Mental Health as an essential benefit under ACA Health Care Reform
Parity Laws – Mental Health must be equal to Medical Benefits
Try turning your phone sideways to see the graphs & pdf's?
Mental Health
- Mental is an essential mandated benefit under ACA/ObamaCare/Health Care Reform
- All Insurance plans – QHP qualified health plan (Obama Care compliant-meeting the 10 essential benefits) must provide parity equal coverage for mental health and substance use services as for other conditions, illness and accident resulting in no added treatment limits and no extra costs, co pays, deductibles..
- More than 43 million Americans suffer from depression, anxiety, and other mental health conditions. But more than half the people who felt like they needed help last year, never got it. Even people who had insurance complained of barriers to care, like Narrow Provider Lists? Some said they still couldn’t afford it; some were embarrassed to ask for help. Others just couldn’t get through the red tape.
- Hopefully, the ACA mandate and parity laws will help remedy the problem.
Information, links and resources
- Mental Health Parity Act 1996 Wikipedia
- Parity – Using Employer Sponsored Plan SAMHSA 8 page pdf
- I’m not sick & don’t need help – Book
- Dealing with social & mental problems can cut health care costs CA Health Line 1.23.2017
- NAMI (National Assoc of Mental Illness) Website, Insurance & Health Care Reform Section
- FAQ on if Mental Health Therapist Benefits vary by Metal Level
- Our Webpages on:
- Affordable Care Act Will Expand Mental Health and Substance Use Disorder Benefits and Parity Protections for 62 Million Americans, that details how EHBs will expand mental health and substance use disorder benefits and federal laws requiring that mental health benefits be equal to, or have “parity” with, other health benefits in the individual and small group markets. .bna.com/hhs-releases-essential-n17179872551/
- kff.org/the-implications-of-covid-19-for-mental-health-and-substance-use
- Medi Cal & Behavioral Health Services
- health payer intelligence.com private-insurance-covers-most-nonelderly-adults-with-mental-health-needs
- Union accuses Kaiser of violations months after state fine on mental health care April 2024
Call 988 for Mental Health Emergencies
Mid July 2022 there is supposed to be a new # to call, just like 911 for Mental Health Emergencies, but the funding doesn't see to be there for California.
#Medicare & You - Mental Health

- Medicare & Mental Illness Publication # 10184
- Find therapists who accept Medicare Assignment
- Medicare Billing Etc Guidelines for Professionals
- Our Webpage on Medicare & Mental Health
- Mental Health
- Medicare.Gov on Mental Health
- EOC Evidence of Coverage - Plain English,
- Los Angeles Consumer Resources #Directory
- Los Angeles Times on low cost & free therapy alternatives
- NPR Mental Health & COVID
- Guide to Mental Health Benefits (The Mighty)
 Compliance Assistance Guide from DOL.Gov Health Benefits under Federal Law
Compliance Assistance Guide from DOL.Gov Health Benefits under Federal Law
- Mental Health Videos
- Veteran's Mental Health
- CMS Learning Aid for Mental Health Professionals
Get a term life quote here,
to protect your loved one
AB 88 California Mental Health Parity
Federal Mental Health Parity
#California Mental Health Insurance Parity
Summary:
- Senate Bill 855 – Mental Health as a Medical Necessity
- Our webpage on Medical Necessity
- Insurers Begin To Tackle Complex Mental Health Compliance Rules kff September 2024
- AB 88 CA Insurance Code §§10144.5. Health and Safety Code§1374.72 requrires that severe mental illness for children be covered and also prohibits health plans from basing medical necessity denials on whether the admission for mental health services was voluntary or involuntary, WIC 5150 hold CA Legislator * or on the method of transportation of the patient to the health facility.
- AB 88 also requires Insurance Companies that offer mental health services (Individual & Families * Medi-Cal * Employer Groups) to have information on their website that will assist enrollees in accessing mental health services. SB 1553 §1368.015, §1367.015Health & Safety Code Blue Cross / Anthem Mental Health Procedures
SB 221 Return Visit Guarantees
SB 221 requires that Mental health and substance abuse patients be offered return appointments no more than 10 days after a previous session, unless their provider OKs less frequent visits. CA HealthLine * CA Health Line 11.24.2021 *
Severe Mental Illness Coverage
AB 88 – Insurance Code §10144.5
(a) Every policy of disability (health) insurance that covers hospital, medical, or surgical expenses in this state* … shall provide coverage for the diagnosis and medically necessary treatment of severe mental illnesses of a person of any age, and of serious emotional disturbances of a child, … under the same terms and conditions applied to other medical conditions,
(b) These benefits shall include the following:
(2) Inpatient hospital services.
(3) Partial hospital services.
(4) Prescription drugs, if the policy or contract includes coverage for prescription drugs.
How to obtain, get or find these benefits?
(c) The terms and conditions applied to the benefits required by this section that shall be applied equally to all benefits under the disability (Health, Medical) insurance policy shall include, but not be limited to, the following:
(1) Maximum lifetime benefits.
(2) Co-payments and coinsurance.
(3) Individual and family deductibles.
(d) For the purposes of this section, “severe mental illnesses” shall include [these diagnosis]:
(1) schizophrenia.com/ *
(2) Schizoaffective disorder. *** WedMD
(3) Bipolar disorder (manic-depressive illness). bipolar.com/*** WebMD
(4) Major depressive disorders. *** WebMD
(5) Panic disorder. *** WebMD
(6) Obsessive-compulsive disorder.*** WebMD
(7) Pervasive developmental disorder WebMD or autism. *** Web MD
(8) Anorexia nervosa. *** WebMD
(9) Bulimia nervosa. *** WebMD
(e) For the purposes of this section, a child suffering from, “serious emotional disturbances of a child” shall be defined as a child who
(1) has one or more mental disorders as identified in the most recent edition of the Diagnostic and Statistical Manual of Mental Disorders, other than a primary substance use disorder or developmental disorder, that result in behavior inappropriate to the child’s age according to expected developmental norms, and …
California Law Aims to Strengthen Access to Mental Health Services
FEDERAL – Mental Health Parity and Addiction Equity Act of 2008
- The 2008 Mental Health Parity and Addiction Equity Act already requires insurers and corporate-backed health plans to provide access and payment structures for mental health care services on par with other medical services.
- In practice, that is often not the case, with less than half of U.S. adults with mental illness able to access care in 2020, while nearly 70% of children cannot receive treatment, according to studies cited by the administration.
- Under the new rules, federal officials are clarifying that autism, intellectual and neurodevelopmental disorders and all other conditions listed in the mental, behavioral and neurodevelopmental disorders chapter of the current International Classification of Diseases or the Diagnostic and Statistical Manual of Mental Disorders must be included under the definition of “mental health benefits” for plans and coverage.
- Biden admin to require mental health coverage parity – The White House says health insurers are not complying with 2008 law in a move that’s likely to draw legal challenges from the industry Politico September 22024
- Our webpage on Autism
- Final Rule to strengthen Parity Law 9/9/2024 Reuters
- Fact Sheet: Final Rules under the Mental Health Parity and Addiction Equity Act (MHPAEA)
- Fact Sheets & FAQs On Mental Health Parity 2008
- Regulations & Guidance
- Wikipedia
- Code of Federal Regulations §146.136 Parity in mental health and substance use disorder benefits.
Mental Health Bill of Rights
The Mental Health Parity Act of 1996 (MHPA)
- MHPA is a federal law that may prevent your group health plan from placing annual or lifetime dollar limits on mental health benefits that are lower – less favorable – than annual or lifetime dollar limits for medical and surgical benefits offered under the plan. Learn more on Wikipedia Mental Health Parity Act 1996
- The act removes separate treatment limitations for mental health and chemical dependency benefits (including number of visits, days of coverage, and annual dollar limits) and requires cost sharing for these services to be equal to or less than the cost sharing for other health care services. (Federal Mental Health Parity Act of 2007 NAMI More on Mental Health Parity NAMI) Public Law 110–343 wikipedia.org/110-343
- MHPA applies to most group health plans with more than 50 workers. MHPA does NOT apply to group health plans sponsored by employers with fewer than 51 workers. MHPA also does NOT apply to health insurance coverage in the individual market.
- MHPA is a federal law that requires that annual or lifetime dollar limits on mental health benefits provided by a group health plan be no lower than the annual or lifetime dollar limits for medical and surgical benefits offered by that plan. MHPA applies to employers with more than 50 employees. For up to date information on the applicability of the Mental Health Parity Act, contact the EBSA regional office nearest you.
- Statute1185 A
- Regulations
- Fact Sheet
- Publications
The MHPA does not prohibit group health plans from:
Covering mental health services within network only, even though the plan will pay for out of network services for
- medical/surgical benefits (although with higher out-of-pocket cost to the subscriber);
- Increasing co-payments or limiting the number of visits for mental health benefits;
- Imposing limits on the number of covered visits, even if the plan does not impose similar visit limits for medical and surgical benefits; and
- Having different cost-sharing arrangements, such as higher coinsurance payments for mental health benefits, as compared to medical and surgical benefits
- HOWEVER, check out the rules under ACA/Obamacare & AB 88
- .A visit limit coupled with a usual, customary, and reasonable (UCR) charge is not the equivalent of an annual or lifetime dollar limit. As a result, it is not a violation of the MHPA requirements. Payments made by the plan on the basis of UCR charges will vary from one case to the next.
- What is not permitted is a limit on the number of visits, together with a fixed dollar limit per visit, for example, 60 visits annually at $50 per visit (totaling $3,000), unless the medical-surgical coverage is the same.cms.hhs.gov
Resources & Links
- wikipedia.org/Mental_health_parity
- Our webpage on how to read a contact and Insurance Policy
- Technical Resources
- IRS Code § 9812. Parity in the application of certain limits to mental health benefits
- Federal MHPA Renewal Legislation S.558
- Library of Congress
- 42 USC 18022 (E) Mental health and substance use disorder services, including behavioral health treatment.
- Essential Health Benefits
- §146.136 Parity in mental health and substance use disorder benefits.
- NAMI South Bay Website
All our plans are Guaranteed Issue with No Pre X Clause
Quote & Subsidy #Calculation
There is No charge for our complementary services
Watch our 10 minute VIDEO
that explains everything about getting a quote
- Our Quote Engine Takes all the complexity out of using pencil and paper to figure out the premiums per the Obamacare/ACA rules under CFR §1.36B-3 *
- Get more detail on the Individual & Family Carriers available in CA
Substance Abuse Treatment
SB 855 2020
#Substance Abuse Treatment
SB 855 requires insurance companies to expand the definition of Mental Health to include Substance abuse and cover as any other illness. Learn More — Bill Summary
(2) “mental health and substance use disorders” means a mental health condition or substance use disorder that falls under any of the diagnostic categories listed … Diagnostic and Statistical Manual of Mental Disorders.
(g) This section shall not apply to accident-only, specified disease, hospital indemnity, Medicare supplement, dental-only, or vision-only insurance policies. Autism 7.1.2012 SB 946 §10144.5.
Plans must cover out-of-network services based on billed charges (rather than a discounted allowed amount or negotiated price) immediately if the plan was not able to provide in-network services in a timely manner based geographic access and timeliness requirements. CA Health Line *
Links & Resources
- Using Health Insurance to Attend Drug Treatment in California
- Blue Shield Summary & FAQ’s *
- CA Insurance Commissioner letter to All Health Insurance Companies to comply with SB 855 to provide coverage for medically necessary treatment of mental health and substance use disorders, as defined, under the same terms and conditions applied to other medical conditions.
- magellan provider focus.com/what-you-need-to-know-about-senate-bill-855
- Analysis of California Senate Bill 855 Health Coverage: Mental Health or Substance Abuse Disorders 104 pages report to State Legislature
- aacap.org/Medical_Necessity_Criteria
- Treatment Guidelines: Substance Use Disorders
- PRACTICE GUIDELINE FOR THE Treatment of Patients With Substance Use Disorders Psychiatry Online . org 276 pages
- Magellan’s Adopted Clinical Practice Guidelines For the Assessment and Treatment of Patients With Substance Use Disorders
- Fact Sheet SB 855 5 pages Senator Scott Wiener
- Treatment Guidelines: Substance Use Disorders
- medicare.gov/ mental-health-substance-use-disorder-services
- medicare advocacy.org/coverage-of-mental-health-services/
- Medicare Coverage of Substance Abuse Services MLN
FAQ’s
Substance Abuse Treatment
- Question My son lives in California and has medi – cal age 28 yrs. He has dual diagnosis mental health and substance use, it’s almost impossible to get him into a residential rehab because most places don’t take medi cal.
- Is there any affordable extra insurance we can get for him in this particular area.
.
- Is there any affordable extra insurance we can get for him in this particular area.
- Answer
- You could pay full price – no subsidies as they are not available if you qualify for Medi Cal for an Individual Plan.
- See information below on Medi Cal coverage and how to appeal.
- What Medi Cal Insurance Company HMO is he in?
- Did you check with them?
- medicaid.gov/substance-use-disorders
- LA Public Health Substance Abuse
- Here’s what I found in Google on Treatment Centers that take Medi Cal.
- FAQs / Ask Us a Question
. - Ok so my homeless friend has Medi Cal. Let’s say we got him a blue shield ppo in addition. I realize that it will be expensive but my question is how will it work.
-
1. Let’s say he went to a $50,000 inpatient place and insurance covered 10%. So we would be responsible for the remaining amount or only up to a certain amount?
-
2. What if he goes to the hospital would Medi-cal cover his stay or no because he has other health care.
-
3. We would really like to help him out but I get different answers from different people. I apologize if you already answered. I will read through when I get time.
.
-
- Get quotes for Blue Shield PPO
- # 1 your question sounds good, but doesn’t make sense. How would the Insurance only pay 10%? Are you talking about the Blue Shield PPO or Medi Cal?
- Private Insurance pays first. Then if you are using a Medi Cal provider, Medi Cal would pay.
- Our webpage on Medi Cal & Dual Coverage
- # 2 See above.
- # 3, that’s why I only give answers with a citation and don’t take phone calls.
- Private Insurance pays first. Then if you are using a Medi Cal provider, Medi Cal would pay.
Maximum #a190 Medicare Psychiatric Inpatient Days?
- If one is mentally #ill, has Medicare and Medi Cal, is constantly in and out of inpatient care, will Medi Cal pay if Medicare doesn’t as the person maxed out his inpatient days and used up the lifetime limit?
-
- Yes, Medicare pays or doesn’t pay and then Medi Cal is the secondary payer. § 1300.67.13. Coordination of Benefits (“COB”).
- References & Links
- Our webpages on:
- What is covered under Medicare Parts A & B
- Appeals & Grievances
- Dual Coverage
- Which Pays first Medi Cal or other coverage?
- Medicare
- Medicare #DualCoverage
# 02179
- most health care costs are covered if you qualify for both Medicare and Medicaid. Medicaid never pays first for services Medicare covers. It only pays after Medicare has paid Page 11
- Choose Medi Cal HMO
- Medicare #DualCoverage
- SSI, SSDI & Automatic Medicare Coverage
Medicare Benefit Period – CA Health Care Advocates
Medicare & You Publication 10050 Page # 121
Benefit period
The way that Original Medicare measures your use of hospital and skilled nursing facility services. A benefit period begins the day you’re admitted as an inpatient in a hospital or skilled nursing facility. The benefit period ends when you haven’t gotten any inpatient hospital care (or skilled care in a skilled nursing facility) for 60 days in a row. If you go into a hospital or a skilled nursing facility after one benefit period has ended, a new benefit period begins. You must pay the inpatient hospital deductible for each benefit period. There’s no limit to the number of benefit periods.
Mental health care (inpatient) Medicare.Gov Medicare & You page 27
However, if you’re in a psychiatric hospital (instead of a general hospital), Part A only pays for up to 190 days of inpatient psychiatric hospital services during your lifetime.
- Try Medi Cal for additional days
-
-
LA Care EOC Evidence of Coverage and Member Handbook
Coordination of Benefits (COB): The process of determining which insurance coverage (Medi-Cal, Medicare, commercial insurance or other) has primary treatment and payment responsibilities for members with more than one type of health insurance coverage.
The LA Care EOC page 49 states:
Other Medi-Cal programs and services
Other services you can get through Fee-For-Service (FFS) Medi-Cal or other Medi-Cal programs
Sometimes L.A. Care does not cover services, but you can still get them through FFS Medi-Cal or other Medi-Cal programs. This section lists these services. To learn more, call L.A. Care Member Services at 1-888-839-9909 (TTY/TDD 711).
- Medi Cal coverage – County Mental Health
-
Specialty mental health services
Some mental health services are provided by county mental health plans instead of L.A. Care. These include specialty mental health services (SMHS) for Medi-Cal members who meet medical necessity rules. SMHS may include these outpatient, residential and inpatient services:
• Inpatient services:
° Acute psychiatric inpatient hospital services
° Psychiatric inpatient hospital professional services
° Psychiatric health facility servicesTo learn more about specialty mental health services the county mental health plan provides, you can call your county mental health plan.
-
To find all counties’ toll-free telephone numbers online, visit dhcs.ca.govMHPContact List
-
-
- Medi-Cal Specialty Mental Health Services
- Medi Cal and Social Service Contacts for Assistance
- dmh.lacounty.gov
- Evidence of Coverage D SNP – Page 77
- CBO.gov THE INPATIENT PSYCHIATRIC HOSPITAL BENEFIT UNDER MEDICARE July 1993
- Medi Cal Inpatient Mental Health Services Program
- chcf.org/Medi Cal Explained Behavioral Health.pdf
- ‘Go on Medi-Cal to get that’: Why Californians with mental illness are dropping private insurance to get taxpayer-funded treatment
- Advocates Guide to Medi Cal – Mental Health
- Cal. Code Regs. Tit. 9, § 1820.205 – Medical Necessity Criteria for Reimbursement of Psychiatric Inpatient Hospital Services
- MHSUDS INFORMATION NOTICE NO.: 19-026
-
-
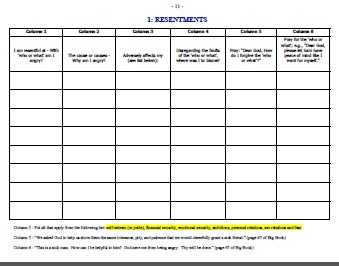
AA’s 12 STEPS, INCLUDING #POWERFUL 4 TH STEP WORKSHEETS
Herb K's workbook

#My Medi-Cal
How to get the Health Care
You Need
24 pages
Smart Phones - try turning sideways to view pdf better
-
- More explanation

- Enroll with Benefits Cal
- What is Medi Cal - VIDEO
-
How to VIDEO
-
Medi-Cal Managed Care HMO – Health Care Options
- Benefits Cal is a one-stop-shop to apply for...
- Cal Fresh
- Ages 26 through 49 Adult Full Scope Medi-Cal Expansion regardless of immigration status
- Cal WORKs
- Medi-Cal
- CMSP (County Medical Services Program)
- Disaster Cal Fresh
- GA/GR (General Assistance and General Relief )
- Briefing — Medi-Cal Explained: An Overview of Program Basics
- chcf.org/medi-cal-explained/
- #BenefitsCal is a one-stop-shop to apply for...
- Medi-Cal
- County Medical Services Program (CMSP),
- Food Assistance - Cal Fresh (formerly known as Food Stamps)
- How to use Eat Fresh.org VIDEO
- Cooking & Nutrition
- California Work Opportunity and Responsibility to Kids (CalWORKs) or check their other website
- Medi-Cal
-
Here you can review and choose the HMO that you want to deliver your Medi-Cal health Care.
-
BIC Benefits Identification Card
Mental Health - Related Pages
- Mental Health – ACA/Health Reform Mandated Essential Benefit
- Autism – Essential Benefits & Health Coverage
- Resources – Mental Health – Conservatorship – FSP
- Therapist find one who takes Medicare – ACA – Blue Shield
- Medicare & Mental Health
- Find Resources – Aunt Bertha
- FSP Full Service Partnership
- Laura’s Law
- Lanterman LPS Conservatorships
- §1370 Murphy Conservatorship
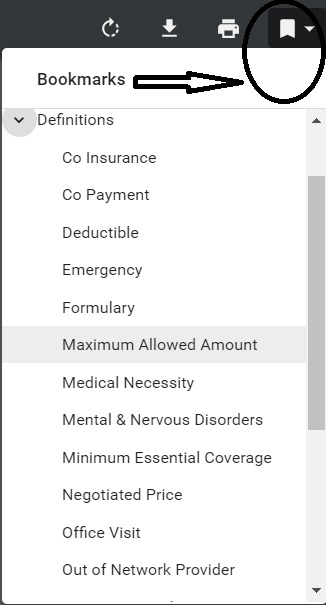
Specimen Individual Policy #EOC with Definitions
Employer Group Sample Policy
It's often so much easier and simpler to just read your Evidence of Coverage EOC-policy, then look all over for the codes, laws, regulations etc! Plus, EOC's are mandated to be written in PLAIN ENGLISH!
- Find your own Individual EOC Evidence of Coverage
- It' important to use YOUR EOC not just stuff in general!
- Obligation to READ your EOC
- Plain Meaning Rule - Plain Writing Act
- Our Webpage on Evidence of Coverage
- OOP Out of Pocket Maximum - Many definitions are explained there.









https://business.kaiserpermanente.org/california/care-value/mental-health-services
https://www.dol.gov/agencies/ebsa/about-ebsa/our-activities/resource-center/publications/understanding-your-mental-health-and-substance-use-disorder-benefits
https://www.dol.gov/sites/dolgov/files/EBSA/laws-and-regulations/laws/mental-health-parity/mental-health-substance-use-benefits-parity.pdf
https://adaa.org/
https://blueshieldca.crediblemind.com/
If one is mentally ill, has Medicare and Medi Cal, is constantly in and out of inpatient care, will Medi Cal pay if Medicare doesn’t as the person maxed out his inpatient days and used up the lifetime limit?
We are answering your question in the webpage above.