Prescription Drugs – Rx
How do I know if my Rx – Prescription is in the formulary – #Covered?
1st What is a Formulary – definition?
The formulary list of preferred Generic and Brand Drugs maintained by the Insurance Companies Pharmacy & Therapeutics Committee. It is designed to assist Physicians in prescribing Drugs that are Medical Necessary and cost-effective. The Formulary is updated periodically. Benefits are available for Formulary Drugs. Non-Formulary Drugs are covered when the Insurance Company or an external reviewer (see our appeals & grievances webpage) approves an exception request. EOC page 110 *
If you are eligible for Medicare Part D Rx, there is a shopping tool that searches all the plans! But, be sure to enroll in the link we give you, so that you get our assistance and consultation in the future.
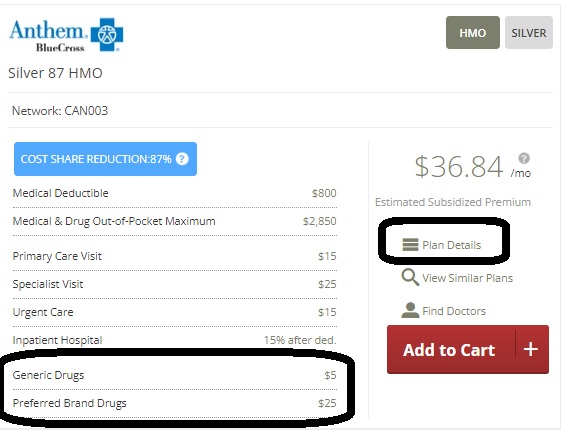
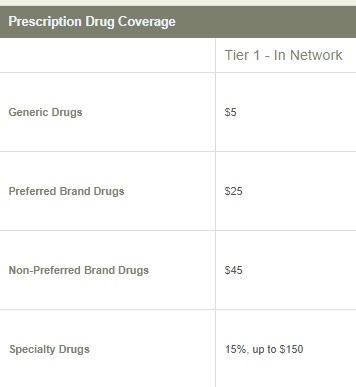
So, go back and check out the FREE quote, click on details, compare up to three plans and see what the co pay is for tier 4
Click on plan details to get more information.
I will grant you that this is a LOT of work.
We can’t stress this enough, the BEST way to find out what YOUR plan covers is in your EOC Evidence of Coverage.
2nd best is our website, 3rd is the one we link to, as it’s a popular plan in CA.
How to request a formulary #exception
- Check the EOC Evidence of Coverage. Here’s Blue Shield’s as an example procedure for Prior Authorization, exceptions & step therapy on page 71 of the EOC
- Oscar Pharmacy Clinical Guidelines (Medical Necessity) We are showing Oscar as IMHO their guidelines are easier to read.
- Some drugs, most Specialty Drugs, and prescriptions for Drugs exceeding specific quantity limits require prior authorization for Medical Necessity, as described in the Prior Authorization/Exception Request Process section. The Member or his/her Physician or Health Care Provider may request prior authorization
- How to get prior authorization is on page 27
- The Member, his/her Physician or Health Care Provider may request prior authorization by submitting supporting information
- For formulary exceptions, the prescriber’s supporting statement must indicate that the non-formulary drug is necessary for treating an enrollee’s condition because all covered drugs on any tier would not be as effective or would have adverse effects, the number of doses under a dose restriction has been or is likely to be less effective, or the alternative(s) listed on the formulary or required to be used in accordance with step therapy has(have) been or is(are) likely to be less effective or have adverse effects. CMS.gov
- Once all required supporting information is received, the Insurance Company will provide prior authorization approval or denial, based upon Medical Necessity, within two business days. Coverage requests for Non-Formulary Drugs in standard or normal circumstances will have a determination provided within two business days or 72 hours, whichever is earlier; the same requests in exigent circumstances will have a determination provided within 24 hours.
- Contacting your insurance company Check their EOC Evidence of Coverage., or the back of your ID card.
- If we are your appointed agent, no charge, we can help you do this, if you send us the supporting documents from your doctor.
- Holistic alternative for erectile dysfunction to Viagra?
AI Version of requesting formulary exception
- Get a prior authorization: Your doctor must start this process by submitting a request to your insurance plan with a letter of medical necessity and supporting documents.
- Ensure the prescription is for an approved use: The plan will likely only cover Ozempic if it’s prescribed for a condition that it’s FDA-approved to treat, such as Type 2 diabetes. Coverage for weight loss alone is generally not provided.
- Provide detailed medical records: Your doctor should include notes, labs (like A1C levels), and any measurements (like BMI) to support the request.
- Document failed treatments: If you have already tried other, less expensive diabetes medications and they didn’t work or caused side effects, your doctor should include the dates, duration, and outcomes of those trials in the request. [1, 2, 3, 5, 6, 8]
- Filing an appeal: You have the right to appeal the decision if your plan denies the prior authorization.
- Building a strong case: Gather all documentation showing why preferred medications are not a suitable option for your specific medical needs.
- Using clinical evidence: In your appeal, you can include clinical research that illustrates why Ozempic would be more effective for your condition than the alternatives your plan prefers. [2, 5, 9]
Definition of Status of Rx in Formulary List
| Status | Definition |
|---|---|
| Tier 1 | Most generic drugs and low-cost, preferred brand drugs |
| Tier 2 | Non-preferred generic drugs, preferred brand drugs, or drugs recommended by Blue Shield’s Pharmacy and Therapeutics (P&T) Committee based on drug safety, efficacy, and cost |
| Tier 3 | Non-preferred brand drugs, drugs recommended by Blue Shield’s P&T Committee based on safety, efficacy, and cost, or drugs that generally have a preferred and often less costly therapeutic alternative at a lower tier |
| Tier 4 | Drugs that are required by the Food and Drug Administration (FDA) or drug manufacturer to be distributed by specialty pharmacies, drugs that require training or clinical monitoring for self administration, drugs manufactured using biotechnology, or drugs with a plan cost (net of rebates) greater than $600 |
| Non-formulary |
Non-formulary Drugs not listed that meet the Tier 4 description require a formulary exception based on medical necessity to be covered at the Tier 4 share of cost. All other drugs not listed require a formulary exception based on medical necessity for coverage at Tier 3. |
Definition of Restrictions
| Restriction | Definition |
|---|---|
| Age Restriction | Prior authorization may be required if your age does not fall within the FDA, manufacturer, or treatment guideline recommendations. |
| Contraceptive drugs and devices |
Contraceptive drugs and devices covered at no charge. |
| Contraceptive drugs and devices | Contraceptive drugs and devices may be covered at no charge with prior authorization. |
| Gender Limit – Female Only |
Coverage is restricted to females. Prior authorization may be required if the FDA, manufacturer, or treatment guidelines do not recommend the drug for a gender. |
| Gender Limit – Male Only |
Coverage is restricted to males. Prior authorization may be required if the FDA, manufacturer, or treatment guidelines do not recommend the drug for a gender. |
| Limited Access |
Limited Access/Distribution Only available through select pharmacies that are designated by the manufacturer. |
| Limits/Notes | Coverage restrictions or limits for drugs. |
| Prior Authorization | Prior authorization is required to determine coverage |
| Quantity Limit | The prescription quantity covered is limited. Prior authorization is required for greater than the limit. |
| Retail & Mail Pharmacy Access | Tier 4 drugs available at retail and mail order pharmacy. |
| Short Cycle Drug | Short Cycle DrugInitial prescriptions for select Specialty Drugs can be dispensed for a 15 day trial supply. The applicable Copayment or Coinsurance will be pro-rated. |
| Specialty Pharmacy | Must be obtained through a network specialty pharmacy. |
| Step Therapy | Coverage is determined based on use of other first-line therapies/drugs. Copied from BS Website |
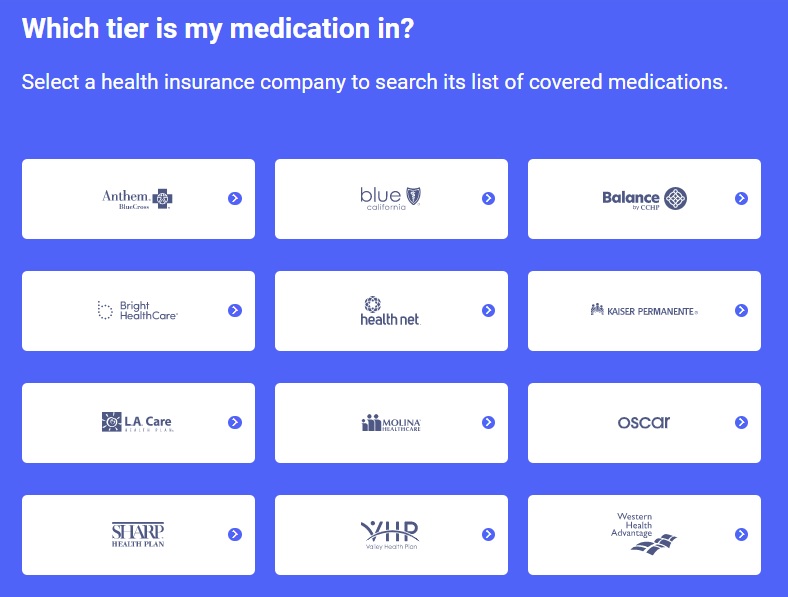
Here’s the links to check All the plans in the Individual Market.
How to check the Formulary list.
Let’s not reinvent the wheel, here’s where I did extensive research in April 2022 on how to search Kaiser’s Employer Small Group formulary with VIDEO’s and everything.
Formulary research is one BIG reason not to wait till the last minute to shop plans. If one were to pick a plan at the beginning of Open Enrollment or special enrollment, they have 30 days FREE look, where one could cancel and still have time to pick a NEW plan!
So, just list each Rx in the search box. Then use Ctrl F if appropriate How to use Ctrl F if it’s pdf * VIDEO
- Jump to section on:
- Rx Covered?
- Request Formulary Exception
- Pain Management
- Ultra Expensive Rx
- Latuda
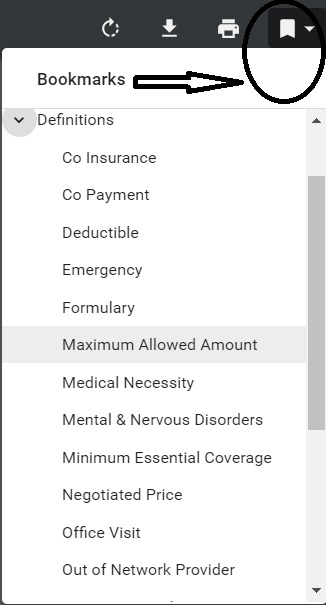
Specimen Individual Policy #EOC with Definitions
Employer Group Sample Policy
It's often so much easier and simpler to just read your Evidence of Coverage EOC-policy, then look all over for the codes, laws, regulations etc! Plus, EOC's are mandated to be written in PLAIN ENGLISH!
- Find your own Individual EOC Evidence of Coverage
- It' important to use YOUR EOC not just stuff in general!
- Obligation to READ your EOC
- Plain Meaning Rule - Plain Writing Act
- Our Webpage on Evidence of Coverage
- OOP Out of Pocket Maximum - Many definitions are explained there.
VIDEO Steve Explains how to read EOC
Mandated Essential Benefit – ACA/Obamacare
Prescription Drugs – Rx are an essential mandatory benefit of Health Care Reform
Prescription drug benefits.
CFR Code of Federal Regulations §156.122
(a) A health plan does not provide essential health benefits unless it:
(1) Subject to the exception in paragraph (b) of this section, covers at least the greater of:
(i) One drug in every United States Pharmacopeia (USP) category and class; or
(ii) The same number of prescription drugs in each category and class as the EHB-benchmark plan;
California Benchmark Plans
♦ Kaiser HMO 30 (1 Page), ♦ 2 Page, ♦ all plans brochure (30 Pages), ♦ Evidence of Coverage 64 pages
and
(2) Submits its drug list to the Exchange, the State, or OPM.
blueshieldca.com/Standard_Formulary.pdf
(b) A health plan does not fail to provide EHB prescription drug benefits solely because it does not offer drugs approved by the Food and Drug Administration as a service described in §156.280(d) of this subchapter.
(c) A health plan providing essential health benefits must have procedures in place that allow an enrollee to request and gain access to clinically appropriate drugs [medically necessary?] not covered by the health plan.
Please have your MD contact BS to convince them the brand name is the only thing that will work.
800. 535.9481
Fax 888.697.8122
♦ blueshieldca.com/drug-prior-authorization
♦ blueshieldca.com/exceptions-appeals
Procedures shown in “Blue Cross” specimen policy.
Be sure to take your Rx the way your doctor, pharmacist and Rx manufacturer suggest.
Visit Our webpage on Medical Necessity
Holistic alternative for erectile dysfunction to Viagra?
Guaranteed Issue under ACA/Obama Care
All our Health plans are Guaranteed Issue with No Pre X Clause
Quote & Subsidy #Calculation
There is No charge for our complementary services, we are paid by the Insurance Company.
- We are authorized Brokers for Dental, Vision & Covered CA get instant quotes direct and in Covered CA with subsidy calculation for:
Watch our 10 minute VIDEO
that explains everything about getting a quote
-
- Our Quote Engine Takes all the complexity out of using pencil and paper to figure out the premiums per the Obamacare/ACA rules under CFR §1.36B-3 *
#GoodRx
We do not know who they are. We are not endorsing them. We’ve heard from some of our clients, who are happy with them.
- GoodRx said Wednesday its dispute last year with Kroger continues to affect its bottom line.The company reported a first-quarter net loss of $3.3 million, or 1 cent per share, compared with net income of $12.3 million, or 3 cents per share, a year ago. Quarterly revenue totaled $184 million, down 10%. The company’s biggest revenue driver, its prescription transaction business, saw a 13% decline, to $155.5 million this year from $134.9 million in 2022.GoodRx blamed the decline in the prescription transaction business on its contract dispute last year with Kroger, the national grocery chain that temporarily stopped accepting Good Rx’s discounts at the point of sale in May 2022. The company also blamed the Kroger issue for a 5% decrease in monthly active customers from 6.4 million in 2022 to 6.1 million this year. Modern Health Care *
- Los Angeles Times 9.17.2020 Good Rx going IPO - They can make $$$ since the Rx pricing system is so crazy!
- Times Rx.com
- On the other hand...
- Needy Meds.org
Pain Management
#Pain Management, Opioid Crisis, Physical Therapy, etc.
- Dr. Oz: How to Treat Chronic Pain Without Drugs
- Breakthrough in the Relief of Chronic Pain Without Drugs!
- Stopping Pain without Rx
- We’re Experiencing a Crisis in Pain Management. Can We Treat It Without Drugs?
- How You Can Manage Your Pain Without Medications With OMT, Acupuncture and an Anti-Inflammatory Diet
Understanding your alternatives - How Can You Relieve Chronic Pain — Without Drugs?
Cognitive behavioral therapy helps guide thoughts, actions - Drug-Free Remedies for Chronic Pain
Escape from pain — without drugs - 8 Proven Ways to Manage Chronic Pain Without Medication
- How to Treat Your Pain Without Drugs
- 8 Surprising (And Natural) Ways To Beat Pain
When it comes to your chronic aches and pains, the new gold standards aren’t what you think - Management of Pain without Medications
- Is it possible to manage pain well without opioids?
- institute for chronicpain.org
- Pain Management Without Drugs
- 11 Tips for Living With Chronic Pain
- practical pain management.com
- Musculoskeletal Health
- Pain Management
- Back Pain
- Arthritis
- The Ache of Arthritis
- Take a tip from the Tin Man
- Anti-Arthritis Diet
- Guide to Posture in the Workplace
- Setting Up Your Workstation
- Repetitive Motion Injury Prevention
- Your Office Workout
- Poster: Keep Motion Injuries at Bay
Mind over Matter
Stress – Seeing a Psychiatrists, Shrink or Therapist
The Ten Biggest Mistakes Psychiatrists Make
6. Don’t refer to therapy.
Psychopharmacology without therapy is treating an infection with Tylenol.
Medications do not cure a psychiatric disease; we’re not even sure what the disease actually is. What they can do is reduce symptoms, give you strength—so that you can learn new behaviors. That’s the point of medications. Treating depression with an antidepressant is not the solution; it’s the preliminary step in allowing you to figure out how to handle depression later on. The adaptation, the adjustment, the physical altering of brain functioning is done by new learning, often this is therapy (though it doesn’t have to be.) I’m not saying therapy is that great, or necessary, either. I’m simply saying that trying to improve a person’s long term status using medications alone without some sort of education and training is a waste of time. It is maybe the most profound disservice of all to tell a patient that their depressive or bipolar symptoms are the result of biology or chemical imbalances and thus absolve them of the responsibility of learning new ways of interpreting and coping with their environment.
8. Polypharmacy
Polypharmacy isn’t just common– it’s the codified standard. When two psychiatrists discuss a patient, inevitably one of them will say these four words: “You should consider adding…” The Last Psychiatrist.com *
- 10 Ways Depression and Anxiety Can Cause Physical Pain
- Can Mental Illness Cause Physical Pain?
- There are indeed mental illnesses that can cause people to experience pain, numbness and a variety of other “physical” symptoms. They are known as Somatoform Disorders.
- Somatic Symptom and Related Disorders Web MD
- New Test Distinguishes Physical From Emotional Pain in Brain for First Time
- 13 Ways That Emotional Pain Is Worse Than Physical Pain
- Is There Such a Thing as Psychological Pain? and Why It Matters National Institute of Health
- The Link Between Depression and Physical Symptoms
- How Emotional Pain Affects Your Body
- Emotional and Physical Pain Activate Similar Brain Regions
Where does emotion hurt in the body? - 5 Ways Emotional Pain Is Worse Than Physical Pain
Why emotional pain causes longer lasting damage to our lives - 8 Physical Symptoms That Prove Depression Is Not Just ‘In Your Head’
We don’t often pair depression with physical pain but research shows this mental illness can really hurt.
Rx – Prescriptions for Pain
- Lumbar Epidural Injections
Therapeutic and Diagnostics Benefits for Low Back Pain - Radiculopathy John Hopkins
- Wikipedia
- Visit our webpage on the clinical guidelines for Rx Medication
Physical Therapy & Exercise
Exercises for the Fifth Lumbar
Rx Drug Abuse
- The Opioid Crisis in America and How Employers Can Help
Medicare Provider Finder https://www.medicare.gov/physiciancompare/
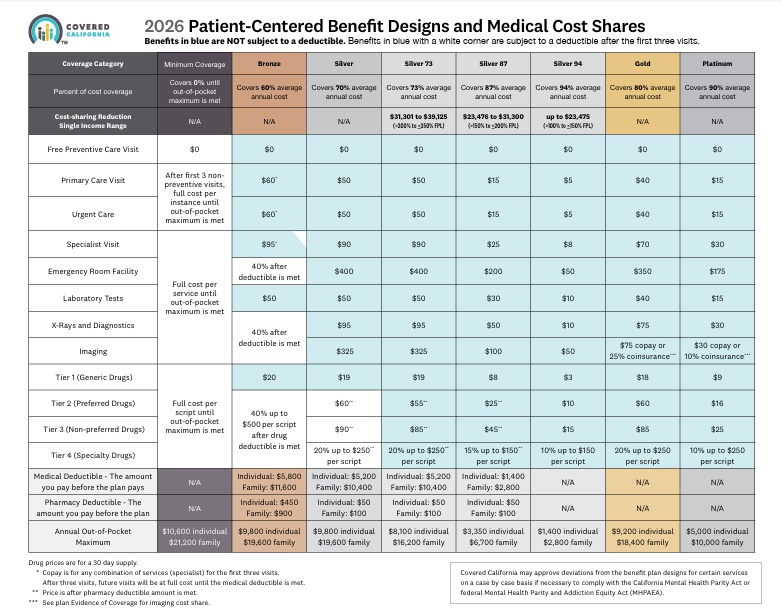
- 2026 Covered California 2026 Patient-Centered Benefit Plan Designs Final Approval 7/28/2025
- Get Instant Quotes & Subsidy Calculation
- Covered CA bulletin on new and improved Enhanced Silver CSR Cost Sharing Reduction
- Do you think your medical bills will be higher or lower than average for your age & zip code?
- Expected Payout (AV)
- MLR Medical Loss Ratio
- Bronze 60%
- Out-of-Pocket Pain From High-Deductible Plans Means Skimping on Care Kff 12/2025 *
- Enhanced Silver 70% - 94% Gold 80% Platinum 90%
- Metal Levels are based on Expected Claims Payment - that is the actuarial value (AV).
- Renewal Tool Kit
- Patients often can’t afford to pay off what their insurance leaves behind
- This is one way Health Care Reform hopes to make shopping and comparing Instantly - easier. So, if you get a lower priced plan with less or fewer benefits, co-pays, deductibles you simply pay more when you have a claim. Don't worry, there is a stop loss - maximum out of pocket OOP, of say $7k so that you won't break the bank.
- Lessons from the ACA: Simplifying Choices to Optimize Health Coverage 12/2025 Commonwealth Fund *
- All plans cover the 10 Federal essential benefits and CA mandated benefits.
- Team Trump’s Answer to Ballooning Obamacare Premiums: Less Generous Coverage KFF.org *
- Our main webpage on Metal Levels
FAQ’s
See historical and archives at archive.org
Resources, Bibliography & Links
- CA Senate Bill SB 853 Wiener 2022 would require state-regulated insurance companies to cover a denied prescription while the patient appeals the decision if a patient has previously taken the drug Read More KHN.org
- New drugs come with high price tag, research finds
- FTC to Investigate CVS Caremark and Other Pharmacy-Benefit Managers
Inquiry will examine what impact their businesses have on cost and access to prescription drugs - Median Launch Price For A New Drug Was $2,115 In 2008. In 2021? $180K
- New drug prices soar to $180,000 a year on 20% annual inflation
- Industry middlemen driving up prices of generic drug prescriptions as much as 20 percent: research
- Legislative leaders to scrutinize state health insurance plan, pharmacy benefit managers
Parent, Child & Related Pages