for instructions & details on each companies provider finder
- ‘Father Of The HMO’ Dies At 95; Idea Didn’t Turn Out Like He Envisioned KFF
Medicare A & B if you don't #live in USA
Publication 11871
Medicare just visiting Out of County Publication # 11037
- medicare.gov/travel-outside-the-u.s.
- Our webpage on Medicare Coverage outside of USA
- FAQ - Buying Medi Gap if you live outside USA
- Get International Travel Quotes & Information
- Medi Gap - Covers up to $50k
- Medicare Advantage may cover unlimited ER and Urgent care - check the details
*********Social Security*****
Payments if you are living outside of USA # 10137
- Learn More
Our Webpages on:
Introduction
Since Medicare benefits are available only in the United States, it may not be to your advantage to pay the premium for Part B medical insurance if you will be out of the United States for a long period of time. But be aware that when you return and sign up for Part B, your premium will be 10% higher for each 12-month period you could have been enrolled in Part B, but were not.
If you return to the United States, you must re-enroll in Part B, but you may only do so from January through March each year, your benefits will not begin until July, and you may have to pay a premium penalty. CA Health Care Advocates HICAP
See also our page on Part B late enrollment penalty
So, how do I figure out the penalty vs paying the premium, which is better?
Try Medicare’s Calculator above
Bibliography
- Los Angeles Times 4.26.2015 Signing up late for Medicare Part B can trigger a lifelong penalty
- Enrolling for Part A & B #11036 Page 28 Living outside USA Part B…
All our Health plans are Guaranteed Issue with No Pre X Clause
Instant Quote & Subsidy #Calculation
There is No charge for our complementary services, we are paid by the Insurance Company.
- Our Quote Engine Takes all the complexity out of using pencil and paper to figure out the premiums per the Obamacare/ACA rules under CFR §1.36B-3 *
- We are authorized Brokers for Dental, Vision & Covered CA get instant quotes direct and in Covered CA with subsidy calculation for:
- Watch our 10 minute VIDEO that explains everything about getting a quote
#Covered CA Certified Agent
No extra charge for complementary assistance
- Get Instant Health, Dental & Vision Quotes, Subsidy Calculation & Enroll
- Appoint us as your broker
- Get Instant Health Quotes, Subsidy Calculation & Enroll
Related Pages - Travel Insurance








https://www.caloes.ca.gov/
https://www.fire.ca.gov/