California Based Health Insurance
Emergency and Urgent Care, ONLY? when Traveling?
Introduction
How does my California Coverage work out of Area?
- What coverage is there under a California issued Health Policy, when you are:
- Out of CA?
- Out of your HMO Service Area?
- Outside of USA?
- Learn more and enroll in International Travel Insurance.
- Questions of coverage can be quite confusing, especially what coverage might there be if your California issued coverage, is used out of your HMO local area, network, out of state or out of country.
- Coverage can differ if it’s for routine care, Urgent Care & Emergency or seeking out specialists at prestigious world famous clinics and hospitals.
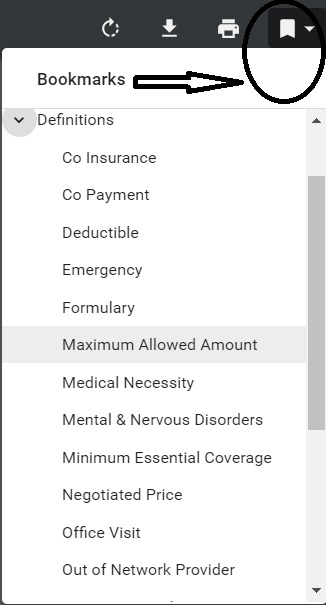
- For an example – check out the Blue Shield PPO Evidence of Coverage EOC
- Please refer to your specific Evidence of Coverage EOC for details of YOUR coverage.
- Coverage can differ if it’s for routine care, Urgent Care & Emergency or seeking out specialists at prestigious world famous clinics and hospitals.
- Note – Employer Group Plans appear MUCH more liberal!
#Insubuy Travel Health Insurance
Instant Quotes, Details and ONLINE Enrollment
Steve talks about International Travel Insurance VIDEO
US State Department - Travel - Insurance
Our webpage on Travel Insurance
Definition Urgent Care and #Emergency Services
Emergency Medical Condition
An illness, injury, symptom (including severe pain), or condition severe enough to risk serious danger to your health if you didn’t get medical attention right away. If you didn’t get immediate medical attention you could reasonably expect one of the following:
1) Your health would be put in serious danger; or
2) You would have serious problems with your bodily functions; or
3) You would have serious damage to any part or organ of your body. Health Net Glossary *
Urgent Care
Care for an illness, injury, or condition serious enough that a reasonable person would seek care right away, but not so severe as to require emergency room care.
How Much Does An Urgent Care Visit Cost In 2023? Forbes
Prior Authorization – Preauthorization
A decision by your health insurer or plan that a health care service, treatment plan, prescription drug or durable medical equipment (DME) is medically necessary. EOC * Our Webpage * Sometimes called prior authorization, prior approval or precertification. Your health insurance or plan may require preauthorization for certain services before you receive them, except in an emergency. Preauthorization isn’t a promise your health insurance or plan will cover the cost. Health Net Glossary *
Be sure to check the definition in YOUR EOC
Links related to Urgent & Emergency Care Definition
- Urgent Care vs ER
- Emergency Room – Obligation to treat uninsured patients
- Emergency Room – Balance Billing
- Health Net Provider Networks & Search
- Definitions – Glossary
- Providence Health – Difference between ER and Urgent Care
- Viewpoints: Insurance Companies Can Drop Patients Whenever; Choosing Between Doctor Vs. Urgent Care KFF
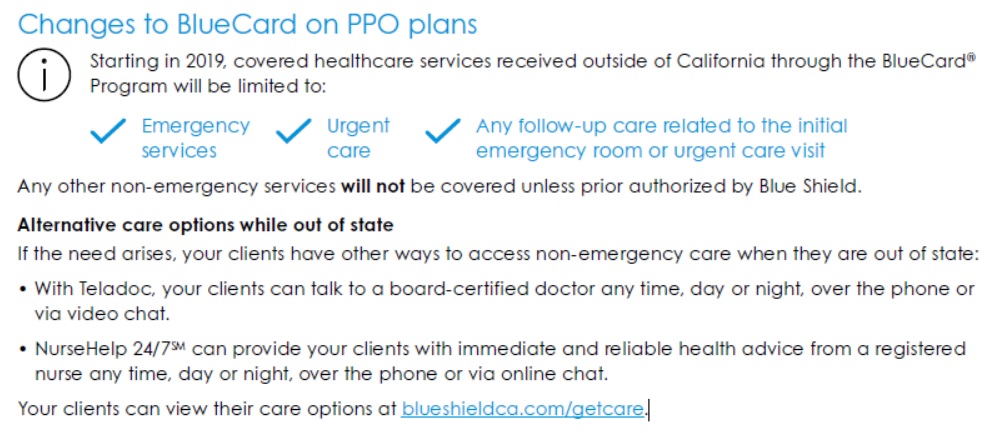
BlueCard Program
blue shield ca.com/provider/guidelines/blue card
& Inter plan Arrangements -
for members traveling out of state & outside of the united states
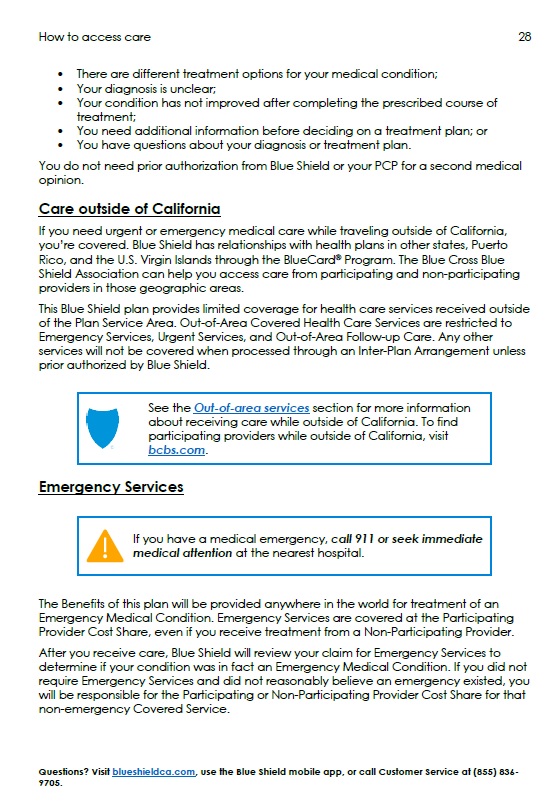
Excerpt from Typical EOC Evidence of Coverage
Out-of-area services
- Blue Shield has a variety of relationships with other Blue Cross and/or Blue Shield licensees. Generally, these relationships are called Inter-Plan Arrangements and they work based on rules and procedures issued by the Blue Cross Blue Shield Association. Whenever you receive health care services outside of California, the claims for those services may be processed through one of these Inter-Plan Arrangements described below.
- When you access health care services outside of the Plan Service Area, [see also Medicare.gov for a definition] you will receive the care from one of two kinds of providers.
- Most providers are participating providers and contract with the local Blue Cross and/or Blue Shield licensee in that other geographic area (Host Blue). S
- home providers are non-participating providers because they do not contract with the Host Blue. Blue Shield’s payment practices in both instances are described below and in the Introduction section of this Agreement.
This Blue Shield plan provides limited coverage for health care services received outside of the Plan Service Area. Out-of-Area Covered Health Care Services are restricted to
- Emergency Services,
- Urgent Services, and
- Out-of-Area Follow-up Care.
Any other services will not be covered when processed through an Inter-Plan Arrangement unless prior authorized by Blue Shield. Please see the Medical Management Programs section for additional information on prior authorization and the Emergency Benefits section for information on emergency admission notification.
- View YOUR actual EOC - It's YOUR EOC Policy that rules, not what you read on the Internet
- Here's the Individual Blue Shield Silver PPO It's a lot of material, so we won't just copy and paste, nor summarize it. It's mandated to be in plain English.

- Please note that Employer Group Plans may have MUCH better coverage than Individual, namely they may cover out of state Non Emergency, Non Urgent. Here's a Blue Cross Group EOC.
- Email from Blue Shield 2.7.2025 IFP Individual - Family Plans says that Blue Card went away with ACA.
- Co Pays, Deductibles, OOP In vs Out of Network
- Appoint us as your Covered CA broker, no extra charge
- Get Instant California Health Quotes
The BlueCard® Program links Blue plans across the United States and abroad through a single electronic network for claims processing and reimbursement. When an out-of-state Blue plan member seeks medical care from your office, use the information and tools in this section to submit those claims to Blue Shield of California. As a mission-driven, non-profit health plan, Blue Shield of California is working every day to create a sustainably affordable healthcare system that’s worthy of our family and friends.
- Find a doctor - but it seems you can only do that, if you currently have coverage. Finder requires you put in your Plan Prefix Code.
- BlueCard Program tools |
- Prior Authorization
Specimen Individual Policy #EOC with Definitions
Employer Group Sample Policy
It's often so much easier and simpler to just read your Evidence of Coverage EOC-policy, then look all over for the codes, laws, regulations etc! Plus, EOC's are mandated to be written in PLAIN ENGLISH!
- Find your own Individual EOC Evidence of Coverage
- It' important to use YOUR EOC not just stuff in general!
- Obligation to READ your EOC
- Plain Meaning Rule - Plain Writing Act
- Our Webpage on Evidence of Coverage
- OOP Out of Pocket Maximum - Many definitions are explained there.
VIDEO Steve Explains how to read EOC
CA Insurance Company Travel Guides
-
#World Wide Travel
- Kaiser – KP.org Travel Care away from home * 951-268-3900 *
- Provider Finder for all our companies
- Travel assistance services No matter where you are, help is with you Anthem Blue Cross
- Sharp
- sutter health plus.org/care-while-traveling
- US News & World Report 10.2015 – Coverage while outside USA
- Free Quotes, Brochures and complete information on travel coverage and International Medical Plans
- Medicare.Gov/Travel
- Brochures for people outside USA
- $50k Emergency Coverage in Supplemental & Advantage Plans - Check your EOC!
- Blue Shield Silver 70 PPO Off Exchange Evidence of Coverage EOC
- California Medi Cal rules on out of area coverage
-
Medical Info for American’s Traveling Abroad US State Department
-
Official Web Site for Canadian Health Care
-
Constitutional right to travel 14th Amendment
- Geo Blue Israel Bulletin October 9th. Google or see our travel site for latest information.
Why the restrictions in Coverage?
Going to Urgent Care vs ER Emergency Room
What if you’re out of the area, out of state?
Visiting an urgent care center can cost up to five times less than a visit to the ER and significantly reduce your wait time. While the average wait at a California ER is 4 hours and 34 minutes, urgent care center wait times are usually under an hour*. That means you can bypass the crowds and take your first step on the road to recovery.
- *”Urgent Care or the ER – Which is the Right Choice?” Health Alerts, Johns Hopkins Medicine, January 2011. Read more Accessing Urgent Care
- 49 Ways to stay out of the ER – Emergency Room Kevin MD.com
- The Insurance Company might base the claim payment on final diagnosis, rather than if a reasonable person felt their life was in danger?
-
Why CA Insurance Companies limited out of area – CA to urgent and emergency only
Too Many Claims
Blue Shield INDIVIDUAL Plans
Unauthorized Excerpt of Confidential Agent Guide
Blue Shield BlueCard Program frequently asked questions
Medicare A & B if you don't #live in USA
Publication 11871
Medicare just visiting Out of County Publication # 11037
- Medicare Abroad: Travel and Living Coverage Explained The Street.com
- medicare.gov/travel-outside-the-u.s.
- Our webpage on Medicare Coverage outside of USA
- FAQ - Buying Medi Gap if you live outside USA
- Get Travel Quotes & Information
*********Social Security*****
Payments if you are living outside of USA # 10137
- What if you work in two or more different Countries?
- International Social Security agreements, “Totalization agreements,” have two main purposes.
-
- First, they eliminate dual Social Security taxation, the situation that occurs when a worker from one country works in another country and is required to pay Social Security taxes to both countries on the same earnings.
- Second, the agreements help fill gaps in benefit protection for workers who have divided their careers between the United States and another country.
- Payments Abroad Screening Tool
- Learn More
Our Webpages on:
Introduction
Since Medicare benefits are available only in the United States, it may not be to your advantage to pay the premium for Part B medical insurance if you will be out of the United States for a long period of time. But be aware that when you return and sign up for Part B, your premium will be 10% higher for each 12-month period you could have been enrolled in Part B, but were not.
If you return to the United States, you must re-enroll in Part B, but you may only do so from January through March each year, your benefits will not begin until July, and you may have to pay a premium penalty. CA Health Care Advocates HICAP
See also our page on Part B late enrollment penalty
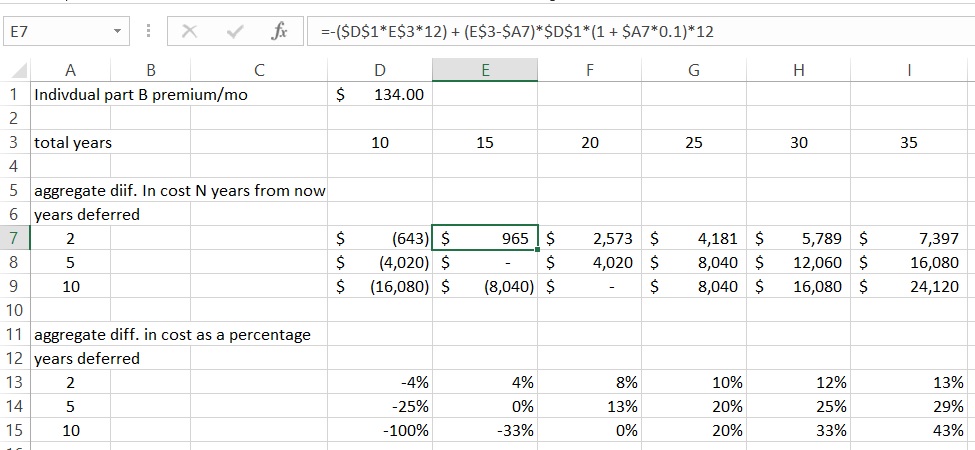
So, how do I figure out the penalty vs paying the premium, which is better?
Try Medicare’s Calculator above
Your Initial Enrollment Period ended September 30, 2009. You waited to sign up for Part B until the General Enrollment Period in March 2012. Your Part B premium penalty is 20%. (While you waited a total of 30 months to sign up, this included only 2 full 12-month periods.) You’ll have to pay this penalty for as long as you have Part B. Enrolling in Medicare # 11036 *
******************
Jeremy turned 65 in 2011. He did not sign up for Medicare Part B until 2017.
His penalty is:
10% x 6 years = 60 His penalty is thus 60% on top of the premium 0.6 X $134 (2017 Part B premium) = $80.40 penalty $80.40 + $134= $214.4 Jeremy will pay $214.4 on a monthly basis as his penalty Part B premium. United Medicare Advisors So, how does the penalty compare to if he had paid the $134 premium for 6 years?
10 years to even out
Here’s where a web site visitor did a spread sheet.
Spreadsheets are beyond my pay grade.
Bibliography
- Los Angeles Times 4.26.2015 Signing up late for Medicare Part B can trigger a lifelong penalty
- Enrolling for Part A & B #11036 Page 28 Living outside USA Part B…
FAQ’s
Just the answers
- I’m not aware of any way to put a temporary hold on Part B and Part D if one is out of country. You risk the Part B Late Enrollment Penalties and wouldn’t be able to get Part D Rx until the next AEP open enrollment period.
- If you are out of country more than say 6 months… or change residency, you may lose Part D and MAPD.
- If you enroll for Part A from abroad (Italy), and declined Part B, you became a candidate to receive an unsolicited phone call from a US government employee in Rome who handles SS/Medicare issues!! They want to make sure you understand the issues with respect to Part B penalties. I was told by a website visitor that the person was very helpful, but knew nothing about MediGap. He didn’t even know what it was.
- The late enrollment penalty takes the standard premium amount and increases it by 10% for each full 12-month period that you could have had Part B, but didn’t. For example, if you were first eligible for Part B in July 2015, but didn’t enroll until January 2018, you’d have a 20% late enrollment penalty. The standard premium amount would be increased by 20% for as long as you have Part B. Publication 11036 Enrolling in Part A & B * CA Health Advocates.org *
All our plans are Guaranteed Issue with No Pre X Clause
Quote & Subsidy #Calculation
There is No charge for our complementary services
Watch our 10 minute VIDEO
that explains everything about getting a quote
- Our Quote Engine Takes all the complexity out of using pencil and paper to figure out the premiums per the Obamacare/ACA rules under CFR §1.36B-3 *
- Get more detail on the Individual & Family Carriers available in CA
#Covered CA Certified Agent
No extra charge for complementary assistance
- Get Instant Health Quotes, Subsidy Calculation & Enroll
- Appoint us as your broker
- Get Instant Health Quotes, Subsidy Calculation & Enroll
- Videos on how great agents are
Related Pages - Travel Insurance












https://individuals.healthreformquotes.com/eligibility/#emergency
HOLY SMOKES – it worked (at least it looks promising)
Thank you Steve for your clever observation about BS of CA potentially being more liberal about considering out-of-state providers “in network” as of 2022 (even for Covered CA).
Actually I don’t know if this is really new or not – but I wouldn’t have pursued it unless you had sent me the new, updated, benefits guide (where you highlighted info specific to my out of state coverage situation in the 150 page document). This will save me AT LEAST 4 trips back and forth to CA, during a time when I need to be temporarily staying in another state to support a sick family member. YOU ROCK STEVE!!!
Your other customers might be able to benefit from this same thing if they log on to their BS of CA account and go to the section where they can FIND a DOCTOR (across the top of the page)
Scroll down to the VERY bottom of the page, on the left side it says ACCESSING CARE OUTSIDE CA. Two options under that including PROVIDERS OUTSIDE OF CA and COVERAGE OUTSIDE OF THE US. Click on that and it will take them to the “IN NETWORK” providers in the BLUE CARD Network!
FIND a DOCTOR ->ACCESSING CARE OUTSIDE OF CA-> PROVIDERS OUTSIDE OF CA
See attached letter where BS of CA explains it. Apparently the out of state provider (in Washington) will be considered in-network since the provider participates in the BlueCard program.
Feel free to put this on your site – as long as you take all the personal info off.
WELL DONE!!!

I’m traveling to Costa Rica next week.
Will Blue Shield PPO meet the Health Insurance Requirements to get a Visa?
Visitors traveling to Costa Rica will need to provide proof of a medical insurance policy to cover any COVID-19 related medical treatment or quarantine lodging while in Costa Rica.
In the case of international insurance, tourists must request from their insurer a certification issued in English or Spanish, noting:
1) the validity of the policy during the dates of visit to Costa Rica,
2) guarantee of coverage for medicals expenses in cases of COVID-19 related medical treatment in the amount of 50,000 USD and,
3) minimum coverage of 2,000 USD for extended lodging expenses due to COVID-19 related illness. US Embassy in Costa Rica
See webpage above, Blue Shield would be good for Requirement # 1
#2 Blue Shield would only page for urgent and emergency care
#3 I doubt Blue Shield would pay for lodging.
Don’t quote me! See the actual EOC Evidence of Coverage. See the bulletins on COVID coverage.
We are authorized brokers for Insuby where you can get a Costa Rican compliant policy!
We have a Silver PPO from Blue Shield of CA. (the primary coverage). Here’s the evidence of coverage.
It has hefty out of network deductibles, co pays and max out of pocket limits. For illustration purposes, let’s say the annual deductible for out of network is $25K and max out of pocket is $50K.
If we buy an annual travel plan with secondary medical coverage (they all seem to have secondary coverage – your webpage on dual coverage),
will the annual travel policy play pick up the hefty deductible ($25 k in this notional example) and $50K Max out of pocket, etc that Blue Shield of CA won’t pay if we end up hit by a bus in Italy and end up going to an out of network provider?
Please, let’s use the actual #’s and actually read and cite the real 1st hand information.
Are there any PPO Silver plans that don’t have the CALIFORNIA “in-network” requirement?
In other words, in the last year or two Blue Shield of CA has added a requirement that one needs to use a CALIFORNIA provider to have the encounter considered “in-network”.
Are there any Silver PPOs that allow one to go to providers (occasionally) in other states and have the encounters considered “in-network?
Basically, one needs to get their routine care done in CA. If it’s urgent or emergency, then you can go out of network out of state. See our “Blue Card” webpage.
2021 Rates and Benefits will be on our quote engine on the 15th http://www.quotit.net/eproIFP/webPages/infoEntry/InfoEntryZip.asp?license_no=0596610
IMHO it would be better to wait till November 1st to really look as then we will have information from all plans.
Then, you’ll want to check the summary of benefits and EOC Evidence of Coverage to verify the technical questions you are asking.
Here’s our page showing all the carrier pages, administrative and provider networks.
Here’s a master provider finder for all companies https://www.quotit.net/eproIFP/webpages/providers/providers_v20.asp?license_no=0596610
Plan Comparison PPO
Health Net
https://individuals.healthreformquotes.com/international/blue-shield-ppo-state-country/#emergency
Our webpage for finding Health Net Providers https://individuals.healthreformquotes.com/companies/health-net/portal/provider-networks-search/
At an agent meeting today, HN said their enhanced care PPO has over 10k doctors and medical groups like Facey & Scripps
Blue Shield PPO Providers Search https://individuals.healthreformquotes.com/companies/blue-shield/member-portal/provider-finder/
Blue Shield has 56K doctors and 325 hospitals in CA in Exclusive PPO Network https://www.blueshieldca.com/bsca/bsc/public/broker/PortalComponents/StreamDocumentServlet?fileName=A49537-OL_1-21.pdf
Please note, it’s confusing keeping track of all these names. Health Care Reform didn’t really allows us to keep our doctor.
Our webpage on narrow networks
Blue Cross of CA
Out-of-state protection: benefits that travel with you
When you are out of California for work, school or on vacation, you should not have to worry about health surprises. Through the BlueCard® program, https://www.blueshieldca.com/bluecard our exclusive provider organization (EPO) plans cover nonemergency, emergency and urgent care, while our health maintenance organization (HMO) plans cover medically necessary emergency and urgent care visits. The program applies to all 50 states.
Exclusive provider organization (EPO):
With our EPO plans, you will be able to see any in network doctor. It is a good idea to have a primary care doctor to coordinate your care, so we will pick one close to your home and let you know your assignment in the beginning of the year. You do not need to see this doctor for services or referrals, and you can change your assigned primary care doctor at any time. EPO plans do not offer out of network benefits, except for emergency and urgent care, ambulance services or when a service is preapproved. If you see a doctor not in your plan for any other reason, you will have to pay 100% out of pocket.
EPO plans are available in
Alpine, Amador, Butte, Calaveras, Colusa, Del Norte, Glenn, Humboldt, Imperial, Inyo, Kern, Lake, Lassen, Mariposa, Mendocino, Merced, Modoc, Mono, Monterey, Nevada, Plumas, San Benito, San Joaquin, San Luis Obispo, Santa Barbara, Santa Clara, Santa Cruz, Shasta, Sierra, Siskiyou, Stanislaus, Sutter, Tehama, Trinity, Tulare, Tuolumne, Ventura and Yuba counties
BlueCard® Program and Blue Shield Global Core
Covered services and urgent and emergency care while traveling in the United States or abroad.
HMO and EPO plan members: Coverage for emergency and urgent care services.
PPO, POS, and Active Choice® members: Same as above plus access to covered benefits (except dental, vision care, and prescription drugs).
If in the United States: Call (800) 810-BLUE or visit provider.bcbs.com.
If overseas: Call (804) 673-1177 or visit bcbsglobalcore.com.
This sounds good, BUT the benefits provided are in your EOC Evidence of Coverage, the actual contract that you have with the insurance company.
Blue Card is simply stating that if your EOC says so, then you can have these benefits. There might be a difference between Individual and Employer Group plans on this benefit.
So, now this question is getting beyond my pay grade as it’s my recollection that the contract – agreement has priority and not some ancillary benefit on some other page, that doesn’t really apply to the actual policy that an Individual can purchase in CA.
See our webpage on how to read and interpret a contract.
Coverage out of the state of California due to COVID travel restrictions???
I have Blue Shield of CA, Silver PPO, on-exchange (Covered California).
I am presently in WASHINGTON state caring for a very sick family member and will be in WASHINGTON for another 90 +/- days. I had planned to go back to CA, (to my normal providers) for a few days, to have some tests and procedures done for continuing care conditions (Breast Cancer follow up concerns, migraine management) among other things. {NOTE: these procedures and tests have already been been “pre-authorized by BS of CA}
Given the COVID travel restrictions / stay at home / quarantine orders in both states I am not able to make it to my home providers in California to have these tests/procedures. Some things I can postpone (like my annual dermatology check – other things I can not postpone (like a recently ordered breast Ultrasound and mammogram, etc).
QUESTION:
Can I go to providers in WASHINGTON state that accept Blue Shield, for those things I can’t postpone AND have them considered “in-network” – OR – will going to a WASHINGTON State Blue Shield provider be considered out-of-network on my “on-exchange” CALIFORNIA Silver PPO?
If I can go to WASHINGTON state provider (in the Blue Shield Network) to have these continuing care tests / procedures, what is the process for doing so?
How do I document or get approvals or whatever, so that it is considered “in network” and I don’t have to pay out of network rates or completely out of pocket?
I need to get these procedures re-scheduled in WASHINGTON in the next couple weeks.
Thank you!
IMHO the first place to go, would be the Blue Shield member portal and ask them to accommodate you. https://individuals.healthreformquotes.com/companies/blue-shield/member-portal/
Here’s an example of Blue Shield accommodating people with a similar situation
Blue Cross and Blue Shield of Oklahoma will authorize any member who was receiving treatment outside of Oklahoma prior to March 15 to continue receiving care closer to home if they prefer not to travel during the COVID-19 crisis through July 31. This date is an extension from the original end date of June 30. Members can transition to an in-network provider in Oklahoma or BCBSOK will cover the costs to see an out-of-network provider in Oklahoma at the in-network rate. AHIP.org
Public Health Emergency?
The purpose of the 1135 waiver authority is to ensure that sufficient healthcare services are available to meet the needs of individuals enrolled in SSA programs when and where an emergency is experienced.
the secretary can waive or modify specific requirements to match the particular needs of the emergency event and service providers. Section 1135 allows the secretary to waive or modify the following reimbursement requirements:
Out-of-Network Payments—Limitations on payments to permit …enrollees to use out-of-network providers in an emergency situation.
Social Security Act, Section 1135 Waiver Authority in National Emergencies
Forcing you to use out of network providers might be considered to be AGAINST PUBLIC POLICY!
https://www.upcounsel.com/what-contracts-are-considered-to-be-contrary-to-public-policy
duhaime.org/LegalDictionary/P/PublicPolicy.aspx
See our webpage on how Insurance Companies are covering COVID
Thanks for your answers. Is it fair to say that, in 2019, both PPO options, available in my zip code (San Diego County), Blue Shield of California and Health Net, classify (hence reinburse) non emergency treatment OUTSIDE of CALIFORNIA as out of network / non preferred providers.
It’s my understanding they won’t pay at all. See comment below.
Please read the excerpt 3 times, then when you think you understand it, read it again. Justice Frankfurter. If you disagree, then you should probably talk to someone who actually completed law school, passed the bar and specializes in Insurance Contracts. My bio is here.
In 2019, Are there any PPOs in California, that provide services considered in network, our of state or out of the country. Blue shield used to but apparently will stop in 2019
First try our quote engine and see.
Here’s a sample proposal. Please note that this is for San Pedro, CA. Different plans are offered in different counties, zip codes. 19 rating areas in CA.
Health Net Enhanced Care PPO is the only other one.
HN Covered CA information
Evidence of Coverage Silver 87 Enhanced Care PPO
Page 7 :
THIS BENEFIT PLAN PROVIDES BOTH PREFERRED PROVIDER AND OUT-OF-NETWORK PROVIDER BENEFITS FOR SERVICES (INCLUDING BEHAVIORAL HEALTH TREATMENT) ONLY WITHIN CALIFORNIA.
THIS BENEFIT PLAN DOES NOT PROVIDE BENEFITS FOR SERVICES (INCLUDING SERVICES FOR BEHAVIORAL HEALTH TREATMENT) OUTSIDE OF CALIFORNIA, EXCEPT FOR URGENT CARE AND EMERGENCY CARE.
OUTSIDE THE UNITED STATES, COVERAGE IS LIMITED TO URGENT CARE AND EMERGENCY CARE, AS DESCRIBED BELOW UNDER “FOREIGN TRAVEL OR WORK ASSIGNMENT” IN THIS “MISCELLANEOUS PROVISIONS” SECTION.
If Blue Shield of California PPO plans ( either on or off the exchange ) no longer cover non – emergency coverage – then are they any better than an HMO?
What am I paying the extra for???