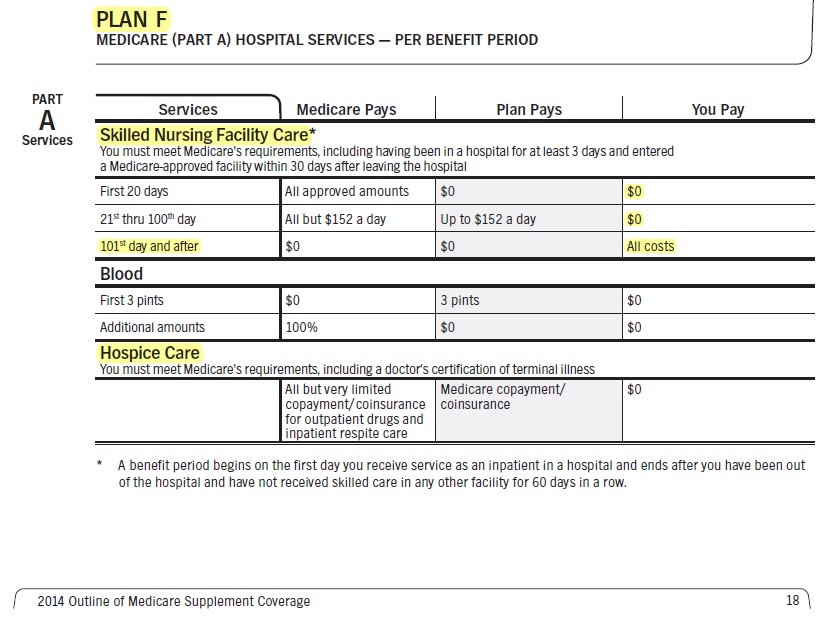
Skilled nursing facility care
Medicare covers semi-private rooms, meals, skilled nursing and rehabilitative services, and other medically necessary services
(Clinical Guidelines – Oscar – Explains Medical Necessity Requirements so much better and in logical order!)
and supplies furnished in a skilled nursing facility after a 3-day minimum, medically necessary, inpatient hospital stay Medicare Policy Manual * Publication 10153 SNF * for a related illness or injury. An inpatient hospital stay begins the day the hospital formally admits you as an inpatient based on a doctor’s order and doesn’t include the day you’re discharged. You may get coverage of skilled nursing care or skilled therapy care if it’s necessary to help improve or maintain your current condition.
A SNF is a care center where nurses and nursing assistants are available to provide twenty-four hour care for patients to assist them with conditions in their transition between the hospital and a lower level of care such as the home. A SNF may also provide rehabilitation in order to improve the member’s function and decrease the burden of care. Oscar Clinical Bulletin *
To qualify for skilled nursing facility care coverage, your doctor must certify that you need daily skilled care (like intravenous injections or physical therapy) which, as a practical matter, can only be provided in a skilled nursing facility if you’re an inpatient.
You pay:
- Nothing for the first 20 days of each benefit period
- $185 Coinsurance per day for days 21–100 of each benefit period
- Sample Medicare Advantage Copay
- Medicare Advantage must pay at least as well and same qualifications as Original Medicare.
- MAPD can’t do “funny stuff” or they can get busted for Risk Adjustment Fraud
- Sample Medi Gap
- All costs for each day after day 100 in a benefit period Medicare.Gov SNF *
Medicare doesn’t cover long-term care or custodial care.
Medical Requirements
The beneficiary needs daily skilled care or rehabilitation services as ordered by a physician. These skilled services can only be rendered by, or under the direct supervision of, skilled nursing or rehabilitation staff. In addition, the skilled services the patient receives must be for a medical condition they were treated for during the three-day qualifying hospital stay, or for a condition that arose during that hospital stay or while the patient was receiving Medicare-covered SNF care.
The requirement of “daily” skilled services should not be taken so literally that occasional sessions missed due to holidays or illness will make the patient not meet the daily requirement for skilled services.
See Oscar’s Clinical Guidelines – It’s explained so much better!
Daily Skilled Services Defined
Skilled nursing services or skilled rehabilitation services (or a combination of these services) must be needed and provided on a “daily basis,” i.e., on essentially a 7-days-a week basis. A patient whose inpatient stay is based solely on the need for skilled rehabilitation services would meet the “daily basis” requirement when they need and receive those services on at least 5 days a week. (If therapy services are provided less than 5 days a week, the “daily” requirement would not be met.) Medicare Benefits Policy Manual SNF Services
Links & Resources
True Freedom Home Health Plan – Enroll BEFORE you need it.
How does Medicare pay for #SkilledNursing Homes - 10153
Our Introductory You Tube VIDEO based on this manual
- Your costs for Skilled Nursing in Original Medicare You pay:
-
Days 1–20: $0 for each benefit period .
- Days 21–100: $194.50 coinsurance per day of each benefit period.
-
Days 101 and beyond: All costs. Medicare.gov *
-
- Clinical Guidelines explain the coverage so much better and in logical order!
- Medicare's VIDEO Nursing Home / Long-Term Care
- Planning for Discharge from a Health Care Setting VIDEO
- Long Term #Acute Care Publication # 11347
- Long-Term Acute Care Hospital (LTACH) Clinical Guidelines - Oscar
- Differences between Skilled Nursing, Long Term Acute Care & Inpatient Rehabilitation Facility
- Our FAQ on Sub Acute Care
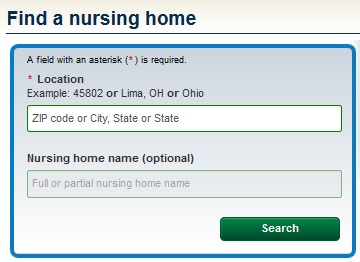
- Find & compare nursing homes, hospitals & other providers near you Medicare.Gov
- Learn more about providers
- Calculate Cost of Long Term Care in your Area Genworth
- "Hospital at Home" Programs Improve Outcomes, Lower Costs But Face Resistance from Providers and Payers
- Our Webpagse on Long Term Care
Blue Shield of California Authorized Agent - Broker
![]()
Medicare #Home health services
You can use your home health benefits under Part A and/or Part B to pay for home health services. Medicare covers medically necessary part-time or intermittent skilled nursing care, and/or physical therapy, speech-language pathology services, or continued occupational therapy services. A doctor, or certain health care professionals who work with a doctor, must see you face to-face before a doctor can certify that you need home health services. A doctor must order your care, and a Medicare-certified home health agency must provide it.
Home health services may also include medical social services, part-time or intermittent home health aide services, durable medical equipment, and medical supplies for use at home. You must be homebound, which means:
• You have trouble leaving your home without help (like using a cane, wheelchair, walker, or crutches; special transportation; or help from another person) because of an illness or injury.
• Leaving your home isn’t recommended because of your condition.
• You’re normally unable to leave your home because it’s a major effort.
You pay nothing for covered home health services. You pay 20% of the Medicare-approved amount, and the Part B deductible applies, for Medicare covered medical equipment. copied from Medicare & You – see brochure in side panel *
True #Freedom Home Health Plans
True Freedom Plan Details - Brochure
- Enrollment Form
- Be sure to add our Broker Information or email [email protected] the form to us
- Rate Chart
- VIDEO Explanation on True Freedom Plan
- The Long Road Ahead Video
- The application disclaimers
- FAQ's
- True Freedom website, but be sure to enroll with us!
"Prepaid Home Health Care?"
Watch 3 minute simple plain English Video
- Email us for more information [email protected]
- Our webpage on Long Term & Home Health Care
- Our webpage on True Freedom
$1.2 trillion infrastructure package
Build Back Better
November 6, 2021
The bill leaves out Biden’s proposal to spend $400 billion to bolster caregiving for aging and disabled Americans — the second largest measure in the American Jobs Plan.
His proposal would have expanded access to long-term care services under Medicaid, eliminating the wait list for hundreds of thousands of people. It would have provided more opportunity for people to receive care at home through community-based services or from family members.
It would also have improved the wages of home health workers, who now make approximately $12 an hour, and would have put in place an infrastructure to give caregiving workers the opportunity to join a union. CNN * Reuters * Wikipedia *
CA Dept of Aging – Home & Long Term Care ---
Please note, there are updates all the time, double check everything.
#Taking Care of Tomorrow
- Get Quote - Proposal for Long Term Care
- Borden Hamman Long Term Planning Guide
- California to Potentially Implement a Long-Term Care Payroll Tax
- Nolo Long Term Care
- Medi Cal IHSS In Home Support Services
- Here’s how those looking to ‘age in place’ can fund home health-care services
- Study: 70% Want To Age At Home, But Only 10% Have Long-Term Insurance
- In-Home Supportive Services 101: Opportunities and Challenges Under CalAIM
- Californians who need help paying for ’round-the-clock home care are stuck on a state waitlist
- Long Term Care.gov
- Calculate Cost of Long Term Care in your Area Genworth
our webpages on
- Medi-Cal Nursing Home, Long Term Care & Estate Recovery
- Home Health & Long Term Care
- Low Premium Home Health Care ONLY
- Hospice
- How Medicare covers Home Health Care
- Medicare & Skilled Nursing
- For Older Americans Month, questions about aging in place and staying at home
- 5 Wishes Talk to your loved ones today about what matters most. The advance care planning program trusted by more than 40 million people
- Facing Financial Ruin as Costs Soar for Elder Care
- VIDEO's
-
H. Long-Term Care
NAIC Shoppers Guide to Long Term Care
Flyer - Americans Unprepared for Future Health Care Expenses
Our Main Webpage on
Finding and #Choosing the right Nursing Home & Home Health Care for you or a loved one
- Medicare.Gov Nursing Home finder, guide & Compare This government provided tool also allows you to see what insurances and public benefits are accepted at the various facilities.
- Medi-Cal,
- Home Health Care Publication # 10969
- Private – Individual Long Term Care Coverage.
- Sunnyside Nursing & Post Acute Care – Torrance CA
- Veteran’s Home Health Care va.gov
- Veteran’s Care Co-Ordination.com
- Health Grades.com – they charge a fee
- Jewish Free Loan Assoc.
- Medicare.Gov Home Health Provider Finder
- Freedom from abuses Code of Federal Regulations (C.F.R.), 42 CFR 483.12
- Physician’s Report for Residential Care Facilities for the Elderly (RCFE) Preplacement Appraisal Information LIC 603 Identification and Emergency Information LIC 601 Senate Reviews Assisted Living Facility Problems 2.2014 CA Health Line
How to Find Home Health Care
-
Senior Living and Care Options
- New Life Styles.com
- Find & compare nursing homes, hospitals & other providers near you Medicare.Gov
- 24 hr cares.com Home Care Provider – owned by the son of a friend of ours
- modern health care.com/post-acute-care/nursing-home-care-broken-us-panel-reports 4.6.2022
Continuing Care Retirement Communities (CCRCs)
offer persons 60 years of age or older a long term continuing care contract that provides for independent living units, residential care/assisted living services, and skilled nursing care, usually in one location, and usually for a resident’s lifetime. Most CCRCs require a substantial entrance fee (e.g., from a low of $100,000 to over a million) to be paid by the applicant upon admission along with monthly fees. * CANHR.org *
- Continuing Care Retirement Community cdss.ca.gov
- How to choose a CCRCs CANHR
Medicare & #HomeHealth Care # 10969
TRUE FREEDOM - Home Health Care
No health questions asked

- Our webpage on Home Health & Long Term Care
- Medicare.Gov Home Health Provider Finder
- Resources to find Home Health & Nursing Care
- FAQ on Home Health Care Nurse - Medical Necessity - Wound Care
- The Medicare Home Health Benefit: An Unkept Promise
- Study Finds Medicare Advantage Patients Experience Worse Home Care Kff
Sub Acute Care vs Skilled Nursing #needed – Qualify for and the proper insurance plan.
Skilled Nursing Care Livanta the Medicare reviewer – appeals denied – Medical Necessity
excerpt of denial letter.
A review of the medical record shows that the patient was admitted to the skilled nursing facility after hospitalization for difficulty breathing and weakness.
The patient is now receiving skilled services for decreased functional mobility. The patient has made poor progress and is unable to walk, needing help for bed mobility and transfers. The patient needs moderate help for upper body dressing and totally dependent for lower body bathing, toileting and lower body dressing.
There is no documented evidence that continued skilled services are needed on a daily basis to maintain or prevent decline.
There are no documented medical issues to support the need for daily skilled nursing care.
FYI not that it applies here, but a 4.27.2022 HHS Office of the Inspector General report found that MAPD plans denied 13% of prior authorizations that would have been covered under original Medicare (Medi Gap, just follows what Medicare pays.)
“sub acute care” as opposed to SNF Skilled Nursing Facility
Subacute patients are medically fragile and require special services, such as inhalation therapy, tracheotomy care, intravenous tube feeding, and complex wound management care.
Adult subacute care is a level of care that is defined as comprehensive inpatient care designed for someone who has an acute illness, injury or exacerbation of a disease process.
Pediatric subacute care is a level of care needed by a person less than 21 years of age who uses a medical technology that compensates for the loss of a vital bodily function. DHCS Medi Cal *
Provider criteria for participation in the Subacute Care Program:
Licensed as an acute care hospital with a distinct part (DP), skilled nursing facility (SNF), or
Licensed as a freestanding (FS) SNF, and
Certified as a long term care Medicare and Medi-Cal provider, and
History of compliance with the DHCS Licensing and Certification program, and
Professional staff with the ability to provide care to subacute patients either by experience or demonstrated competence.
When a provider meets the criteria the DHCS enters into a contractual agreement to provide services to Medi-Cal subacute patients.
When a DP/FS SNF meets the criteria the DHCS enters into a contractual agreement, with the facility, to provide services to Medi-Cal subacute patients. DHCS Medi Cal *
Medi Cal sub acute care program, eligibility and treatment procedures
When you are ready to leave the hospital, you may need more medical care and rehab as part of the next step before you can go home. Your Cedars-Sinai care team may arrange for you to go to a sub-acute unit at a nursing facility while you are still healing and getting your strength back. Cedars Sinai *
Sub acute rehab (also called subacute rehabilitation or SAR) is complete inpatient care for someone suffering from an illness or injury. SAR is time-limited with the express purpose of improving functioning and discharging home.
SAR is typically provided in a licensed skilled nursing facility (SNF). SAR is typically paid for by Medicare or a Medicare Advantage program.
SAR provides help in two different areas:
Licensed physical, occupational and speech therapists provide therapy to increase your strength and functioning. For example, depending on what your need is, they might work to:
Increase your balance
Improve your safety when walking
Work to help you move your legs again after a stroke
Improve your independence with activities of daily living (ADLs)
Improve your cardio (heart) fitness after a heart attack
Licensed nursing staff provides medical care such as:
Wound management
Pain management
Respiratory care
Other nursing services that must be provided or supervised by an RN or LPN
SAR vs. Acute Rehab vs. Hospital
The terms used to talk about medical care and rehabilitation can be confusing at times. SAR is different from a hospital or an acute inpatient rehabilitation center.
A hospital, which is sometimes called “acute care,” is appropriate only for significant medical issues with the goal of a very short stay.
An acute rehab center is designed for high-level rehab needs, typically requiring more than three hours a day of physical, occupation, or speech therapy.
Sub acute rehab (SAR) centers are usually most appropriate for people who need less than three hours of therapy a day, thus the label of “sub acute,” which technically means under or less than acute rehab. Very Well.com * knollwood *
If we change plans by March 31 for MAOEP Medicare Advantage Open Enrollment Period, can we get a secondary or supplemental plan to pay for Long Term Care, Sub Acute Care or the $185 Skilled Nursing Co Pay?
Resources & Links
- Medicare Coverage for Skilled Nursing Publication 10153
- Home Health Care # 10969
- Excerpts from Typical MAPD policy on Skilled Nursing, Home Health,
- Insurance Companies need to make a profit and take in 20% more than they pay out in claims. Medical Loss Ratio and all.
- CA Department of Health Care Services — Sub acute Care
- In home supportive care Medi Cal – Medicaid
- Physical therapy Medicare Rules…
- Medicare Website Skilled Nursing SNF
- Our Webpage Medicare Skilled Nursing & Home Health Care
- Here’s our webpage on physical therapy
- See above for the Medicare Pamphlet & Video on Home Health Care
- Medi Cal Aged & Disabled Program
- Medi Cal IHSS In Home Supportive Services
- Appeals & IMR Independent Medical Review
- Requirements to qualify for Skilled Nursing Care
- Physical & Speech Therapy
- Requirements for Physical & Occupational Therapy
- nolo.com/medicare-coverage-inpatient-rehabilitation-stays
- Medicare.Gov MAPD Medicare Advantage Plans must cover all Medicare Services!
- Medicare Quality of Care Complaint Form
- Medi-Cal Medicaid Long Term and Nursing Home coverage – Estate Recovery
- Medi Cal Medicaid Share of Cost
- Risk Adjustment Fraud
- Livanta – Medicare Contractor to make sure MAPD meets Medicare guidelines
- Our webpage on Long Term Care
- Our webpage on Blue Shield Medicare Advantage
- Medical Necessity Clinical Guidelines and go step by step and show the evidence in the medical records that you need skilled nursing care and services on a daily basis to maintain or prevent decline?
- How about Medicare’s Home Health Care benefits? Can you get your doctor to write up a program of care that meets the Home Health Care guidelines?
- Medi Cal IHSS In Home Supportive Services?
- CA Department of Health Care Services — Sub acute Care
- In home supportive care Medi Cal – Medicaid
- Physical therapy Medicare Rules…
- Medicare Website Skilled Nursing SNF
- Our Webpage Medicare Skilled Nursing & Home Health Care
- Requirements to qualify for Skilled Nursing Care
- Physical & Speech Therapy
- Requirements for Physical & Occupational Therapy
- Medicare.Gov MAPD Medicare Advantage Plans must cover all Medicare Services!
- Medicare Quality of Care Complaint Form
- Medi-Cal Medicaid Long Term and Nursing Home coverage – Estate Recovery
- Medi Cal Medicaid Share of Cost
- Risk Adjustment Fraud
- Livanta – Medicare Contractor to make sure MAPD meets Medicare guidelines
- Our webpage on Long Term Care
- Our webpage on Blue Shield Medicare Advantage
- See the MAOEP Medicare Advantage Open Enrollment Period as opposed to AEP Annual Enrollment Period above on the rules and deadlines to change MAPD Plans, Rx Plans and/or go back to original medicare.
- Getting a Medi Gap plan is NOT guaranteed. Here’s our webpage on when Medi Gap is guaranteed. Maybe you qualify or can get in through passing underwriting?
- You can shop and compare Medicare Part D Rx and Medicare Advantage Plans with ALL companies nationwide here.
- If you go with California Blue Cross, United Health Care or Blue Shield please come back to us to enroll. We don’t get paid for providing this website. We only get compensated from the Insurance Company, at no additional cost to you when you enroll though us.
- FAQ on Medi Gap Coverage – Medicare Primary
- What is #Subacute Level of Care?
-
Sub acute rehab (also called subacute rehabilitation or SAR) is complete inpatient care for someone suffering from an illness or injury. SAR is time-limited with the express purpose of improving functioning and discharging home.1
SAR is typically provided in a licensed skilled nursing facility (SNF).
-
A hospital, which is sometimes called “acute care,” is appropriate only for significant medical issues with the goal of a very short stay.
An acute rehab center is designed for high-level rehab needs, typically requiring more than three hours a day of physical, occupation, or speech therapy
Sub acute rehab (SAR) centers are usually most appropriate for people who need less than three hours of therapy a day, thus the label of “sub acute,” which technically means under or less than acute rehab. Very Well.com *
-
- Subacute patients are medically fragile and require special services, such as inhalation therapy, tracheotomy care, intravenous tube feeding, and complex wound management care.
- Adult subacute care is a level of care that is defined as comprehensive inpatient care designed for someone who has an acute illness, injury or exacerbation of a disease process.
- Pediatric subacute care is a level of care needed by a person less than 21 years of age who uses a medical technology that compensates for the loss of a vital bodily function.
- There is some confusion, IMHO on if this is Hospitalization or Skilled Nursing dhcs.ca.gov * Cedars Sinai * Knollwood Nursing Center *
- Subacute care, or subacute rehabilitation (SAR) is care received inpatient when recovering from an injury or illness. The care is usually received in a skilled nursing facility (SNF). Medicare World *
- Review of the subacute care literature
- Which patients benefit from Subacute care?
- B. Subintensive Care Type Units.–Some hospitals have units which provide a level of care between other general routine and intensive care. These units are typically designated as subintensive, subacute, progressive, intermediate care units, etc. CMS.gov *
- Medicare Benefit Policy Manual Chapter 8 – Coverage of Extended Care (SNF) Services Under Hospital Insurance CMS.gov *
- Subacute level of Care in a Skilled Nursing Facility (SNF) under Medicare Part A
- OVERVIEW: Subacute nursing and rehabilitation services: services, furnished pursuant to physician orders, for members that are in a Skilled Nursing Facility and covered by Medicare Part A, that:• Require the skills of qualified technical or professional health personnel such as registered nurses, licensed practical nurses, physical therapists, occupational therapists, and speech-language pathologists or audiologists.
• Must be provided directly by or under the general supervision of these skilled nursing or skilled rehabilitation personnel to assure the safety of the patient and to achieve the medically desired result. and
• Require a short term, goal-oriented treatment plan including complex skilled nursing care and/or high intensity level skilled rehabilitation.NOTE: Subacute care is generally more intensive than traditional nursing facility care and less intense than acute care. Common Wealth Care * - Medical Necessity Guideline
Some examples of complex medical conditions that may require subacute skilled nursing or rehabilitative care:• Presence of serious injury or illness that requires inpatient treatment but not acute hospital care
• Ventilator Program
• Complex Respiratory Care and Treatments
• Specialized Infusion Therapy
• Brain Injury Rehabilitation
• High Intensity Stroke
• High Intensity Orthopedic Program
• Specialized Post-Surgical Recovery Programs
• Complex pain management Common Wealth Care *
-
Medicare #Appeals 11525
- AHA wants False Claims Act enforcement of Medicare Advantage care denials Modern Health Care 5.20.2022 See also Beckers Hospital Review
- False Claims Act - Whistle Blower.com

Filing an appeal with Medicare
- Official Medicare Advantage Plan Appeals VIDEO
- How to Appeal a Denial of your Health Claim - VIDEO Kantor & Kantor Attorneys
- Medicare Appeals – 11-22-22 CA Health Care Advocates Hi Cap
- See our webpage on
- Medicare Appeals & Grievances
- Fraud
- Attorneys - We don't know them... Found on Google
- Medicare Appeals & Grievances
- See our webpage on
Resources & Links
- Skilled nursing facility care coverage (Medicare.Gov)
- Get help paying for skilled nursing facility care
- Medi Cal IHSS In Home Services
- Medi Cal – Medically Needy – Share of Cost
- Medi Cal – Qualification & Estate Recovery
- Medi Cal has 90 day look back on claims from date you applied
- Our webpage on Home Health & Long Term Care
- 7 ADL’s Activities of Daily Living to trigger Long Term Care
- Veterans Administration?
- Find hospitals & skilled nursing facilities
- Booklet on this page to finding Nursing Homes
- medicare.gov/-skilled-nursing-facilities
- Pamphlet on Skilled Nursing from Medicare
- Hospice, Palliative & Respite Care
- Medicare Benefit Policy Manual Chapter 8 – Coverage of Extended Care (SNF) Services Under Hospital Insurance
- Social Security – Benefits for Surviving Spouse & Dependent Children
References, Links & Bibliography
- Coverage
- SNF Skilled Nursing Medicare.Gov
-
- Medicare.Gov Glossary
- Definitions
- Benefit Period
- CMS on Benefits Periods Official Detailed Manual
- Medicare Rights.org
- Medicare Interactive
-
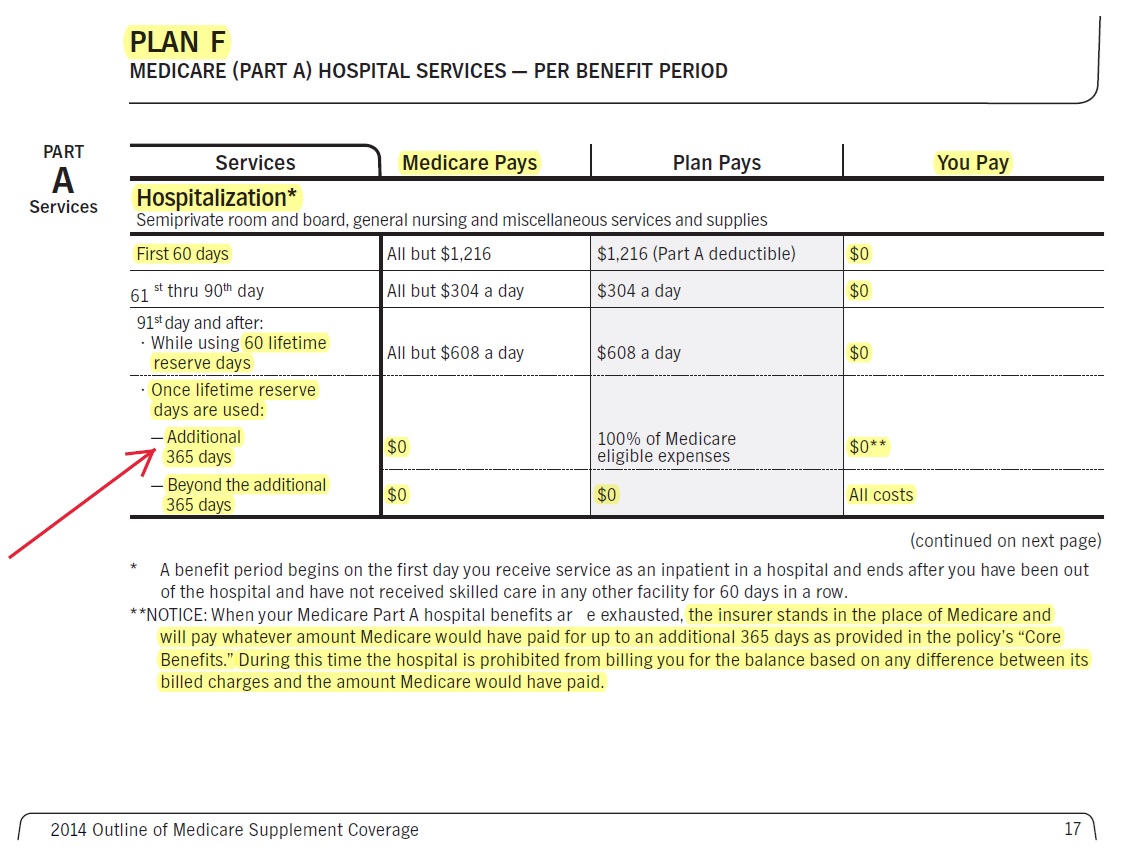
Benefit periods measure your use of inpatient hospital and skilled nursing facility (SNF) services. A benefit period begins the day you are admitted to a hospital as an inpatient, or to a SNF, and ends the day you have been out of the hospital or SNF for 60 days in a row. After you meet your deductible, Original Medicare pays in full for days 1 to 60 that you are in a hospital. For days 61-90, you pay a daily coinsurance.
If you have used your 90 days of hospital coverage but need to stay longer, Medicare covers up to 60 additional lifetime reserve days, for which you will pay a daily coinsurance. These days are nonrenewable, meaning you will not get them back when you become eligible for another benefit period.
Medicare will stop paying for your inpatient-related hospital costs (such as room and board) if you run out of days during your benefit period. To be eligible for a new benefit period, and additional days of inpatient coverage, you must remain out of the hospital or SNF for 60 days in a row. When you start a new benefit period, you will also have a new Part A deductible.
Note: Medigap policies A through N pay for your hospital coinsurance and provide up to an additional 365 lifetime reserve days. Additionally, Plans B through N pay some or all of your hospital deductible. Medicare Interactive
-
- Skilled Nursing over 100 days
- SNF Skilled Nursing past 100 days Medicare Interactive
- Lifetime Reserve Days
- Medicare Interactive from Medicare
- Additional 365 from Medi Gap – EOC Page 4 II A 1 c
- c) Upon exhaustion of the Medicare hospital inpatient coverage including the sixty (60) lifetime reserve days, coverage for the Medicare Part A Eligible Expenses for hospitalization will be paid at the appropriate standard of payment which has been approved by Medicare, subject to a lifetime maximum benefit of an additional 365 days (except that psychiatric care in a psychiatric hospital participating in the Medicare program is limited to 190 days during the Subscriber’s lifetime);
-
CA Insurance Code (b) With respect to the standards for basic (core) benefits for benefit plans A to J, inclusive, every issuer shall make available a policy or certificate including only the following basic “core” package of benefits to each prospective insured. An issuer may make available to prospective insureds any of the other Medicare supplement insurance benefit plans in addition to the basic core package, but not in lieu of it. However, the benefits described in paragraphs (6) and (7) shall not be offered so long as California is required to disallow these benefits for Medicare beneficiaries by the Centers for Medicare and Medicaid Services or other agent of the federal government under Section 1395ss of Title 42 of the United States Code.
-
(1) Coverage of Part A Medicare eligible expenses for hospitalization to the extent not covered by Medicare from the 61st day to the 90th day, inclusive, in any Medicare benefit period.
(2) Coverage of Part A Medicare eligible expenses incurred for hospitalization to the extent not covered by Medicare for each Medicare lifetime inpatient reserve day used.
(3) Upon exhaustion of the Medicare hospital inpatient coverage including the lifetime reserve days, coverage of 100 percent of the Medicare Part A eligible expenses for hospitalization paid at the appropriate Medicare standard of payment,
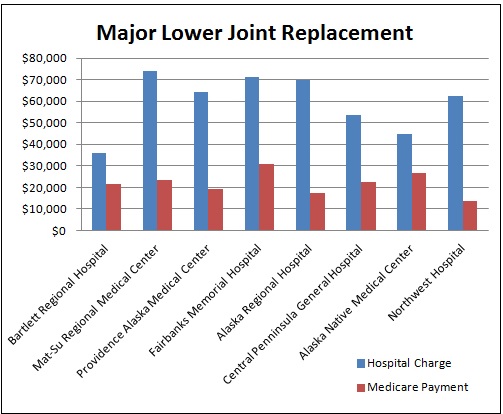
cms.gov/Physician Fee Schedule
health care value hub.org/medicare-rates-benchmark-too-little-or-just-right
AHA.org Fact Sheet
Kaiser Health News What A Hospital Charges Vs. What Medicare Payssubject to a lifetime maximum benefit of an additional 365 days. The provider shall accept the issuer’s payment as payment in full and may not bill the insured for any balance.
-
- (c) The following additional benefits shall be included in Medicare supplement benefit plans B to J, inclusive, only as provided by Section 10192.9.
-
(2) With respect to skilled nursing facility care, coverage for the actual billed charges up to the coinsurance amount from the 21st day to the 100th day, inclusive, in a Medicare benefit period for post hospital skilled nursing facility care eligible under Medicare Part A. CA Insurance Code 10192.8 b
-
- Law, Legal Codes & Clinical Guidelines
- CA Law on Medi Gap Policies
- Medicare General Information, Eligibility, and Entitlement
-
- Oscar (just for reference) Home Care – Skilled Nursing Care (RN, LVN/LPN) (CG020) English PDF
- Home Care – Physical Therapy (PT) and Occupational Therapy (OT) (CG021) English PDF
- Home Care – Home Health Aides (HHA) (CG022) English PDF
- Home Care – Speech Language Pathology (SLP) Services (CG023) English PDF
- Skilled Nursing Facility Care (CG042) English PDF
- Blue Shield Medical Policy List
- Medical Necessity
- Oscar (just for reference) Home Care – Skilled Nursing Care (RN, LVN/LPN) (CG020) English PDF
- Appoint us or someone else the authority to get confidential information from Blue Shield on your account
- Get a Blue Shield Member Portal
- Get ONLINE Account for Medicare & Social Security
How does Medi Gap Plan Hi F pay for Hospital Care, Long Term #Acute Hospital, Sub Acute Care, Skilled Nursing, Home Health Care?
What happens if you go over 90 days? How do 60 lifetime reserve days work? How do 365 additional from Medi Gap work?
Email us [email protected] for Source Brochure




Help!
I’ve been in the hospital, skilled nursing, etc. since November. Due to an infection my toes were amputated. I need physical therapy, skilled nursing, home health care, Medi Cal, IHSS, I don’t know what all.
What programs and guarantees are available to me.
I also have Blue Shield 65 Plus HMO, how is it better and differ from original Medicare?
Here’s the EOC Evidence of Coverage for Blue Shield 65 Plus
Please note that MAPD Medicare Advantage plus must give you equal or better benefits than original medicare!
Skilled Nursing
Note – Medicare is $185/day co-pay for days 21 to 100.
Home Health Care Agency
See the brochure above on Medicare eligibility and benefits of Home Health Care
See the Blue Shield EOC for their rules, details and appeals process. Try Ctrl – F to search.
Skilled Nursing not medically necessary
Do ObamaCare/ACA policies cover Skilled Nursing? How long?
Skilled Nursing Facility Benefits
Benefits are provided for Skilled Nursing services in a Skilled Nursing unit of a Hospital or a freestanding Skilled Nursing Facility, up to the Benefit maximum as shown on the Summary of Benefits.
The Benefit maximum is per Member per Benefit Period, except that room and board charges in excess of the facility’s established semi-private room rate are excluded.
A “Benefit Period” begins on the date the Member is admitted into the facility for Skilled Nursing services, and ends 60 days after being discharged and Skilled Nursing services are no longer being received.
A new Benefit Period can begin only after an existing Benefit Period ends Specimen Policy
Summary of Benefits
Skilled nursing facility (SNF) services Up to 100 days per member, per benefit period,